|
|
  |
 |
  |
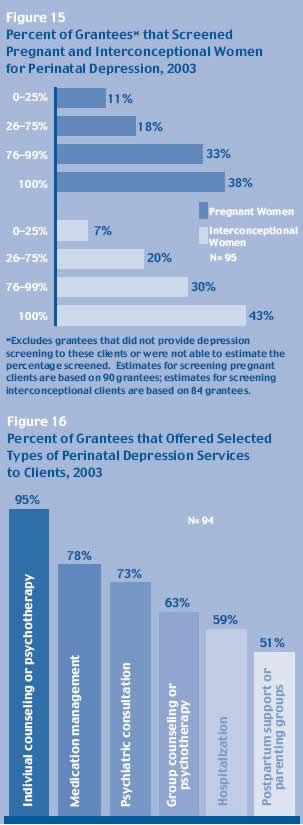
PERINATAL DEPRESSION SERVICES
| Screening for perinatal depression
became a required component in the third
funding cycle of Healthy Start. The recent
focus on perinatal depression is in response
to increasing evidence that links depression
and stress to adverse pregnancy outcomes.
Maternal depression can lead to poor self-care
and poor infant care, and in extreme cases,
to suicide or infant death. With early
detection and intervention, depression
can be treated and functioning improved.
During 2003, all but one grantee provided
perinatal depression services; the remaining
grantee reported that services were under
development. By far, the most commonly
used screening tool was the Edinburgh
Postnatal Depression Scale (EPDS) (used
by 67 percent of grantees). More than
two-thirds of the grantees reported that
they screened at least three-fourths of
their clients for depression. A sizable
proportion of grantees reported that they
achieved universal screening - that is,
they screened all of their pregnant and
interconceptional clients for depression
(38 percent and 43 percent, respectively).
Several factors were associated with
achieving universal depression screening
of pregnant clients. Universal screening
rates were higher among grantees that
performed screening both separately and
as part of a comprehensive screening (58
percent) compared to those that performed
screening either separately (39 percent)
or as part of a comprehensive screening
(28 percent) (data not shown). Projects
that screened at more points in time also
were more likely to screen all their clients,
suggesting that repeated screening attempts
may reduce barriers and resistance to
screening. Universal screening rates increased
from 27 percent among grantees using only
one screening interval, to 48 percent
of those using four intervals, and 100
percent of those using five intervals.
Grantees that involved direct employees
or subcontractors in clinical assessment
and diagnosis (49 percent) had higher
universal screening rates compared to
those that relied only on referrals (26
percent), suggesting that more monitoring
and follow-up is required by grantees
that use referrals.
When Healthy Start clients screen positive
for depression, they require additional
clinical assessments to confirm a mental
health diagnosis and determine the necessary
follow-up services. These subsequent clinical
assessments can be provided by project
staff or subcontractors, or through outside
referrals, and by either specialty mental
health providers or primary care providers.
All of the grantees (100 percent) reported
that further clinical assessment and diagnosis
were available in their communities, and
most (93 percent) indicated that these
services were available from mental health
providers, either alone or in combination
with primary care providers. |
 [D] [D]
|
Specifically, 53 percent of grantees indicated
that assessment and diagnosis services were
provided by specialty mental health providers
only; another 39 percent relied on both specialty
mental health and primary care providers; while
the remaining seven percent involved only primary
care providers. However, grantees in rural areas
(80 percent) were significantly less likely
than urban grantees (95 percent) or urban/rural
grantees (100 percent) to report that specialty
mental health providers performed the follow-up
assessments.
Forty-eight percent of the grantees offered
additional clinical assessments through providers
employed directly by or under subcontract to
the Healthy Start grantee, while 52 percent
provided these services through referrals outside
of Healthy Start (data not shown). The larger
projects (with total 4 year funding of $4 million
or more for the 2001 - 2005 cycle) were significantly
more likely to use direct employees or subcontractors
to provide assessments (69 percent), while projects
with lower funding levels were more likely to
provide these services through referrals (62
percent to 68 percent). In addition, grantees
in urban areas (57 percent) were more likely
than rural (35 percent) or urban/rural (25 percent)
grantees to use direct employees or subcontractors
to provide clinical assessments.
Grantees reported that a wide range of services
were available to those requiring treatment,
with individual counseling or psychotherapy
(95 percent) the most common and postpartum
support or parenting groups (51percent) the
least common (data not shown). Nearly one-third
of grantees (31 percent) reported that all six
types of services were available in their communities.
next page: Barriers
to Care
 |