How Is Peripheral Arterial Disease Diagnosed?
Peripheral arterial disease (P.A.D.) is diagnosed
based on your medical and family histories, a physical exam, and results from
tests.
P.A.D. often is diagnosed after symptoms are
reported. An accurate diagnosis is important, because people who have P.A.D.
are at increased risk for
coronary
artery disease (CAD),
heart
attack,
stroke, and
transient ischemic attack (“mini-stroke”). If you
have P.A.D., your doctor also may want to look for signs of these
conditions.
Specialists Involved
Primary care doctors, such as internists and family
practitioners, may treat people who have mild P.A.D. For more advanced P.A.D.,
a vascular specialist may be involved. This is a doctor who specializes in
treating blood vessel problems.
A cardiologist also may be involved in treating
people who have P.A.D. Cardiologists treat heart problems, such as CAD and
heart attack, which often affect people who have P.A.D.
Medical and Family Histories
To learn about your medical and family histories,
your doctor may ask:
- Whether you have any
risk
factors for P.A.D.
- About your symptoms, including any symptoms that
occur when walking, exercising, sitting, standing, or climbing
- About your diet
- About any medicines you take, including
prescription and over-the-counter medicines
- Whether anyone in your family has a history of
cardiovascular disease
Physical Exam
During the physical exam, your doctor will look for
signs and symptoms of P.A.D. He or she may check the blood flow in your legs or
feet to see whether you have weak or absent pulses.
Your doctor also may check the pulses in your leg
arteries for an abnormal whooshing sound called a bruit (broo-E). He or she can
hear this sound with a stethoscope. A bruit may be a warning sign of a narrowed
or blocked section of artery.
During the physical exam, your doctor may compare
blood pressure between your limbs to see whether the pressure is lower in the
affected limb.
He or she also may check for poor wound healing or
any changes in your hair, skin, or nails that may be signs of P.A.D.
Diagnostic Tests
Ankle-Brachial Index
A simple test called an ankle-brachial index (ABI)
is often used to diagnose P.A.D. The ABI compares blood pressure in your ankle
to blood pressure in your arm. This test shows how well blood is flowing in
your limbs. ABI can show whether P.A.D. is affecting your limbs, but it
won’t show which blood vessels are narrowed or blocked.
A normal ABI result is 1.0 or greater (with a range
of 0.90 to 1.30). The test takes about 10 to 15 minutes to measure both arms
and both ankles. This test may be done yearly to see whether P.A.D. is getting
worse.
Ankle-Brachial Index
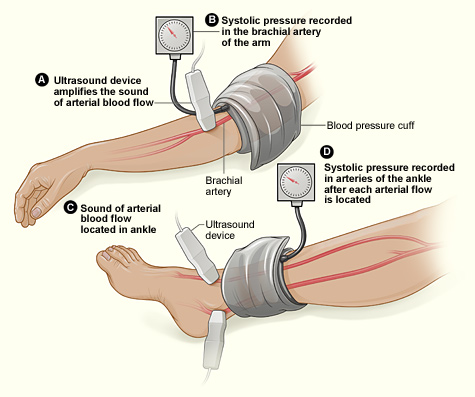
The illustration shows the ABI test.
The ABI compares blood pressure in the ankle to blood pressure in the arm. As
the cuff deflates, the blood pressure in the arteries is recorded.
Doppler Ultrasound
A Doppler ultrasound is a test that uses sound waves
to show whether a blood vessel is blocked. This test uses a blood pressure cuff
and special device to measure blood flow in the veins and arteries of the
limbs. A Doppler ultrasound can help find out how severe P.A.D. is.
Treadmill Test
A treadmill test can show how severe your symptoms
are and what level of exercise brings them on. For this test, you walk on a
treadmill. This shows whether you have any problems during normal walking.
You may have an ABI test done before and after the
treadmill test. This will help compare blood flow in your arms and legs before
and after exercise.
Magnetic Resonance Angiogram
A magnetic resonance angiogram (MRA) uses magnetic
and radio wave energy to take pictures of blood vessels inside your body. An
MRA is a type of
magnetic resonance imaging (MRI).
An MRA can find the location of a blocked blood
vessel and show how severe the blockage is.
If you have a
pacemaker,
man-made joint,
stent,
surgical clips, mechanical heart valve, or other metallic devices in your body,
you might not be able to have an MRA. Ask your doctor whether an MRA is an
option for you.
Arteriogram
An arteriogram provides a "road map" of the
arteries. It’s used to find the exact location of a blocked artery.
For this test, dye is injected through a needle or
catheter (tube) into an artery. This may make you feel mildly flushed. After
the dye is injected, an x ray is taken. The pictures from the x ray can show
the location, type, and extent of the blockage in the artery.
Some hospitals use a newer method of arteriogram
that uses tiny ultrasound cameras that take pictures of the insides of the
blood vessels. This method is called intravascular ultrasound.
Blood Tests
Your doctor may recommend
blood
tests to check for P.A.D. risk factors. For example, you may get a blood
test to check for
diabetes. You may also get a blood test to check your
cholesterol levels. |