|
II. Key Content Areas for the
Workshops
While each workshop was customized to
meet the needs of the individual States,
in fact, some
standardized subject areas were covered
by the workshops on issues ranging from
Medicaid,
SCHIP, managed care contracting, and their
relationship to maternal and child health
programs.
Each of the trainings was a mixture of
didactic presentations by the facilitators,
discussions led
by the facilitators, and group problem
solving. The pages that follow in this
section contain the
standardized information that was transmitted
at the workshops. See the Appendices for
the
background information specific to each
of the States visited.
Medicaid and SCHIP Policies to
Improve Child and Family Health
-
Medicaid is a leading purchaser of pediatric
care. It is a source of coverage for
one out of
every five U.S. children, including
more than one-third of births. Seen
in another light, the
program covers 60 percent of poor children
younger than 18 and nearly half of births
to low
income women.
-
Children need coverage and benefits
tailored to their unique needs and designed
to foster
their health, growth, and development.
Medicaid’s Early and Periodic
Screening, Diagnosis,
and Treatment (EPSDT) package of benefits
and services are specifically designed
to fit with
pediatric clinical standards and children’s
health needs.
-
With Medicaid, poor children's access
to health care is similar to that of
non-poor, privately
insured children.
-
Millions of uninsured children are eligible
for, but not enrolled in, publicly financed
health
coverage through Medicaid or SCHIP.
Effective outreach and enrollment can
make a
difference in coverage levels.
-
Children are half of all Medicaid enrollees,
but represent only 16 percent of the
total program
spending primarily because they use
less expensive, primary and preventive
services. The
average per capita Medicaid cost for
a child is approximately $1,150, compared
to more than
$10,000 per elderly enrollee.
-
In more than half of the States, Medicaid
has been used to expand health coverage
beyond
traditional groups. Under current Federal
law, Medicaid can be used to cover millions
more
children and their parents.
-
SCHIP offers no individual legal entitlement
to a federally defined benefit. In the
35 States
that maintain separately administered
SCHIP programs, child health benefits
vary. States are
obligated to use their funds to purchase
coverage known as “child health
assistance,” making
separately administered SCHIP plans
a form of premium support, with broad
discretion given
to contracting health plans.
Managed Care and Children
An increasing number of children receive
health coverage and services through Medicaid
or
SCHIP managed care arrangements.
- Overall,
more than half of all Medicaid beneficiaries
are enrolled in some form of managed
care in all States and the District
of Columbia, except Alaska and Wyoming.
- Children
are the group in Medicaid most likely
to be required to enroll in managed
care.
Children are more likely than beneficiary
groups such as the elderly, pregnant
women, adults
with disabilities to be included in
mandatory managed care enrollment rules
under Medicaid.
-
In 1998, more than half (55 percent)
of Medicaid beneficiaries enrolled in
managed care
were children under age 21. Many SCHIP
eligible children are enrolled -- on
a voluntary or
mandatory basis -- in managed care arrangements.
- Children
in Medicaid SCHIP plans are entitled
to the same benefits and protections
as
children in regular Medicaid plans.
- Among
26 States using separate, non-Medicaid
SCHIP and comprehensive managed care
in
2000, 11 States integrate the SCHIP
managed care contract with the Medicaid
contract.1
The promise of managed care is that it
can reduce costs to purchasers while improving
health
outcomes for the insured individual. Managed
care organizations (MCOs) seek to fulfill
this
promise through three basic mechanisms:
organizing provider relationships, limiting
what will be
covered, and controlling enrollee access
to services. Controls on access to service
generally are
aimed at high-cost and unnecessary services
(e.g., some elective surgery, and emergency
department use for routine care).2
In theory, MCOs also will seek to ensure
necessary care,
which can help enrollees remain healthy
and reduce long-term costs. In practice,
MCOs’ limits
on care are more frequent than promotions
for utilization of health services, primarily
because
they have greater incentives to reduce
short-term than long-term costs. For children,
such
emphasis on short-term results is a disadvantage.
Improving Child Health Access
and Outcomes through Effective Managed
Care
Contracting
Managed care arrangements are defined
in contracts between the purchaser and
the MCO, as
well as between the managed care organization
and its network providers. The contract
between
the MCO and the purchaser – in this
case the State Medicaid or SCHIP Agency
– sets the
boundaries on what services will be delivered,
when, and how. As use of managed care
has
increased, contracts have become an increasingly
important part of the legal and regulatory
framework under which children and families
receive health care. (See Figure A).
Solid managed care contracts are based
on negotiation and an agreement that reflects
“a meeting
of the minds.” Success depends on
clearly defining the terms of the contract,
specifying the
performance objectives and measures, and
using multiple enforcement tools with
varying levels
of severity. When State governments are
the purchasers, contracts also should
specify the nature
of the agreements and interactions expected
between MCOs and various public programs
(e.g.,
local health departments, WIC Supplemental
Food Program sites).

[D]
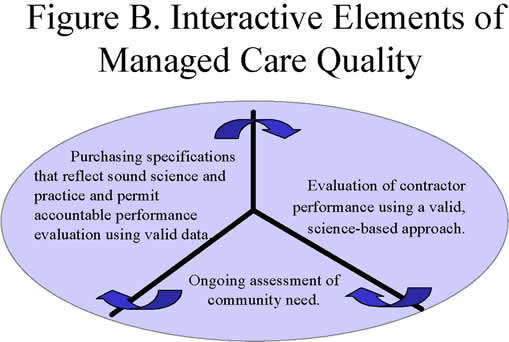
Managed care contracts are a particularly
useful tool for States to use in efforts
to improve health
care quality. (See Figure B.) State Medicaid
or SCHIP Agencies cannot overcome certain
systemic barriers to effective pediatric
preventive care, such as constraints on
access to care,
inadequate provider training and practice,
or deficits in parental knowledge and
parenting skills.
States can, however, set out expectations
for quality and, in turn, monitor quality,
pay for
performance, or penalize those who do
not perform.
Managed care contracts represent a unified
policy Statement by the State and are
the principal
means to create legally binding agreements
with managed care organizations (MCOs).
Contracts,
and the negotiations around contracts,
are the means for working out some very
specific
challenges in the delivery system. Furthermore,
if a benefit, quality standard, or other
expectation is not in the contract, MCOs
and their providers cannot be expected
to meet the
State’s expectations. Contracts
are also useful for policy makers, as
a means to express
priorities. If the State’s contract
development process is inclusive, it creates
inter- and intradepartmental
communication about the inter-relationship
of categorical and entitlement
programs. Such processes force categorical
programs to think about adapting their
programs to
an evolving health care delivery and financing
system. Finally, well-expressed contracts
set the
framework for communication with beneficiaries
(covered persons), including what should
be
contained in enrollment materials, how
people can engage in grievance processes,
and what
protections exist for those involuntarily
disenrolled.
[D]
Managed Care Contracts and Child
Health
A series of analyses of States’
Medicaid managed care contracts by GWU
researchers 3
found that such contracts express a vision
of health care and the health care system,
not
merely health coverage. As State Medicaid
Agencies become more sophisticated health
care purchasers, contracts have become
larger and more complex. Increasingly,
States include
detailed specifications that emphasize
the structure and process of care. Contracts
are
generally comprehensive and specific in
the areas of networks, access, service
delivery,
quality improvement, data collection and
reporting, consumer protections, and provider
payments. At the same time, States continue
to make fairly limited use of provisions
regarding
resolution of conflicting treatment decisions
in the case of contractors and agencies
responsible
for the same member. Detailed analysis
of contract provisions on pediatric care
found that State Medicaid
managed care contracts generally have:
-
Merged coverage and care into comprehensive
specifications that give attention to
pediatric care delivery -- not just
coverage.
-
Increased specificity regarding services
for special populations, such as children
with
special health care needs.
-
Attempted to close the gap between Federal
requirements and State contracts.
-
Not often met the challenge of incorporating
the broad EPSDT benefits into contracts,
despite greater attention to child health.
-
Specified the inclusion of "pediatric
providers" in the managed care
network.4
Table
1. Pediatric Purchasing Specifications:
Table of Contents
Part I Items and Services Covered
101- Medicaid Items and Services
101-A. Coverage Determination Standards
and Procedures
101-B. Delivery of Covered Items and
Services
102- EPSDT
103- Prescription Drugs
104- Family Planning Services and
Supplies
105- Medicaid Items and Services Not
Covered
106- Dental Services
107- STD Services
108- HIV Services
109- TB Services
110- Childhood Lead Poisoning Services
111- Diabetes Services
Part 2 Enrollment and Disenrollment
Part 3 Information for New and Potential
Enrolled Children
Part 4 Provider Selection and Assignment
Part 5 Provider Network
Part 6 Access Standards
Part 7 Relationships with Other State
and Local Agencies
Part 8 Quality Measurement and Improvement
Part 9 Data Collection and Reporting
Part 10 Enrolled Child Safeguards
Part 11 Vaccines for Children Program
Part 12 Remedies for Noncompliance
Part 13 Other Applicable Federal and
State Requirements
Part 14 Definitions |
Pediatric Purchasing Specifications
GWU has prepared purchasing specifications
to assist State agencies, private purchasers,
and
others interested in improving managed
care contract provisions. The Medicaid
Pediatric
Purchasing Specifications include numerous
provisions addressing a wide range of
issues for
Medicaid-eligible children and adolescents.
The purchasing specifications are based
on an understanding of existing contract
provisions
(such as those in the Medicaid managed
care contract database), as well as review
by Federal and
State government agencies, issue content
experts, and consumer advocates.
The GWU Pediatric Purchasing Specifications
are not official government policies and
do not
define a right and a wrong way to set
up contracts. They do provide advice on
how to construct
contract provisions so that they accurately
and precisely reflect the intentions and
expectations of
those who purchase managed care coverage.
They give options and alternatives based
on legal or
clinical guidelines -- they do not indicate
a single "correct" course of
action. The Purchasing
Specifications are designed for “plug
and play” to address key issues
in the context of a larger
purchasing process in a specific State
context. Thus, they can assist Medicaid
and SCHIP
agencies operating in different health
systems and under different State policies.
Purchasing specifications might be used
as a checklist for comparing contract
language, as a
source for examples of legally accurate
provisions, or as a way to explore specific
contract issues
in greater depth. The following examples
illustrate how purchasing specifications
might be used
by different agencies.
State Maternal and Child Health (MCH)
Programs may wish to use the Pediatric
Purchasing
Specifications to:
-
Raise maternal and child health issues
with the State Medicaid agency;
-
Integrate appropriate public health
surveillance activities -- such as immunization
registries
or birth defects surveillance -- with
managed care efforts;
-
Clarify the role of Programs for Children
with Special Health Care Needs (CSHCN)
in
financing extra items and services for
Medicaid beneficiaries under age 21;
-
Ensure that quality standards appropriate
to children's unique developmental,
physical, and
mental health needs are reflected in
the contract;
-
Ensure reimbursement for Medicaid-covered
services provided through local health
or early
intervention agencies (under Part C
of IDEA); and
-
Define linkage and referral mechanisms
between outreach and home visiting programs
for
families with young children.
State Medicaid Agencies may choose to
use pediatric specifications to:
-
Maximize the value of purchasing Medicaid
or SCHIP coverage for children;
- Better
define standards and expectations of
MCOs, particularly under the EPSDT benefit
for
children and services for children with
special health care needs;
- Better
define services that go into determination
of a capitation rate for Medicaid or
SCHIP,
particularly the EPSDT benefit for children
and services for children with special
health care
needs;
- Better
define performance expectations of MCOs,
beyond typical measures such as
immunization or prenatal care rates;
- Define
the outreach, informing, and support
services required under EPSDT, clarifying
and
specifying the expected role of MCOs;
- Better
integrate Medicaid or SCHIP managed
care with other publicly supported services
such as early intervention for infants
and toddlers, school-based health services,
home
visiting, or mental health services;
- Assist
in reducing overall State spending by
avoiding unnecessary public health expenditures
for children enrolled in Medicaid or
SCHIP (e.g., immunization, lead poisoning,
transportation, or case management);
and
-
Focus on selected outcomes to improve
health and reduce costs in areas such
as obstetrical
risk management, early childhood developmental
screening, or preventive services to
adolescents.
Having clear and specific contracts is
key to optimal service for children and
families enrolled in
managed care plans. The Pediatric Purchasing
Specifications are a tool to assist with
improving
contract language. Each player in the
health care system has a role to play.
Suggestions for
using the pediatric purchasing specifications
to improve contract provisions related
to pediatric
care are shown in Table 2.
Table
2. A Contract Review Tool for Purchasing
Child Health Services in Medicaid
Managed Care
Does your State’s Medicaid
managed care contract:
-
Specify pediatric services covered,
including items necessary to prevent,
correct, or ameliorate a condition,
disability, illness, or injury
or to promote growth and developmental,
or to maintain functioning.
-
Specify coverage of recommended
childhood immunizations without
prior authorization.
-
Specify coverage of items and
services for an enrolled child
under an Individualized Family
Services Plan (IFSP) or an Individualized
Education Program (IEP) developed
by an agency under the Individuals
with Disabilities Education Act
(IDEA)
-
Specify coverage of dental services.
-
Reference "Bright Futures:
Guidelines for Health Supervision
of Infants, Children, and Adolescents"
or other applicable medical
and dental association guidelines.
-
Prohibit prior authorization with
respect to comprehensive well-child
(EPSDT) screens based on a State’s
periodic visit schedule, as well
as interperiodic visits not on
the schedule.
-
Prohibit denial of coverage for
newborns due to a "pre-existing
condition" according to the
Newborns' and Mothers' Health
Protection Act of 1996.
-
Require that plans offer the family
or caregiver of a child with special
health care needs the option of
designating as the child's primary
care provider a pediatric
specialist participating
in the provider network as described
in enrollee information materials.
-
Require that safety net providers
be included in provider networks.
-
Require timely access to pediatric
services, including an initial
assessment of an enrolled child
conducted by a primary care provider
using the standards of Bright
Futures.
-
Specify elements for Memorandum
of Understanding (MOU) defining
relationships between the contractor
and public health departments,
Title V agency, SCHIP agency,
child welfare agency, State and
local education agencies, developmental
disabilities agency, and mental
health and substance abuse agency.
-
Specify use of quality measures
or studies appropriate for children.
-
Specify that the contractor shall
collect and report to the purchaser
on underutilization of services
by enrolled children.
-
Require that contractor ensure
each provider furnishing covered
immunizations participate in the
Vaccines for Children Program.
-
Specify remedies for noncompliance
or nonperformance, such as withholding
payments, suspension of enrollment,
or money penalties.
Source: George Washington University
Center for Health Services Research
and Policy. Pediatric Purchasing
Specifications Module © 2001 |
1
Rosenbaum S and Markus AR. Policy
Brief #2 "State Benefit Design Choices
under SCHIP: Implications for
pediatric health care. Washington,
DC: The George Washington University,
2002.
2
Rosenbaum S, et al. Negotiating the
New Health System: A nationwide study
of Medicaid Managed Care
Contracts. (First Edition) Washington,
DC: The George Washington University,
1997.
3
Rosenbaum S, et al. Negotiating the New
Health System: A nationwide study of Medicaid
Managed Care
Contracts. First Edition, 1997; Second
Edition, 1998; Third Edition, 1999; Fourth
Edition, 2001. Washington, DC:
The George Washington University.
4
Rosenbaum S, Sonosky CA, Shaw K, et al.
Negotiating the New Health System: A nationwide
study of Medicaid
Managed Care Contracts. Third Edition,
Vol. 1, 1999. Washington, DC: The George
Washington University. |