Office of Medicare Hearings and Appeals (OMHA)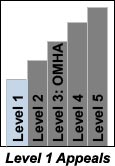 Level 1, Original Medicare (Parts A & B)
Documents in PDF format require the Adobe Acrobat Reader®. If you experience problems with PDF documents, please download the latest version of the Reader®. Documents in DOC format require Microsoft Word® or Microsoft Word Viewer® . If you experience problems with DOC documents, please download Word Viewer 2003®. You can download the Chart of the Appeals Process for Those with Original Medicare - Parts A & B [PDF - 56KB, DOC - 52KB]. The chart contains the overview for the entire appeals process for Original Medicare.
Medicare contracts with private companies to process medical claims (bills) for health care items and services provided to Medicare beneficiaries. After a claim is sent to the appropriate contractor, the contractor must: - Determine if the items and services on the claim are covered or reimbursable by Medicare;
- Calculate any amount that is payable by Medicare;
- Make the payments to health care provider(s) who furnished the items or services; and
- Notify you of its decision to pay or deny coverage or payment for specific items or services.
If you disagree with Medicare's decision on your claim, you have the right to file an appeal. The first level of an appeal for ORIGINAL Medicare is called a redetermination. A redetermination is performed by the same contractor that processed your Medicare claim. However, the individual that performs the appeal is not the same individual that processed your claim. The appeal is a new and independent review of your claim. Your appeal rights are on the last page or back of the Medicare Summary Notice that is mailed to you from a contractor that processes claims for Medicare. The notice will also tell you why your claim was not paid and what appeal steps you can take. You can request an appeal within 120 days from the date you received the Medicare Summary Notice. If you wish to file an appeal, follow the instructions on the Medicare Summary Notice. For more information about filing a Level 1 appeal, visit the "Appeals and Grievance" section of Medicare.gov. If your Level 1 appeal was not decided in your favor, you may wish to file a Level 2 appeal. In Original Medicare (Parts A&B), a Level 2 appeal is called a QIC reconsideration.
Please note that the Office of Medicare Hearings and Appeals is responsible only for the Level 3 claims appeals and certain Medicare entitlements and IRMAA appeals. OMHA is not responsible for levels 1, 2, 4, and 5 of the appeals process. OMHA provides additional information on other levels of appeals to help you understand the appeals process in a broad context.
|