|
Frequently
Asked Questions about
CMV
On this page:
What is
CMV?
 |
 |
 |
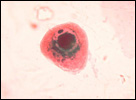
CMV infection of a cell in urine |
 |
CMV, or cytomegalovirus (sī-to-MEG-a-lo-vī-rus), is a common virus that infects people of all ages. Once CMV is in a person’s body, it stays there for life. Most infections with CMV are “silent,” meaning most people who are infected with CMV have no signs or symptoms. However, CMV can cause disease in unborn babies and in people with a weakened immune system.CMV is a member of the herpesvirus family, which includes the herpes simplex viruses and the viruses that cause chickenpox (varicella-zoster virus) and infectious mononucleosis (Epstein-Barr
Virus).
Who is at risk for CMV disease?
Anyone can become infected with CMV. Most healthy adults and
children who have a CMV infection will have few, if any, symptoms. However, certain groups are at higher risk of getting CMV
disease. These groups include
- unborn babies who are infected during pregnancy
- people with a weakened (immunocompromised) immune system
Risk of CMV infection is likely to be reduced by careful attention to good personal hygiene, such as hand washing. |
How is CMV spread?
- Person to person contact (such as, kissing, sexual
contact, and getting saliva or urine on your hands and then
touching your eyes, or the inside of your nose or mouth)
- Through the breast milk of an infected woman who is
breast feeding
- Infected pregnant women can pass the virus to their
unborn babies
- Blood transfusions and organ transplantations
CMV is sometimes found in body fluids, including urine, saliva (spit), breast milk, blood, tears, semen, and vaginal fluids. A person can become infected with CMV when they come in contact with
infected body fluids. However, people who are CMV-positive
(have been infected with CMV sometime in the past) usually do
not have virus in these fluids, so the chance of getting a CMV infection from casual contact is very small.
Contact with the saliva or urine of young children is a major cause of CMV infection among pregnant women. |
Women who are pregnant or planning a pregnancy should follow hygienic practices (e.g., careful handwashing) to avoid CMV infection. Because young children are more likely to have CMV in their urine or saliva (spit) than are older children or adults,
pregnant women who have young children or work with young children should be especially careful.
What are the signs and symptoms of CMV?
Most healthy children and adults infected with CMV have no symptoms and may not even know that they have been infected. Others may develop a mild illness. Symptoms may include fever, sore throat, fatigue, and swollen glands.
These symptoms are similar to those of other illnesses, so most people
are not aware that they are infected with CMV.
Most babies born with CMV (in other words, "congenital" CMV) never develop symptoms or disabilities. When babies do have symptoms, some can go away but others can be permanent.
Examples of symptoms or disabilities caused by congenital (meaning present at birth) CMV:
| Temporary Symptoms |
Permanent Symptoms or Disabilities |
- Liver problems
- Spleen problems
- Jaundice (yellow skin and eyes)
- Purple skin splotches
- Lung problems
- Small size at birth
- Seizures
|
- Hearing loss
- Vision loss
- Mental disability
- Small head
- Lack of coordination
- Seizures
- Death
|
In some children, symptoms do not appear until months or years after birth. The most common of these late-occurring symptoms are hearing loss and vision loss. Children with congenital CMV are more likely to have permanent disabilities and symptoms that get worse if they had symptoms of CMV infection at birth. But, some children who appear healthy at birth can develop hearing or vision loss over time due to congenital CMV. For this reason, if you know your baby was born with CMV, it is important to have her
or him hearing and vision tested regularly.
What health problems does CMV cause in babies?
- Hearing Loss
- Vision Loss
- Mental Disability
- Lung Problems
- Bleeding Problems
- Spleen Problems
- Liver Problems
- Growth Problems
CMV can cause symptoms when the baby is born or later in the baby’s life. Most babies born with CMV never develop symptoms or disabilities. In some infants, hearing or vision loss occur months or years after birth.
How do I know if I have CMV?
Most CMV infections are not diagnosed because the infected person usually has few or no symptoms. However, persons who have been infected with CMV develop antibodies to the virus, which may stay in a person's body for their lifetime. Antibodies are immune proteins
that are the body's response to infection.
A blood test can tell a person if they have CMV, but this test is not commonly performed. Laboratory tests can detect the virus in a person's body fluids (blood or urine) or by a tissue biopsy (a small piece of the body's tissue). CMV can
also be detected in the body by measuring the antibodies (immune proteins) in the blood targeted against CMV. This is called serologic testing.
Congenital CMV disease is most likely to occur when a woman is infected for the first time during a pregnancy. This is known as a primary CMV infection. Primary infections occur in 1%-4% of
seronegative (have no CMV antibodies) pregnant women and lead to fetal infection in
one-third of these pregnancies. In women who are already
infected before becoming pregnant (CMV seropositive women), CMV reactivation or reinfection
leads to fetal infection in less than 1% of pregnancies.
Approximately 10% of congenitally infected infants who have
symptoms at birth, and of the 90% who have no symptoms, 10%-15% will develop symptoms over months or even years.
How do you prevent CMV during pregnancy?
 |
 |
 |
Wash hands with plenty of soap and water. |
 |
No actions can eliminate all risks of becoming infected
with CMV, but there are
measures that can reduce spread of
the disease:
- Wash hands often with soap and water, especially after changing diapers.
Wash well for 15 to 20 seconds. More information on hand
washing is available on the CDC
Ounce of Prevention site.
- Do not kiss young children under the age of 5 or 6 on the mouth or cheek. Instead, kiss them on the head or give them a big hug.
- Do not share food, drinks, or utensils (spoons or forks) with young children.
If you are pregnant and work in a day care center, reduce your risk of getting CMV by working with children who are older than 2 ½ years of age, especially if you
are CMV seronegative (have never been infected with CMV) or are unsure if you
are seronegative.
If I have a baby with congenital CMV, will my next baby also have congenital CMV?
Nearly all women who have one baby with congenital CMV will be protected from future CMV infections because they have developed immunity.
There have been few reports of mothers who gave birth to more than one baby with congenital CMV.
However, these cases are rare.
Is there a treatment for CMV?
Currently, no treatment is recommended for CMV infection in the healthy individual,
including pregnant women. However, antiviral drugs ganciclovir and valganciclovir
are being used for patients with weakened immune systems. Antiviral drugs are being tested in infants born with congenital CMV. Because of its strong side effects, ganciclovir should only be considered for infants with severe congenital CMV
disease.
Vaccines for preventing CMV infection are still in the research and development stage.
|