You are here:
Health Information
Pemphigus
PDF Version of this Document Order this publication
Publication Date: April 2007
Questions and Answers about Pemphigus
This booklet contains general information about pemphigus. It describes what pemphigus is and how it is diagnosed and treated. At the end is a list of key words to help you understand the medical terms used in this booklet. If you have further questions after reading this booklet, you may wish to discuss them with your doctor.
What Is Pemphigus?
Pemphigus is a group of rare autoimmune diseases that cause blistering of the skin and mucous membranes (mouth, nose, throat, eyes, and genitals). Some forms of the disease, including the most common form, may be fatal if left untreated.
- What Causes Pemphigus?
- Is Pemphigus Contagious?
- Is Pemphigus Hereditary?
- Who Gets Pemphigus?
- What Are the Different Types of Pemphigus?
- What Is Pemphigoid, and How Is It Different From Pemphigus?
- How Is Pemphigus Diagnosed?
- What Type of Doctor Treats Pemphigus?
- How Is Pemphigus Treated?
- What Is the Prognosis for People Who Have Pemphigus?
- What Are Researchers Learning About Pemphigus?
- Where Can People Get More Information About Pemphigus?
- Key Words
Illustration
What Causes Pemphigus?
Normally, our immune system produces antibodies that attack viruses and harmful bacteria to keep us healthy. In people with pemphigus, however, the immune system mistakenly attacks the cells in the epidermis, or top layer of the skin, and the mucous membranes. The immune system produces antibodies against proteins in the skin known as desmogleins. These proteins form the glue that keeps skin cells attached to keep the skin intact. When desmogleins are attacked, skin cells separate from each other and fluid can collect between the layers of skin, forming blisters that do not heal. In some cases, these blisters can cover a large area of skin.
It is unclear what triggers the disease, although it appears that some people have a genetic susceptibility. Environmental agents may trigger the development of pemphigus in people who are likely to be affected by the disease because of their genes. In rare cases, it may be triggered by certain medications. In those cases, the disease usually goes away when the medication is stopped.
Is Pemphigus Contagious?
Pemphigus is not contagious. It does not spread from person to person.
Is Pemphigus Hereditary?
Though there can be a genetic predisposition to develop pemphigus, there is no indication the disease is hereditary.
Who Gets Pemphigus?
Pemphigus affects people across racial and cultural lines. Research has shown that certain ethnic groups (such as the eastern European Jewish community and people of Mediterranean descent) are more susceptible to pemphigus. A particular type of pemphigus occurs more frequently in people who live in the rain forests of Brazil.
Men and women are equally affected. Research studies suggest a genetic predisposition to the disease. Although the onset usually occurs in middle-aged and older adults, all forms of the disease may occur in young adults and children.
What Are the Different Types of Pemphigus?
There are several types of pemphigus and other similar blistering disorders. The type of disease depends on what level in the skin the blisters form and where they are located on the body. Blisters always occur on or near the surface of the skin, which is called the epidermis. People with pemphigus vulgaris, for example, have blisters that occur within the lower layer of the epidermis, while people with pemphigus foliaceus have blisters that form in the topmost layer. The type of antibody that is attacking the skin cells may also define the type of disease present.
Skin Structure
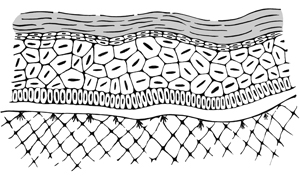
- Pemphigus vulgaris is the most common type of pemphigus in the United States. Soft and limp blisters appear on healthy-looking skin and mucous membranes. The sores almost always start in the mouth. The blisters of pemphigus vulgaris form within the deep layer of the epidermis, and are often painful. Blistered skin becomes so fragile that it may peel off by rubbing a finger on it. The blisters normally heal without scarring, but pigmented spots may remain for a number of months.
- Pemphigus vegetans is a form of pemphigus with thick sores in the groin and under the arms.
- Pemphigus foliaceus involves crusted sores or fragile blisters that often appear first on the face and scalp and later on the chest and other parts of the body. Unlike pemphigus vulgaris, blisters do not form in the mouth. The sores are superficial and often itchy, and are rarely as painful as pemphigus vulgaris blisters. There may also be loose, moist scales on the skin.
- IgA pemphigus is a blistering disorder in which a different type of antibody binds to the cell surface of epidermal cells. This disease is different from other forms of pemphigus because it involves a different type of antibody (called IgA) than other types. The disease may result in blisters similar to those seen in pemphigus foliaceus, or it may involve many small bumps containing pus. This is the most benign, or least harmful, form of pemphigus.
- Paraneoplastic pemphigus is a rare disease that is distinct from pemphigus, but shares some features of it. It occurs in people with certain types of cancer, including some lymphomas and leukemias. It often involves severe ulcers of the mouth and lips, cuts and scarring of the lining of the eye and eyelids, and skin blisters. Because the antibodies also bind the airways, patients may develop life-threatening problems in the lungs. This disease is different from pemphigus, and the antibodies in the blood are different. Special tests may be needed to identify paraneoplastic pemphigus.
What Is Pemphigoid, and How Is It Different From Pemphigus?
Pemphigoid is also a blistering disorder caused by autoimmune problems that result in an attack on the skin cells by a person’s own antibodies. Pemphigoid produces a split in the cells where the epidermis and dermis, the layer below the epidermis, meet, causing deep, tense blisters that do not break easily. Pemphigus, on the other hand, causes a separation within the epidermis, and the blisters are soft, limp, and easily broken. Pemphigoid is seen most often in the elderly and may be fatal. Usually, both pemphigus and pemphigoid are treated with similar medications. Severe cases may require different treatment.
How Is Pemphigus Diagnosed?
A diagnosis of pemphigus has several parts:
- A visual examination by a dermatologist. The doctor will take a complete history and physical exam, noting the appearance and location of the blisters.
- A blister biopsy. A sample of a blister is removed and examined under the microscope. The doctor will look for cell separation that is characteristic of pemphigus, and will also determine the layer of skin in which the cells are separated.
- Direct immunofluorescence. A biopsy of a skin sample is treated in the laboratory with a chemical compound to find the abnormal desmoglein antibodies that attack the skin. The specific type of antibodies that form may indicate what type of pemphigus exists.
- Indirect immunofluorescence. Sometimes called an antibody titre test, a sample of blood is tested to measure pemphigus antibody levels in the blood and help determine the severity of the disease. Once treatment begins, this blood test may also be used to find out if treatment is working.
Pemphigus is a serious disease, and it is important to do all of these tests to confirm a diagnosis. No single test is right all of the time.
Because it is rare, pemphigus is often the last disease considered during diagnosis. Early diagnosis may permit successful treatment with only low levels of medication, so consult a doctor if you have persistent blisters on the skin or in the mouth. In the most common form of pemphigus (pemphigus vulgaris), the mouth is often the first place that blisters or sores appear.
What Type of Doctor Treats Pemphigus?
Pemphigus is a rare disease of the skin; therefore, dermatologists are the doctors best equipped to diagnose and treat people with pemphigus. If you have blisters in the mouth, a dentist can provide guidance for maintaining good oral health. This is important for preventing gum disease and tooth loss.
How Is Pemphigus Treated?
Treatment for pemphigus vulgaris involves using one or more drugs. High-dose oral corticosteroids, such as prednisone or prednisolone, are the main treatment for pemphigus. These are anti-inflammatory medicines that suppress the immune system. High doses are often required to bring pemphigus under control. To minimize the side effects patients may experience, once the disease begins to subside the corticosteroid levels are reduced slowly to the lowest level required to prevent new blisters or sores from appearing. Many patients will go into complete remission with treatment, although this may take a number of years. Other patients will need to continue to take small doses of medication to keep the disease under control. Prednisone is usually taken by mouth, but can also be injected into a vein, muscle, or directly into a blister. The route depends on the type and severity of disease. Usually, a corticosteroid cream will be used directly on the blisters.
To keep the levels of corticosteroid use to a minimum, immunosuppressive drugs are often added to a patient’s treatment. These are drugs that stop or slow down the immune system’s response to what it sees as an attack on the body. They include:
- Myco-phenolate mofetil (CellCept*)
- Azathioprine (Imuran)
- Cyclophosphamide (Cytoxan)
- Methotrexate.
Other drugs that may be used include:
- Dapsone (DDS)
- Antibiotics such as tetracycline.
* Brand names included in this booklet are provided as examples only and their inclusion does not mean that these products are endorsed by the National Institutes of Health or any other Government agency. Also, if a particular brand name is not mentioned, this does not mean or imply that the product is unsatisfactory.
All of these medications can cause serious side effects. You should see your doctor regularly for blood and urine tests. Be sure to report any problems or side effects you experience to the doctor. With prolonged high-dose corticosteroid therapy, common side effects include susceptibility to life-threatening infections, delayed wound healing, osteoporosis, cataracts, glaucoma, type 2 diabetes, loss of muscle mass, peptic ulcers, swelling of the face and upper back, and salt and water retention. To reduce the risk of osteoporosis, bone density measurements are taken, and patients with low bone density are prescribed medications such as alendronate (Fosamax) or risedronate (Actonel). Extra calcium and vitamin D intake, exercise, and stopping smoking are also recommended. For diabetes caused by steroid use, patients must be on a low sugar diet and may need to take antidiabetic medications.
The immunosuppressive drugs that are used to treat pemphigus can also increase the chances of developing an infection and may cause anemia, a decrease in the white blood cells in the blood, inflammation of the liver, nausea, vomiting, or allergic reactions.
People with severe pemphigus that cannot be controlled with corticosteroids may undergo plasmapheresis, a treatment in which the blood containing the damaging antibodies is removed and replaced with blood that is free of antibodies. Such patients can also be treated with IVIg, or intravenous immunoglobulin, which is given daily for 3 to 5 days, every 2 to 4 weeks for 1 to several months. Plasmapheresis and IVIg are both very expensive treatments, since they require large amounts of donated and specially processed blood. Scientists have reported success in treating difficult cases of pemphigus vulgaris with a combination of IVIg and rituximab, a cancer medication.
The treatment prescribed will depend on the type of pemphigus and the severity of the disease. Work closely with your doctor to devise the treatment regimen that works best for you. Because the medications used to treat pemphigus are strong medications with potentially serious side effects, every doctor that you see should be made aware of the type and amount of medications you are taking.
It may take several months to years for the ulcers and blisters of pemphigus vulgaris to disappear after treatment has begun because circulating antibodies remain in the blood for a long time. Lesions in the mouth are particularly slow to heal. Blisters in the mouth can make brushing the teeth painful, leaving you prone to gum disease and tooth loss. A dentist can offer approaches that enable you to maintain healthy teeth and gums. Avoiding spicy, hard, and acidic foods will help, since those foods can irritate or trigger the blisters. If you are taking corticosteroids, you should receive advice for maintaining a diet low in calories, fat, and sodium, and high in potassium and calcium.
What Is the Prognosis for People Who Have Pemphigus?
The outlook for people with pemphigus has changed dramatically in the past 40 years. A person diagnosed with pemphigus vulgaris in the 1960s faced the reality that they had a disease that was rare, usually fatal, poorly understood, with no good treatment options. Today, through medical research supported by the National Institutes of Health (NIH), the picture is dramatically better. The disease is now rarely fatal, and the majority of deaths occur from infections. For most people with pemphigus, the disease can be controlled with corticosteroids and other medications, and these medications can eventually be completely discontinued. However, as described earlier, these medications can cause side effects that can sometimes be serious. Pemphigus and its treatments can be debilitating and cause lost time at work, weight loss, loss of sleep, and emotional distress. The International Pemphigus Foundation provides patient support services to help people with the disease cope with its effects.
What Are Researchers Learning About Pemphigus?
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), a part of the Department of Health and Human Services’ National Institutes of Health, supports a broad range of research on pemphigus to better understand what causes various forms of the disease and to develop better treatments. When researchers began to understand that pemphigus is an autoimmune disease, they were able to target their laboratory studies on immune function and to apply research advances in other autoimmune diseases to pemphigus. They have already clarified that effective therapies against this disease must stop production of the antibodies that attack the skin cells.
Environmental and genetic risk factors: Researchers are trying to determine the environmental and genetic risk factors for pemphigus by studying populations that have high rates of the disease, such as people living in certain rural areas of Brazil.
Basic research: Scientists are working in laboratories to study the antibodies that attack skin cells. They are studying the genes that interact when the body’s antibodies attack healthy tissue. Other NIAMS-supported researchers are studying animal models of various forms of pemphigus to define the events that trigger the development of the blistering skin and mucous membranes.
Clinical research: To help patients on current therapies involving high-dose corticosteroid treatments, researchers are testing approaches to reduce the risk of osteoporosis and other side effects related to corticosteroid use.
Designing better treatment options: Other scientists are devising treatments to avoid the use of high-dose corticosteroids altogether. They are working to design drugs that more effectively inhibit antibody formation without the side effects that can occur with current treatments.
Where Can People Get More Information About Pemphigus?
-
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
Information Clearinghouse
National Institutes of Health1 AMS Circle
Bethesda, MD 20892-3675
Phone: 301-495-4484
Toll Free: 877-22-NIAMS (226-4267)
TTY: 301–565–2966
Fax: 301-718-6366
Email: NIAMSinfo@mail.nih.gov
Website: http://www.niams.nih.govNIAMS provides information about various forms of arthritis and other rheumatic diseases and bone, muscle, joint, and skin diseases. It distributes patient and professional education materials and refers people to other sources of information. Additional information and updates can also be found on the NIAMS Web site.
-
American Academy of Dermatology (AAD)
P.O. Box 4014
Schaumberg, IL 60168-4014
Phone: 847-330-0230
Toll Free: 888-462-3376
Fax: 847-330-0050
Website: http://www.aad.orgThis national professional association for dermatologists provides referrals to dermatologists. Their Web site has a brochure on “Bullous diseases” that includes information on pemphigus. You can find other information on dermatology topics through their Web site’s public resource center.
-
The International Pemphigus Foundation
1540 River Park Drive, Suite 208
Sacramento, CA 95815
Phone: 916-922-1298
Fax: 916-922-1458
Email: pemphigus@pemphigus.org
Website: http://www.pemphigus.orgThis nonprofit organization offers information for patients (including questions to ask the doctor) and health care providers, gives physician referrals, and provides patient support services.
-
American Autoimmune-Related Diseases Association, Inc. (AARDA)
22100 Gratiot Ave.
East Detroit, MI 48021
Phone: 586-776-3900
Toll Free: 800-598-4668
Fax: 586-776-3903
Email: aarda@aarda.org
Website: http://www.aarda.orgThis organization is involved in education, public awareness, research, and patient services that focus on autoimmunity.
-
National Organization For Rare Disorders (NORD)
55 Kenosia Avenue, P.O. Box 1968
Danbury, CT 06813-1968
Phone: 203-744-0100
Toll Free: 800-999-6673
Email: orphan@rarediseases.org
Website: http://www.rarediseases.orgThis organization provides information on numerous rare diseases and disorders, referrals to patient organizations, and medication assistance programs. It has a fact sheet on pemphigus available for a small fee.
Key Words
-
Adverse reaction: An unwanted effect attributed to a medication or therapy.
Animal model: A laboratory animal useful for medical research because it has specific characteristics that resemble a human disease or disorder. Scientists can create animal models, often laboratory mice, by transferring new genes into them.
Antibodies: Proteins made by the body to attack foreign invaders, such as viruses and harmful bacteria, to keep the body healthy.
Autoantibodies: Antibodies that attack one’s own cells.
Autoimmunity: Immune responses that are inappropriately directed at a person’s own tissues.
Benign: Not life-threatening.
Cataracts: Clouding of the lens of the eye.
Corticosteroids: Potent anti-inflammatory hormones that are made naturally in the body or synthetically (man-made) for use as drugs. They are also called glucocorticoids. The most commonly prescribed drug of this type is prednisone. Dapsone: An anti-inflammatory drug that was first used to treat leprosy.
Dapsone: An anti-inflammatory drug that was first used to treat leprosy.
Dermatologist: A doctor who treats problems of the skin, hair, and nails.
Dermis: The layer of skin cells under the uppermost layer, the epidermis.
Desmoglein: Proteins in the cells of the skin that form the “glue” that connects adjacent skin cells, keeping the skin intact.
Epidermis: The uppermost layer of skin cells.
Gene: The functional and physical unit of heredity passed from parent to offspring. Genes are pieces of DNA, and most genes contain the information for making a specific protein.
Genetic predisposition: Any condition in which genetic makeup leaves the individual more susceptible to disease.
Glaucoma: Abnormally high fluid pressure in the eye that can lead to vision loss or blindness.
Immune system: A complex network of specialized cells and organs that work together to defend the body against attacks by “foreign” invaders such as bacteria and viruses. In some conditions, it appears that the immune system does not function properly and may even work against the body.
Immunofluorescence: A specific type of laboratory test on a tissue or blood sample that is used to detect antibodies that can attack skin. The specific antibodies are labeled with a compound that makes them glow when observed microscopically under ultraviolet light.
Immunosuppressive drugs: Drugs that suppress the immune response and can be used to treat autoimmune disease. Unfortunately, because normal immunity is also suppressed with these drugs, they leave the body at risk for infection.
Infection: Invasion of the body tissues by bacteria or other tiny organisms that cause illness.
Osteoporosis: A disease characterized by low bone mass and structural deterioration of bone tissue, leading to bone fragility and an increased risk of fractures.
Acknowledgments
The NIAMS gratefully acknowledges the assistance of Carl Baker, M.D., and Alan Moshell, M.D., NIAMS; Jean Bystryn, M.D., New York University School of Medicine; Luis Diaz, M.D., the University of North Carolina; and John Stanley, M.D., the University of Pennsylvania School of Medicine in the preparation of this booklet. Cori Vanchieri was the author of this booklet.
The mission of the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), a part of the Department of Health and Human Services’ National Institutes of Health (NIH), is to support research into the causes, treatment, and prevention of arthritis and musculoskeletal and skin diseases; the training of basic and clinical scientists to carry out this research; and the dissemination of information on research progress in these diseases. The National Institute of Arthritis and Musculoskeletal and Skin Diseases Information Clearinghouse is a public service sponsored by the NIAMS that provides health information and information sources. Additional information can be found on the NIAMS Web site at www.niams.nih.gov.
For Your Information
This publication contains information about medications used to treat the health condition discussed here. When this booklet was printed, we included the most up-to-date (accurate) information available. Occasionally, new information on medication is released.
For updates and for any questions about any medications you are taking, please contact the U.S. Food and Drug Administration at:
-
U.S. Food and Drug Administration
Toll Free: 888-INFO-FDA (888-463-6332)
Website: http://www.fda.gov/
This booklet is not copyrighted. Readers are encouraged to duplicate and distribute as many copies as needed.
Additional copies of this booklet are available from
-
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
Information Clearinghouse
National Institutes of Health1 AMS Circle
Bethesda, MD 20892-3675
Phone: 301-495-4484
Toll Free: 877-22-NIAMS (226-4267)
TTY: 301–565–2966
Fax: 301-718-6366
Email: NIAMSinfo@mail.nih.gov
Website: http://www.niams.nih.gov
NIH Publication No. 07-7083