HealthDay Reporter
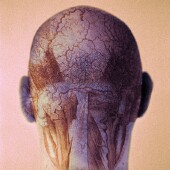
MONDAY, Sept. 15 (HealthDay News) -- Human stem cells derived from bone marrow can cut the brain damage caused by an interruption in blood supply, such as what happens after a heart attack, scientists report.
Although these initial results were seen in mice, researchers are hopeful the breakthrough will one day help humans struck by cardiac arrest or stroke.
The human cells did not trigger the development of new brain cells, as previously believed. Instead, they switched on and off different genes, essentially turning down inflammation and immune system reactions that were harmful to the brain.
"This is the first time that interactions between the two kinds of cells [injected cells and host cells] worked out," said Dr. Darwin Prockop, senior author of the study, which appears in this weeks issue of the Proceedings of the National Academy of Sciences.
The study was completed while Prockop was with Tulane University's Center for Gene Therapy. He recently accepted a post as Stearman Chair in Genomic Medicine at Texas A&M Health Science Center College of Medicine and is director of the Institute for Regenerative Medicine at Scott & White.
"The big thing was finding out how these cells were helping," Prockop elaborated. "This dramatic crosstalk was very surprising. The human cells specifically turned down immune and inflammatory reactions."
The finding "goes along with the argument that something here could be used in human therapy. Even though this is a short-term fix, it might be sufficient to have a reparative function," added Dr. Robert Schwartz, director of the Texas A&M Health Science Center Institute of Biosciences and Technology, in Houston.
For this study, Prockop's team at Tulane injected human mesenchymal stromal cells (hMSCs) into the brains of adult mice one day after blood flow to the rodents' brains had been temporarily blocked.
"The blood supply was tied off for just 15 minutes and then restored," Prockop explained. "That causes massive damage to the brain. It's the sort of thing that happens when you have a cardiac arrest ... It's not quite a stroke because you're cutting off the blood supply then returning it."
Although the human cells disappeared within about a week, they nevertheless exerted dramatic effects upon the brain. "The number of dead neurons dropped off about 60 percent. It was quite amazing," Prockop said. "And the motor responses of mice improved dramatically."
Further analysis revealed that the human and mouse cells were actually signaling to each other, with the human cells changing the way certain genes were expressed. This meant that certain harmful immune and inflammatory responses were considerably suppressed, the researchers said.
"These hMSCs are really blood cells and they have effects on vascular formation and angiogenesis [new blood vessel growth] and they also produce a fair number of growth factors and signaling factors that seem to ameliorate the disease process," Schwartz explained.
Ideally, the results would one day be translated into stroke and other therapies for humans, an area which is sadly lacking in options.
"This could be a therapy for patients who have had cardiac arrest either by itself or after surgery," Prockop said. "But the next step is to find out what human cells are producing to make all these effects."
"This is a really good study," Schwartz added. "It has a lot of value. Now the question is, can you move it eventually into the clinic and how do you go forward with the next set of studies involving large mammals and getting it generally approved by the FDA [U.S. Food and Drug Administration] as a methodology and treatment?"
More information
There's more on stem cell research at the U.S. National Institutes of Health.
SOURCES: Darwin Prockop, M.D., Ph.D., Stearman Chair in Genomic Medicine, professor, molecular and cellular medicine, Texas A&M Health Science Center College of Medicine, and director, Institute for Regenerative Medicine, Scott & White; Robert Schwartz, Ph.D., director, Texas A&M Health Science Center Institute of Biosciences and Technology, Houston; Sept. 15-19, 2008, Proceedings of the National Academy of SciencesCopyright © 2008 ScoutNews, LLC
 . All rights reserved.
. All rights reserved.HealthDayNews articles are derived from various sources and do not reflect federal policy.
omhrc.gov does not endorse opinions, products, or services that may appear in news stories.