HIV and Older Americans
In 2018, over half (51%) of people in the United States (US) and dependent areasa with diagnosed HIV were aged 50 and older. Though new HIV diagnosesb are declining among people aged 50 and older, around 1 in 6 HIV diagnoses in 2018 were in this group. People aged 50 and older with diagnosed HIV are living longer, healthier lives because of effective HIV treatment.
The Numbers
HIV Diagnoses

New HIV Diagnoses Among People Aged 50 and Older in the US and Dependent Areas by Transmission Category and Sex, 2018*



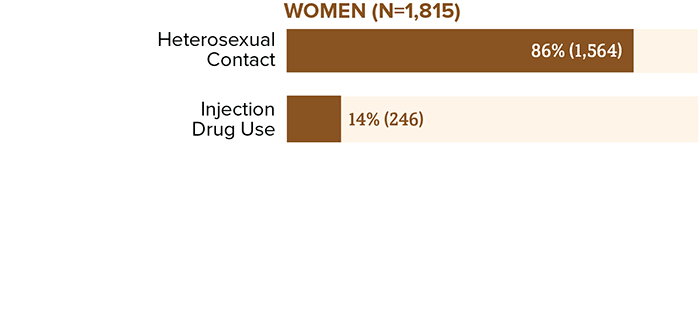
Total for men may not equal 100% due to rounding.
* Based on sex at birth and includes transgender people.
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated). HIV Surveillance Report 2020;31.
New HIV Diagnoses Among Adults and Adolescents in the US and Dependent Areas by Age, 2018



Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated). HIV Surveillance Report 2020;31.
From 2014 to 2018, HIV diagnoses decreased 6% overall among people aged 50 and older, with trends varying by sex and transmission category.
HIV Diagnoses Among People Aged 50 and Older in the US and Dependent Areas, 2014-2018*
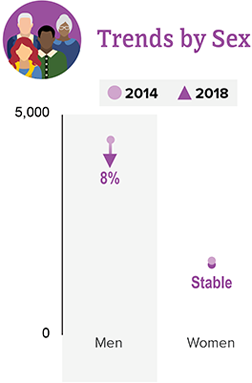

* Based on sex at birth and includes transgender people.
Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated). HIV Surveillance Report 2020;31.
Living with HIV
People Aged 55 and Older with HIV in the 50 States and the District of Columbia



It is important for people aged 50 and older to know their HIV status so they can take medicine to treat HIV if they have the virus. Taking HIV medicine every day can make the viral load undetectable. People who get and keep an undetectable viral load (or stay virally suppressed) can live a long and healthy life. They also have effectively no risk of transmitting HIV to HIV-negative sex partners.
* Had 2 viral load or CD4 tests at least 3 months apart in a year.
† Based on most recent viral load test.
Source: CDC. Estimated HIV incidence and prevalence in the United States 2014–2018. pdf icon[PDF – 3 MB] HIV Surveillance Supplemental Report. 2018;25(1).
Adults and Adolescents with Diagnosed HIV in the US and Dependent Areas by Age, 2018



Source: CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated). HIV Surveillance Report 2020;31.
Deaths
In 2018, there were 11,425 deaths among people aged 50 and older with diagnosed HIV in the US and dependent areas. These deaths could be from any cause.
Prevention Challenges
There are some behaviors that put everyone at risk for HIV. These include having anal or vaginal sex without protection (like a condom or medicine to prevent or treat HIV) or sharing injection drug equipment with someone who has HIV. Other factors that affect older people particularly include:
Although they visit their doctors more frequently, older people and their providers are less likely to discuss sexual or drug use behaviors. Health care providers may not ask patients aged 50 and older about these issues or test them for HIV. Also, older people may not consider themselves to be at risk for HIV, may be embarrassed to discuss sex, or may mistake HIV symptoms for those of normal aging.
Older people may have many of the same HIV risk factors as younger people, including a lack of knowledge about HIV prevention and sexual risk, such as having multiple sex partners, and may be less likely to use a condom or other prevention options.
Older people in the United States are more likely than younger people to have late-stage HIV infection at the time of diagnosis. People aged 50 and older may start treatment late, which may put this population at risk of more immune system damage. Among people aged 55 and older who received an HIV diagnosis in 2015, 50% had HIV for 4.5 years before they were diagnosed—the longest diagnosis delay for any age group.
Stigma is common among adults with HIV and negatively affects people’s quality of life, self-image, and behaviors. People aged 50 and older may avoid getting the care they need or disclosing their HIV status because they may already face isolation due to illness or loss of family, friends, or community support.
Aging with HIV presents special challenges for preventing other diseases. Both age and HIV increase the risk for cardiovascular disease, lung disease (specifically chronic obstructive pulmonary disease), bone loss, and certain cancers. People aged 50 and older also need to be careful about interactions between medications used to treat HIV and those used to treat common age-related conditions such as hypertension, diabetes, elevated cholesterol, and obesity.
What CDC is Doing
CDC is pursuing a high-impact prevention approach to maximize the effectiveness of current HIV prevention interventions and strategies. Funding state, territorial, and local health departments and community-based organizations (CBOs) to develop and implement tailored programs is CDC’s largest investment in HIV prevention. This includes longstanding successful programs and new efforts funded through the Ending the HIV Epidemic initiative. In addition to funding health departments and CBOs, CDC is also strengthening the HIV prevention workforce and developing HIV communication resources for consumers and health care providers.
- Under the new integrated HIV surveillance and prevention cooperative agreement, CDC awarded around $400 million per year to health departments for HIV data collection and prevention efforts. This award directs resources to the populations and geographic areas of greatest need, while supporting core HIV surveillance and prevention efforts across the US.
- In 2019, CDC awarded $12 million to support the development of state and local Ending the HIV Epidemic plans in 57 of the nation’s priority areas. To further enhance capacity building efforts, CDC uses HIV prevention resources to fund the National Alliance of State and Territorial AIDS Directors (NASTAD) $1.5 million per year to support strategic partnerships, community engagement, peer-to-peer technical assistance, and planning efforts.
- In 2020, CDC awarded $109 million to 32 state and local health departments that represent the 57 jurisdictions across the United States prioritized in the Ending the HIV Epidemic. This award supports the implementation of state and local Ending the HIV Epidemic plans.
- Under the flagship community-based organization cooperative agreement, CDC awards about $42 million per year to community organizations. This award directs resources to support the delivery of effective HIV prevention strategies to key populations.
- In 2019, CDC awarded a cooperative agreement to strengthen the capacity and improve the performance of the nation’s HIV prevention workforce. New elements include dedicated providers for web-based and classroom-based national training, and technical assistance tailored within four geographic regions.
- Through its Let’s Stop HIV Together campaign, CDC offers resources about HIV stigma, testing, prevention, and treatment and care. This campaign is part of the Ending the HIV Epidemic.
a Unless otherwise noted, the term United States includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the US Virgin Islands.
b HIV diagnoses refers to the number of people who received an HIV diagnosis during a given time period, not when the people got HIV infection.
- CDC. Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated). HIV Surveillance Report 2020;31.
- CDC. Estimated HIV incidence and prevalence in the United States, 2014–2018 pdf icon[PDF – 3 MB]. HIV Surveillance Supplemental Report 2020;25(1).
- CDC. Selected national HIV prevention and care outcomes pdf icon[PDF – 2 MB] (slides).
- Glaude-Hosch JA, Smith ML, Heckman TG, Miles TP, Olubajo BA, Ory MG. Sexual behaviors, healthcare interactions, and HIV-related perceptions among adults age 60 years and older: an investigation by race/ethnicity. Curr HIV Res 2015;13(5):359-68. PubMed abstractexternal icon.
- Baugher AR, Beer L, Fagan JL, et al. Prevalence of internalized HIV-related stigma among HIV-infected adults in care, United States, 2011-2013. AIDS Behav 2017; 21(9):2600-8. PubMed abstractexternal icon.
- US Census Bureau. 2018 Data profile, Age and Sexexternal icon. Accessed July 7, 2020.
- National Institute on Aging. HIV, AIDS, and older peopleexternal icon [web page]. Accessed July 7, 2020.
- Dailey AF, Hoots BE, Hall HI, et al. Vital Signs: Human Immunodeficiency Virus testing and diagnosis delays—United States. MMWR 2017;66(47):1300-06.
- Onen NF, Shacham E, Stamm KE, Overton ET. Comparisons of sexual behaviors and STD prevalence among older and younger individuals with HIV infection. AIDS Care 2010;22(6):711-17. PubMed abstractexternal icon.
- Golub SA, Tomassilli JC, Pantalone DW, Brennan M, Karpiak SE, Parsons JT. Prevalence and correlates of sexual behavior and risk management among HIV-positive adults over 50. Sex Transm Dis 2010;37(10):615-20. PubMed abstract. external icon
- Brooks JT, Buchacz K, Gebo KA, Mermin J. HIV infection and older Americans: the public health perspective. Am J Public Health 2012;102(8):1516-26. PubMed abstractexternal icon.
- Althoff KN, Gebo KA, Gange SJ, et al. CD4 count at presentation for HIV care in the United States and Canada: are those over 50 years more likely to have a delayed presentation?AIDS Res Ther 2010;7:45. PubMed abstractexternal icon.
- Thrift AP, Chiao EY. Are non-HIV malignancies increased in the HIV-infected population? Curr Infect Dis Rep 2018;20(8):22. PubMed abstractexternal icon.
- Escota GV, O’Halloran JA, Powderly WG, Presti RM. Understanding mechanisms to promote successful aging in persons living with HIV. Int J Infect Dis 2018;66:56-64. PubMed abstractexternal icon.

