 The Cooperative Disability Investigations (CDI) Program continues to be one of our most successful initiatives, contributing to the integrity of SSA’s disability programs.
The Cooperative Disability Investigations (CDI) Program continues to be one of our most successful initiatives, contributing to the integrity of SSA’s disability programs.
SSA and OIG jointly established the CDI Program in Fiscal Year 1998, in conjunction with State Disability and Determination Services (DDS) and State or local law enforcement agencies, to effectively pool resources and expertise and prevent and detect fraud in SSA’s disability programs. The Units investigate disability claims under SSA’s Title II and Title XVI programs that State disability examiners believe are suspicious. The CDI program’s primary mission is to obtain evidence that can resolve questions of fraud before benefits are ever paid. CDI Units also provide reports to DDS examiners during continuing disability reviews (CDRs) that can be used to cease benefits of in-payment beneficiaries.
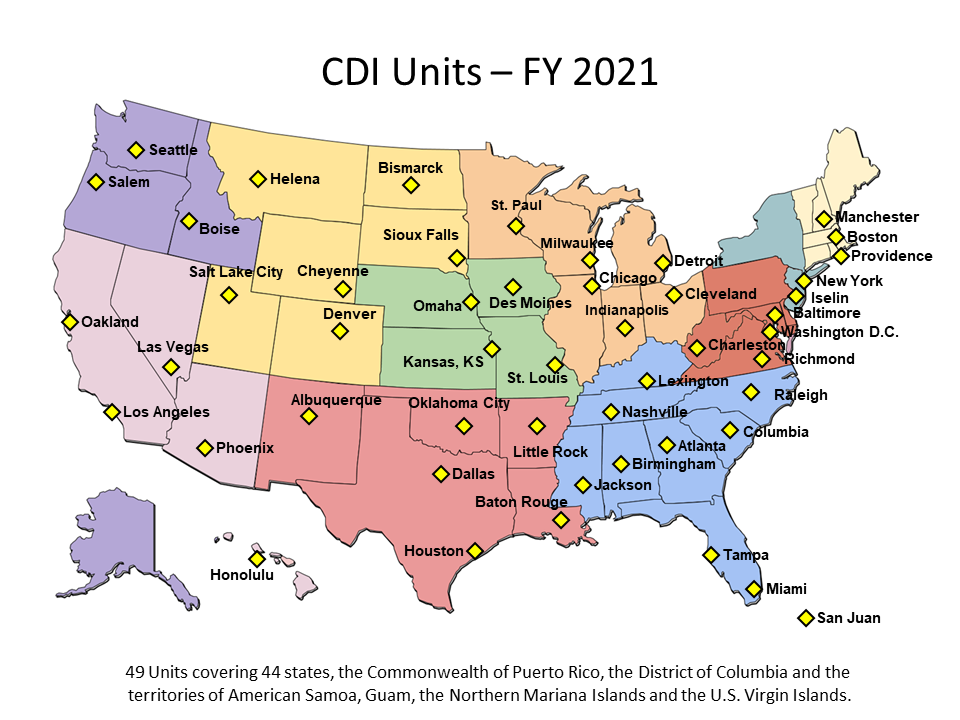
In FY1998, the CDI Program launched with single Units in five states. The program currently consists of 46 Units covering 37 states, the District of Columbia, and the Commonwealth of Puerto Rico. In FY2018, the CDI Program reported $188 million in projected savings to SSA’s disability programs. Since the program was established, through September 2018, the CDI efforts have resulted in $3.9 billion in projected savings to SSA’s disability programs and $2.9 billion in projected savings to non-SSA programs.
Each CDI Unit comprises an OIG Special Agent who serves as the Team Leader, employees from that State’s DDS and an SSA employee who act as programmatic experts, and State or local law enforcement officers. Tapping the skills of each member, the CDI Units receive benefit applications identified as suspicious by the DDS and, where appropriate, investigate these claims.
The process typically begins with a fraud referral from the DDS or SSA to the CDI Unit. We also receive fraud referrals from SSA’s Office of Hearing Operations, private citizens, anonymous sources, and other law enforcement agencies. Disability fraud can involve malingering, filing multiple applications, concealing work or other activities, and exaggerating or lying about disabilities.
Upon completion of the investigation, a report detailing the investigation is sent to the DDS, where DDS staff serves as the ultimate decision-making entity in determining whether a person is eligible to receive a monthly disability benefit payment. If the claimant is already receiving benefits, DDS and/or SSA will determine whether the person’s benefits should be continued or terminated. There is even, in some cases, the possibility of criminal prosecution or the imposition of civil monetary penalties or administrative sanctions.
To report suspected disability fraud, click here.
Fact Sheet: Cooperative Disability Investigations Program
Click the image to download a PDF:

