CDC Guideline for Prescribing Opioids for Chronic Pain
Improving the way opioids are prescribed through clinical practice guidelines can ensure patients have access to safer, more effective chronic pain treatment while reducing the number of people who misuse or overdose from these drugs.
CDC developed and published the CDC Guideline for Prescribing Opioids for Chronic Pain to provide recommendations for the prescribing of opioid pain medication for patients 18 and older in primary care settings. Recommendations focus on the use of opioids in treating chronic pain (pain lasting longer than 3 months or past the time of normal tissue healing) outside of active cancer treatment, palliative care, and end-of-life care.

Improving the way opioids are prescribed through clinical practice guidelines can ensure patients have access to safer, more effective chronic pain treatment while reducing the risk of opioid use disorder, overdose, and death. More than 11.5 million Americans, aged 12 or older, reported misusing prescription opioids in 2016.1
- An estimated 11% of adults experience daily pain
- Millions of Americans are treated with prescription opioids for chronic pain
- Primary care providers are concerned about patient addiction and report insufficient training in prescribing opioids
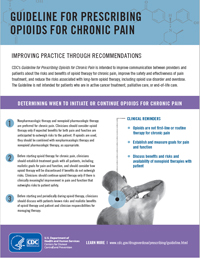
The CDC Guideline addresses patient-centered clinical practices including conducting thorough assessments, considering all possible treatments, closely monitoring risks, and safely discontinuing opioids. The three main focus areas in the Guideline include:
- Determining when to initiate or continue opioids for chronic pain
- Selection of non-pharmacologic therapy, nonopioid pharmacologic therapy, opioid therapy
- Establishment of treatment goals
- Discussion of risks and benefits of therapy with patients
- Opioid selection, dosage, duration, follow-up, and discontinuation
- Selection of immediate-release or extended-release and long-acting opioids
- Dosage considerations
- Duration of treatment
- Considerations for follow-up and discontinuation of opioid therapy
- Assessing risk and addressing harms of opioid use
- Evaluation of risk factors for opioid-related harms and ways to mitigate patient risk
- Review of prescription drug monitoring program (PDMP) data
- Use of urine drug testing
- Considerations for co-prescribing benzodiazepines
- Arrangement of treatment for opioid use disorder
| Opioid | Conversion Factor |
|---|---|
| Codeine | 0.15 |
| Fentanyl transdermal (in mcg/hr) | 2.4 |
| Hydrocodone | 1 |
| Hydromorphone | 4 |
| Methadone: 1-20 mg/day | 4 |
| Methadone: 21-40 mg/day | 8 |
| Methadone: 41-60 mg/day | 10 |
| Methadone: ≥61-80 mg/day | 12 |
| Morphine | 1 |
| Oxycodone | 1.5 |
| Oxymorphone | 3 |
| Tapentadol† | 0.4 |
Calculating the total daily dose of opioids helps identify patients who may benefit from closer monitoring, reduction or tapering of opioids, prescribing of naloxone, or other measures to reduce risk of overdose.
To determine dose in MMEs, multiply the dose for each opioid by the conversion factor. For example, tablets containing hydrocodone 5 mg and acetaminophen 300 mg taken four times a day would contain a total of 20 mg of hydrocodone daily, equivalent to 20 MME daily; extended-release tablets containing oxycodone 10mg and taken twice a day would contain a total of 20mg of oxycodone daily, equivalent to 30 MME daily.
- All doses should be in mg/day, except for fentanyl which should be in mcg/hr, before multiplying by the conversion factor.
- Equianalgesic dose conversions are only estimates and cannot account for individual variability in genetics and pharmacokinetics.
- Do not use the calculated dose in MMEs to determine the doses to use when converting opioid to another; when converting opioids the new opioid is typically dosed at substantially lower than the calculated MME dose to avoid accidental overdose due to incomplete cross-tolerance and individual variability in opioid pharmacokinetics.
- Use particular caution with methadone dose conversions because the conversion factor increases at higher doses.
- Use particular caution with fentanyl since it is dosed in mcg/hr instead of mg/day, and its absorption is affected by heat and other factors.
SOURCE: Adapted from Von Korff M, Saunders K, Thomas Ray G, et al. De facto long-term opioid therapy for noncancer pain. Clin J Pain. 2008 Jul–Aug; 24(6):521–527 and Washington State interagency guideline on prescribing opioids for pain; 2015.
For clinical guidance on dosage of opioids for treatment of chronic pain, please see these resources:
- MMWR: CDC Guideline for Prescribing Opioids for Chronic Pain
- Factsheet: Calculating Total Daily Dose of Opioids for Safer Dosagepdf iconpdf icon
- Mobile App: CDC Opioid Guideline
Additional clinical guidance, including opioid prescribing for acute pain, may be available through manufacturers’ full prescribing informationexternal iconexternal icon or consultation with other clinicians with expertise and experience in pain management. Conversion factors for drugs prescribed or provided as part of medication-assisted treatment for opioid use disorder should not be used to benchmark against MME dosage thresholds meant for opioids prescribed for pain.
References
- Centers for Disease Control and Prevention. 2018 Annual Surveillance Report of Drug-Related Risks and Outcomes — United States. Surveillance Special Report 2pdf icon. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. Published August 31, 2018.