Health
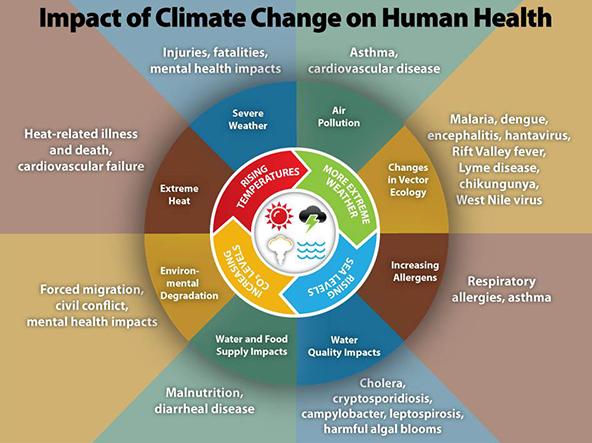
- Climate variability and change pose significant threats to human health and well-being in the United States. These climate impacts come from higher temperatures, increased extreme weather events, wildfire, decreased air quality, threats to mental health, and illnesses transmitted by food, water, and disease carriers such as mosquitoes and ticks.
- Some people are more vulnerable than others to climate impacts on health; vulnerable populations of concern include children and pregnant women, older adults, those with low income, immigrant groups, indigenous peoples, and some communities of color.
- Extreme storms and temperatures can disrupt the delivery of health services and damage hospitals, clinics, wastewater treatment plants, and other facilities. Climate also impacts economic sectors that support health, such as energy, transportation, and agriculture.
- Steps taken to prepare for climate variability and change can improve health and provide other societal benefits, such as sustainable development, disaster risk reduction, and improvements in quality of life.
Key points:
The health risks of climate change
Climate change is increasing health risks for people in the United States, including respiratory stress from poor air quality, heat stress, and the spread of diseases through food, water, and animals.1 Extreme weather events can lead to deaths, serious injuries, and lingering mental health issues such as post-traumatic stress disorder.
A number of key weather and climate factors drive human health impacts. More frequent, intense, and longer-lasting extreme heat events increase drought, wildfire, and air pollution risks.1 More frequent and extreme rain and snow, intense storms, and changes in weather patterns can produce flooding, drought, and ecosystem changes.1 Rising sea levels intensify coastal flooding and storm surges (waves that rise above normal high tide), causing injuries, deaths, stress due to evacuations or displacements, and illness due to decreased water quality, among other effects on public health. With climate variability and change, areas already experiencing weather and climate events that threaten human health are likely to experience worsening impacts, and some locations will experience new climate-related health threats.2
Climate change affects human health in two main ways—by increasing the severity or frequency of health problems already affected by climate or weather, and by creating new health problems or threats in places where they have not previously occurred.2
The subtopics in the menu at right explore some of the major climate change-related health risks facing the United States today.
People and places most at risk
A variety of factors can increase a person's vulnerability to climate change-related health impacts. Extreme weather events such as heat waves and severe storms can disrupt people’s access to clinical and public health services and food assistance programs, magnifying the stresses they may already be facing. Key factors that determine a person's or population’s risk include:
- Age — Older adults are more vulnerable to heat stress because their bodies are less able to regulate temperature. They may also have more difficulty evacuating during an extreme weather emergency. Children, who breathe more air relative to their size than adults, are also at greater risk of worsened asthma and respiratory symptoms from air pollution. More than nine percent of U.S. children live with asthma, which is the third leading cause of hospitalizations for children.3
- Underlying Physical Conditions — People with pre-existing chronic conditions, such as obesity, diabetes, heart disease, and asthma, are at increased risk for a range of climate-related health impacts. As of 2012, about half of all adults in the United States have one or more chronic conditions.3 Likewise, pregnant women, people with disabilities, and those who rely on home-based therapies, such as dialysis, are at higher risk of climate-related health impacts.
- Underlying Mental Conditions — Climate change impacts affect the social, economic, and environmental determinants of mental health. Extreme weather events can create increased anxiety and emotional stress about the future, with the most severe impacts being felt by individuals who were already disadvantaged prior to the event. Individuals who already suffer from mental health disease and stress-related disorders are at increased risk of worsened effects following extreme weather or other climate-related events.
- Socioeconomic Status — Poverty increases the risk that a population displaced by extreme weather events or environmental degradation will not easily recover and, as a result, may suffer much greater disease risks. For instance, some may be too poor to afford air conditioners or pay for the energy to run them, or to rebuild after losing their home to an extreme weather event. Extreme weather events can also lead to job loss and the loss of employer-provided health insurance.
- Communities of Color — Disparities in access to health care and a disproportionate disease burden, among other factors, make some communities of color more vulnerable to the health impacts of climate change. For instance, asthma hits some communities particularly hard. Minority populations—including African Americans, Asians, and Hispanics—are more likely to live in areas polluted by fine particle matter and ozone.4 Asthma prevalence is higher among multiracial, Hispanics, and African Americans than among whites.4 Additionally, asthma prevalence is higher among children than adults, higher among females than males, and higher among the poor than non-poor.4 The effects of climate change combined with air pollution place a disproportionate disease burden on the children in these communities.
- Location — People may face higher climate change-related health risks based on where they live or vacation. For instance, coastal lifelines, such as water supply systems, health care delivery systems, and evacuation routes, are increasingly vulnerable to higher sea levels and storm surges, inland flooding, erosion, saltwater intrusion, and other climate-related changes.5 Threats to the coast potentially affect more than half the country’s population, given that 164 million people live in coastal counties—to say nothing of the more than 180 million tourists that flock to the coasts each year.5 Urban dwellers also face disruptions in essential infrastructure services, in part because many of these infrastructures rely on one another. For example, electricity is essential to multiple systems, and a failure in the electrical grid can affect water treatment, transportation, and public health. People in rural areas may already face reduced access to health care services, which climate change-related impacts can exacerbate.
Learn more
To learn more about impacts of climate change and variability on human health, visit the subtopic pages:
- Extreme Heat—NIHHIS
- Extreme Events
- Increased Levels of Air Pollutants
- Food- and Water-Related Threats
- Changing Ecosystems and Infectious Diseases
- Building Health Care Sector Resilience
Featured Tools
Assessing Health Vulnerability to Climate Change: This document provides guidance for health departments on how to conduct a climate and health vulnerability assessment to understand the people and places in their jurisdiction that are more susceptible to adverse health impacts associated with climate change, and to implement targeted public health interventions to reduce the burden of such impacts.
Climate at a Glance: The impacts of extreme precipitation, including rainfall and snow, on health are many and varied. This tool from NOAA's National Climatic Data Center allows for near real-time analysis of monthly temperature and precipitation data across the contiguous U.S. Users can request data for select cities, states, regions, and the nation and compare current conditions with the historical record to study climate variability and change.
ClimateData.us: This tool provides users with a highly interactive means of visualizing how differences in levels of greenhouse gases may affect people and their communities. The tool uses a subset of the full climate dataset created for the Third National Climate Assessment, including the average of all 33 individual models. The tool offers projected temperature and precipitation estimates for a mitigation scenario and an increasing emissions scenario. It provides estimates of minimum and maximum daily average temperature and precipitation for four different seasons for every decade from 1950 through 2100.
Integrated Climate and Land Use Scenarios: This GIS-based tool combines county-level projections of population, housing density, and impervious surfaces to enable scientists and planners to predict how resources such as aquatic ecosystems, drinking water, and air quality might be affected under different land use and climate change scenarios.
Local Climate Analysis Tool: The tool links local weather and water events to signals in the global climate system, providing information on the effect of climate variability and change on temperature and precipitation in a given community in recent decades and how those trends may continue into the future. LCAT enables users to dive all the way into data from individual weather stations or zoom out to larger regions.
Metadata Access Tool for Climate and Health (MATCH): MATCH is a searchable clearinghouse of publicly available federal metadata (i.e., data about data) and links to datasets on both climate and health that are relevant to understanding the effects of climate change on human health.
NOAA's Weather and Climate Toolkit: As the saying goes, “A picture is worth a thousand words.” This can be especially true when trying to convey the impacts of climate and weather on communities. This toolkit provides free, platform-independent software from NOAA’s National Climatic Data Center to visualize and export climate and weather data; create maps, animations and filtering; and export images and movies in a variety of formats.
Social Vulnerability Index: Social vulnerability refers to factors such as poverty, access to transportation, and housing conditions that may affect a community’s ability to avoid human suffering and economic loss during disasters, including those related to climate change. This tool ranks U.S. census tracts (subparts of counties) on 14 variables and maps them across four themes: socioeconomic status, household composition, race/ethnicity/language, and housing/transportation. These data can be used by local officials to identify communities that may need support in preparing for hazards or in recovering from disaster.
- 1. a. b. c. Luber, G., K. Knowlton, J. Balbus, H. Frumkin, M. Hayden, J. Hess, M. McGeehin, N. Sheats, L. Backer, C. B. Beard, K. L. Ebi, E. Maibach, R. S. Ostfeld, C. Wiedinmyer, E. Zielinski-Gutiérrez, and L. Ziska, 2014: Ch. 9: Human Health. Climate Change Impacts in the United States: The Third National Climate Assessment, J. M. Melillo, Terese (T.C.) Richmond, and G. W. Yohe, Eds., U.S. Global Change Research Program, 220–256. doi:10.7930/J0PN93H5.
- 2. a. b. USGCRP, 2016: The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. A. Crimmins, J. Balbus, J. L. Gamble, C. B. Beard, J. E. Bell, D. Dodgen, R. J. Eisen, N. Fann, M. D. Hawkins, S. C. Herring, L. Jantarasami, D. M. Mills, S. Saha, M. C. Sarofim, J. Trtanj, and L. Ziska, Eds., U.S. Global Change Research Program, 312 pp.
- 3. a. b. White House Report, cited 2014: The Health Impacts of Climate Change on Americans.
- 4. a. b. c. Moorman, J.E., H. Zahran, B.I. Truman, and M.T. Molla, 2011: Current Asthma Prevalence—United States, 2006–2008. CDC Health Disparities and Inequalities Report—United States, 60, 84–86.
- 5. a. b. Moser, S. C., M. A. Davidson, P. Kirshen, P. Mulvaney, J. F. Murley, J. E. Neumann, L. Petes, and D. Reed, 2014: Ch. 25: Coastal Zone Development and Ecosystems. Climate Change Impacts in the United States: The Third National Climate Assessment, J. M. Melillo, Terese (T.C.) Richmond, and G. W. Yohe, Eds., U.S. Global Change Research Program, 579–618. doi:10.7930/J0MS3QNW.