 |

NCI Service Assists Researchers with Investigational Drug Issues
NCI-funded investigators can now turn to NCI for help with regulatory process issues as part of an effort to eliminate obstacles to the rapid development of promising new anticancer agents: Researchers can call the new NCI Regulatory Affairs Liaison.
NCI established the liaison position as a pilot program in cooperation with the Food and Drug Administration (FDA), under the NCI-FDA Interagency Oncology Task Force (IOTF). The primary purpose is to help applicants involved in the FDA's Investigational New Drug (IND) application process. IND is the FDA designation for a compound that has been submitted to FDA, has undergone a formal review process, and has been deemed appropriate for clinical testing in humans for specific indications. (Go to http://www.fda.gov/cder/regulatory/applications/ind_page_1.htm for more information.)
"Many IND application issues arise because of the complexity of the development process, the complexity of the FDA regulatory system, and a limited understanding on the part of investigators of the structure and procedures that may already exist within FDA to help resolve their problems," says Dr. Michaele Christian, NCI's co-chair of the IOTF Process Subcommittee, which developed the pilot program. However, she adds, some IND issues represent substantive scientific, medical, and regulatory disagreements that require innovative solutions.
Read more 


Guest Update by Dr. Mark Clanton
Looking Back at Katrina
Among the sad overabundance of images and news stories that emerged in the wake of Hurricane Katrina, particularly those from my hometown
of New Orleans, I'd like to single out one that spoke volumes about this tragedy. It was a plea
posted on a Katrina message board established by the American Society of Clinical Oncology (ASCO). The title: "Please help my mom." A daughter was searching for her mother's oncologist. "She has carcinoid cancer," the message read, "and I am very worried."
The cancer community came together quickly to respond to the needs of cancer patients, community oncologists, researchers, and many others affected by Katrina. As the NCI deputy in charge of coordinating NCI's response, I am very proud of our efforts during this disaster. It was especially gratifying to be part of a community-wide response, as NCI staff worked with many organizations and federal, state, and local health agencies to offer relief.
Read more 
 |
The NCI Cancer Bulletin is produced by the National Cancer Institute (NCI). NCI, which was established in 1937, leads the national effort to eliminate the suffering and death due to cancer. Through basic, clinical, and population-based biomedical research and training, NCI conducts and supports research that will lead to a future in which we can identify the environmental and genetic causes of cancer, prevent cancer before it starts, identify cancers that do develop at the earliest stage, eliminate cancers through innovative treatment interventions, and biologically control those cancers that we cannot eliminate so they become manageable, chronic diseases.

For more information on cancer, call 1-800-4-CANCER or visit http://www.cancer.gov.

NCI Cancer Bulletin staff can be reached at ncicancerbulletin@mail.nih.gov.
|
|
 |
 |

NCI Service Assists Researchers with Investigational Drug Issues
NCI-funded investigators can now turn to NCI for help with regulatory process issues as part of an effort to eliminate obstacles to the rapid development of promising new anticancer agents: Researchers can call the new NCI Regulatory Affairs Liaison.
NCI established the liaison position as a pilot program in cooperation with the Food and Drug Administration (FDA), under the NCI-FDA Interagency Oncology Task Force (IOTF). The primary purpose is to help applicants involved in the FDA's Investigational New Drug (IND) application process. IND is the FDA designation for a compound that has been submitted to FDA, has undergone a formal review process, and has been deemed appropriate for clinical testing in humans for specific indications. (Go to http://www.fda.gov/cder/regulatory/applications/ind_page_1.htm for more information.)
"Many IND application issues arise because of the complexity of the development process, the complexity of the FDA regulatory system, and a limited understanding on the part of investigators of the structure and procedures that may already exist within FDA to help resolve their problems," says Dr. Michaele Christian, NCI's co-chair of the IOTF Process Subcommittee, which developed the pilot program. However, she adds, some IND issues represent substantive scientific, medical, and regulatory disagreements that require innovative solutions.
The NCI Regulatory Affairs Liaison will first direct an investigator with an IND issue to the appropriate FDA guidance documents, regulations, or Web sites, or to the appropriate staff at FDA. The FDA staff will also be prepared to assist the clinical investigator with general questions regarding new medical products to treat cancer.
Significant issues not resolved through existing FDA procedures will be discussed by one of the IOTF subcommittees or referred to the Process Subcommittee's Senior Leadership Team.
Currently, the pilot program is limited to NCI-funded intramural and extramural investigators and investigators with approved Rapid Access to Intervention Development applications. "This joint NCI/FDA Program has been implemented so that barriers may be removed quickly and clinical studies can proceed in a timely manner," notes Dr. Christian. "It is hoped that this process will expedite the initiation of clinical studies and result in more rapid development of new agents."
For more information, go to the NCI Regulatory Affairs Liaison Web site at http://www.tech-res-intl.com/ncifdahelp/, or contact the service by phone (301-897-1705), e-mail (NCIFDAHELP@tech-res.com), or fax (301-897-1703). To initiate a request, investigators should provide their name, a summary of the nature of the IND regulatory issue, the name and number of their NCI-funded project, and the name and location of their institution. Investigators will be contacted by the NCI Regulatory Affairs Liaison if additional information is necessary.
By Bill Robinson
|
 |
 |

Guest Update by Dr. Mark Clanton
Looking Back at Katrina
 Among the sad overabundance of images and news stories that emerged in the wake of Hurricane Katrina, particularly those from my hometown
of New Orleans, I'd like to single out one that spoke volumes about this tragedy. It was a plea
posted on a Katrina message board established by the American Society of Clinical Oncology (ASCO). The title: "Please help my mom." A daughter was searching for her mother's oncologist. "She has carcinoid cancer," the message read, "and I am very worried."
Among the sad overabundance of images and news stories that emerged in the wake of Hurricane Katrina, particularly those from my hometown
of New Orleans, I'd like to single out one that spoke volumes about this tragedy. It was a plea
posted on a Katrina message board established by the American Society of Clinical Oncology (ASCO). The title: "Please help my mom." A daughter was searching for her mother's oncologist. "She has carcinoid cancer," the message read, "and I am very worried."
The cancer community came together quickly to respond to the needs of cancer patients, community oncologists, researchers, and many others affected by Katrina. As the NCI deputy in charge of coordinating NCI's response, I am very proud of our efforts during this disaster. It was especially gratifying to be part of a community-wide response, as NCI staff worked with many organizations and federal, state, and local health agencies to offer relief.
In the days immediately after the hurricane made landfall, Dr. von Eschenbach and I held conference calls with all of the directors of the NCI-designated Cancer Centers to discuss the situation and provide a conduit for those in unaffected regions to offer whatever help they could to those who needed it. A Katrina information portal was launched on the NCI Web site. NCI staff worked with ASCO and others to use the NCI Cancer Information Service's toll-free line (1-800-4-CANCER) to serve as a resource for cancer patients, many of whom were in shelters with limited access to any kind of medical care or even basic communications, to help locate their oncologists or find places where they could receive treatment.
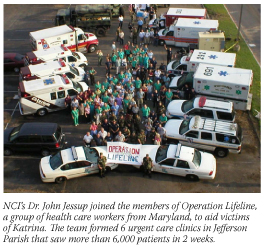 Meanwhile, 18 NCI staff - as well as staff from other organizations working on Katrina relief - were dispatched to medical facilities in the Gulf Coast. CAPT Leslie Cooper, USPHS, from the Center to Reduce Cancer Health Disparities, for example, was deployed twice and worked with officials from all levels of government to provide care to evacuees in San Antonio and New Orleans and reestablish health care systems. LCDR Mark Roth, USPHS, in NCI's Division of Cancer Epidemiology and Genetics, recently returned from deployment as part of an immunization strike team in Louisiana that administered more than 3,000 immunizations to Katrina evacuees.
Meanwhile, 18 NCI staff - as well as staff from other organizations working on Katrina relief - were dispatched to medical facilities in the Gulf Coast. CAPT Leslie Cooper, USPHS, from the Center to Reduce Cancer Health Disparities, for example, was deployed twice and worked with officials from all levels of government to provide care to evacuees in San Antonio and New Orleans and reestablish health care systems. LCDR Mark Roth, USPHS, in NCI's Division of Cancer Epidemiology and Genetics, recently returned from deployment as part of an immunization strike team in Louisiana that administered more than 3,000 immunizations to Katrina evacuees.
Approximately 7,700 patients in 318 NCI-sponsored clinical trials were affected by Katrina. To aid those involved in the trials, NCI's Cancer Therapy Evaluation Program's toll-free help line was manned 24 hours a day for a month after the hurricane. NCI also worked with other institutions to offer researchers at affected centers temporary placement to continue or, in some cases, resurrect their work.
We are continuing to learn important lessons from this experience. Some are simple things, such as having up-to-date contact information for essential staff. Some require a more substantial effort, such as the need for a portable medical record for cancer patients enrolled in clinical trials.
Many more people than can be named here were involved in the response by NCI and the entire cancer community to this disaster. On behalf of NCI, I thank them for their outstanding and selfless work.
|
 |
 |

Communicating About Cancer Pain
Pain can be a harsh reality of cancer. Cancer pain can be caused by a tumor or related to treatment such as radiation and chemotherapy. When surgery is indicated, postsurgical pain is also a consideration.
Studies show that anywhere from 30 to 50 percent of patients who undergo active treatment for cancer and 70 percent of those with advanced stages of the disease experience significant pain and may be reluctant to discuss their pain with their doctors.
Not all pain experienced by cancer patients is due to the cancer itself. "About 75 percent of the pain encountered in cancer patients is due to the cancer, while the balance results from treatments and procedures, such as neuropathic pain following a mastectomy," said Dr. Ann Berger, chief of the Pain and Palliative Care Service at the National Institutes of Health Clinical Center. "Cancer patients might also have migraine headaches, arthritis, or other medical conditions unrelated to their cancer that also need to be treated."
Clinicians have designed scales to help patients communicate their pain levels. If the pain is described as shooting down a leg or a tingling sensation in the hands or feet, this information can be crucial to determining the appropriate therapy. "A significant advance is that the Joint Commission on Accreditation of Healthcare Organizations now requires physicians to ask patients about pain," noted Dr. Berger. "Pain is now the fifth vital sign, like blood pressure and temperature. Physicians are required to ask patients more often about their pain."
"Patients have also stated that they don't discuss pain symptoms for fear that it will distract from talking about treating their disease," said Dr. Ann O'Mara, a program director at NCI's Division of Cancer Prevention. "Patients can be hesitant to discuss their pain due to fear that the pain is a sign that the cancer has returned."
NCI is sponsoring research that examines the barriers that prevent patients from talking about pain and their symptoms. "Patients must become empowered. When it comes to pain and symptom management, they have an important role," commented Dr. O'Mara.
In one study, researchers developed an assessment questionnaire to help patients report their symptoms. The study's goal is to determine the most effective method of enabling patients and doctors to broach the subject of pain, resulting in improved symptom management.
NCI is attempting to dispel the many myths about cancer and pain. One prevalent belief is that cancer is always associated with chronic, unrelieved pain. While many cancer patients will experience some level of pain during or after their treatment, it can be relieved in 80 to 85 percent of patients. The remaining 15 to 20 percent experience pain that can be difficult to resolve. But, even the most intractable pain can be relieved to some degree.
Another common belief - held by many cancer patients, their families, and some physicians - is that treating cancer patients for pain can lead to addiction. "Many people misunderstand the difference between addiction and physical dependence," noted Dr. O'Mara. "Addiction is a chronic, psychological state with contributing genetic and environmental factors. It is characterized by impaired control over drug use, compulsive use, craving, and continued use despite harm. Physical dependence, on the other hand, is an expected outcome with chronic use of narcotics. When the drug is abruptly withdrawn, a patient may experience specific physical reactions. However, after treatment and the cancer resolves, the dose of pain medication should be slowly decreased, enabling a patient to withdraw from the drug without side effects."
Treating pain requires constant reassessment. Clinicians should ask specific questions of their patients. It may not be sufficient to just ask, "How are you doing today?" For proper assessment, clinicians need to help patients verbalize the impact that pain is having on their daily lives. Dr. O'Mara suggested more specific questions, such as, "How have you been sleeping, what is the level of your fatigue, or how is pain affecting your work routine?"
"Just giving a pain medication is not enough. There must be continuous discussion with the patient to determine how the medication is working and how they are coping," concluded Dr. O'Mara.
By Lynette Grouse and
Dorie Hightower
|
 |
 |
Race Influences Decisions on Lung Cancer Surgery
African American patients who are offered surgery to treat early-stage lung cancer are far more likely than white patients to reject the offer, researchers at Henry Ford Health System (HFHS) are reporting. The finding is significant, the researchers write in the November 2005 issue of Chest, because chances of 5-year survival are as high as 50 percent in patients with early-stage disease who are treated with surgery, whereas the median survival is less than 1 year for those who decline surgery.
The result was consistent with previous studies indicating that African American lung cancer patients are less likely to undergo surgery; as a result, their mortality rates are higher than those among whites.
The study was a retrospective analysis of 97 African American patients and 184 white patients treated at the Josephine Ford Cancer Center in Detroit who were enrolled in the center's lung cancer registry. Data from patients enrolled in the HFHS pulmonary clinic between 1995 and 1998 were analyzed. Of those who were offered surgery, 18 percent of African American patients declined, compared with only 5 percent of white patients. Surgery was offered to 78 percent of white patients and 70 percent of African American patients. Of that group, 74 percent of white patients underwent the procedure, compared with 58 percent of African American patients.
"Knowing blacks decline surgery at a higher rate than whites is the first step to decreasing lung cancer mortality among this population," said the study's lead investigator, Dr. Bruno DiGiovine.
The authors hypothesized that, in addition to factors such as lack of trust in the health care system, the higher rate of decline may be linked to reports in previous studies, which found that African Americans are far more likely than whites to believe that surgery to treat lung cancer can actually cause the disease to metastasize.
Prevention Could Cut Worldwide Cancer Deaths by One-Third
Screening and treatment are the two primary approaches against cancer that receive the most money and attention, but a new global meta-analysis shows that about 2.5 million cancer deaths each year can be attributed either to modifiable behavior or environmental factors. If societies were able to implement changes at the population level, a substantial proportion of these deaths could be prevented.
Addictive substances - smoking and alcohol - were the most lethal of the nine modifiable risk factors examined. The other seven risk factors were grouped by diet/physical activity (excess weight, physical inactivity, and low consumption of fruits and vegetables); environmental risks (urban air pollution and indoor smoke, primarily from burning coal); unsafe sex (which transmits human papillomavirus [HPV] infections that cause cervical cancer); and contaminated injections in health care settings (which can cause liver cancer).
Working from published meta-analyses and systematic reviews, researchers determined that 35 percent of the 7 million global cancer deaths in 2001 were attributable to all of the risk factors combined, with more than two-thirds of these occurring in low- and middle-income regions. Nearly twice as many men as women died from preventable cancers. Of all cancer deaths, 41 percent of men's deaths were attributable to the modifiable risk factors, compared with 27 percent of women's deaths.
In high-income countries, the most prevalent causes of cancer are smoking, alcohol use, and overweight/obesity; 52 percent of preventable deaths are from lung cancer, followed by 6 percent each from esophageal and stomach cancer. In low- and middle-income countries, the most common preventable deaths are caused by lung cancer (31 percent), liver cancer (14 percent), and breast and esophageal cancer (13 percent each).
Smoking alone causes 21 percent of all cancer deaths worldwide. Analysis shows that modifying risk factors could reduce three types of cancer by more than 60 percent: esophageal cancer by 62 percent and lung cancer by 74 percent; cervical cancer could be completely eliminated if safe sex practices stopped the spread of HPV infections.
The study was published in the November 19 Lancet by Dr. Majid Ezzati and colleagues at the Harvard School of Public Health, and is the latest result from the Comparative Risk Assessment Collaborating Group (Cancers), a worldwide network of expert working groups that has previously published comparable analyses for other diseases.
Retinoid Resistance in Lung Cancer
Results from many laboratory studies suggested that retinoids - vitamin A and its natural and synthetic analogues - have potential anticarcinogenic activity. However, clinical trials using these compounds to prevent lung cancer have shown universally disappointing results. Loss of retinoic acid receptors (RAR) during carcinogenesis and disruption of the RA cellular signaling pathway may confer some of the observed resistance.
Expression of receptors in the RARβ family is frequently decreased in lung cancer cells. A study, conducted by researchers at Wake Forest and Dartmouth Universities, funded in part by NCI, and reported in the November 16 Journal of the National Cancer Institute, uncovered a previously unknown isoform of RARβ that may play a major roll in lung cancer retinoid resistance. This isoform, named RARβ1', was expressed in normal lung cells and in an RA-sensitive immortalized human bronchial epithelial (HBE) cell line, but not in RA-resistant HBE cells, lung cancer cell lines, or clinical lung cancer samples.
After transfection of an RA-resistant lung cancer cell line with RARβ1', RA treatment suppressed cell growth. Nontransfected cells were not affected by RA treatment. Treatment of another RA-resistant cell line with exogenous RARβ1' also led to growth suppression. Again, control cells were not affected by RA treatment. Investigators concluded that RARβ1' likely plays an important role in retinoid signaling and loss of the isoform that contributes to lung carcinogenesis.
"RARβ1' repression, despite RA treatment, offers a mechanistic explanation for clinical retinoid resistance that has been reported previously," wrote the investigators. "Identification of pharmacologic approaches that restore RARβ1' expression would provide a basis for future retinoid-based combination strategies for lung cancer therapy or chemoprevention."
Nanoparticles Track Cancer Vaccines
Nano-sized particles of iron oxide can be used as tags to label immune-stimulating cells for visualization with magnetic resonance imaging (MRI), according to a new report in the November Nature Biotechnology. The research promises to speed development of cancer vaccines and other immune-boosting strategies, according to an international team of researchers.
Since the debut of immunotherapy for cancer in the mid-1990s, researchers have struggled with delivering dendritic cells to lymph nodes, which is critical for their ability to enhance an immune response. Until now, there has been no accurate way to monitor their location. The team of investigators found that they were better able to assess advanced melanoma patients whose injected dendritic cells reached the target site, utilizing the FDA-approved iron-oxide nanoparticles and MRI, compared with utilizing standard scintigraphic imaging. Using this new procedure may facilitate studies to optimize inoculation procedures, immune response, and vaccination schedules.
"We show that magnetic resonance tracking of magnetically labeled cells is a clinically safe procedure that, because of its high resolution and excellent soft tissue contrast, appears ideally suited to monitor novel experimental cell therapies in patients," says the study's first author, Jolanda de Vries, from Radboud University Nijmegen Medical Center in The Netherlands.
|
 |
 |

 |
 |
CCR Grand Rounds |
 |
|
December 6: Dr. Steven Pavletik, Head, Graft-Versus-Host and Autoimmunity Unit, Experimental Transplantation and Immunology Branch; Acting Chief, Medical Oncology Transplantation and Immunotherapy Service, NCI. "Addressing Challenges in Clinical Research: The Model of Chronic Graft-versus-Host Disease"
December 13: Dr. Joan Massague, Chairman, Cancer Biology and Genetics Program, Howard Hughes Medical Institute, Memorial Sloan-Kettering Cancer Center. Lecture title TBD.
There will be no lecture on December 20 or 27. CCR Grand Rounds will resume on Tuesday, January 10, 2006.
CCR Grand Rounds are held 8:30 to 9:30 a.m. at the NIH campus in Bethesda, Md., in the Clinical Center's Lipsett Amphitheater.
|
|
NIH Director's Pioneer Award Program
RFA-RM-06-005
Application Receipt Date: Feb. 27, 2006.
This funding opportunity will use the DP1 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3295. Inquiries: Dr. Judith H. Greenberg - pioneer@nih.gov
Image-Guided Cancer Interventions (STTR [R41/R42])
PA-06-031
Application Receipt Dates: New applications: Dec. 1, 2005; April 1 and Aug. 1, 2006.
This is a renewal of PA-04-063. This funding opportunity will use the R41 and R42 award mechanisms. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3292. Inquiries: Dr. Keyvan Farahani - farahank@mail.nih.gov; Dr. Laurence P. Clarke - lclarke@mail.nih.gov
Image-Guided Cancer Interventions (STTR [R43/R44])
PA-06-032
Application Receipt Dates: New applications: Dec. 1, 2005; April 1 and Aug. 1, 2006.
This is a renewal of PA-04-063. This funding opportunity will use the R43 and R44 award mechanisms. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3293. Inquiries: Dr. Keyvan Farahani - farahank@mail.nih.gov; Dr. Laurence P. Clarke - lclarke@mail.nih.gov
Research on Clinical Decision Making in Life-Threatening Illness
PA-06-077
Application Receipt Dates: New applications: Feb. 1, June 1, and Oct. 1, 2006; Feb. 1, June 1,
and Oct. 1, 2007; Feb. 1, June 1, and Oct. 1,
2008. Competing continuation, revised, supplemental applications: March 1, July 1, and Nov. 1, 2006; March 1, July 1, and Nov. 1, 2007; March 1, July 1, and Nov. 1, 2008.
This is a renewal of PA-02-118. This funding opportunity will use the R01 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3294. Inquiries: Dr. Wendy Nelson - nelsonw@mail.nih.gov
|
 |
 |

Combination Chemotherapy for Liver Cancer
Name of the Trial
Phase II Study of Doxorubicin and Bortezomib in Patients with Hepatocellular Carcinoma (ECOG-E6202). See the protocol abstract at http://cancer.gov/clinicaltrials/ECOG-E6202.
 Principal Investigators
Principal Investigators
Dr. Jordan Berlin, Dr. Bruce Giantonio, and Dr. William Chapman, Eastern Cooperative Oncology Group
Why Is This Trial Important?
Hepatocellular carcinoma (liver cancer) is expected to kill more than 15,000 Americans in 2005. Surgery is the only known curative treatment for this type of cancer, but fewer than 20 percent of patients are eligible for surgery. Although some patients may benefit from local treatments other than surgery, most patients with inoperable liver cancer are treated with systemic chemotherapy.
Treatment with the drug doxorubicin has provided the best results so far for liver cancer patients with inoperable tumors. Unfortunately, fewer than 20 percent of patients respond to treatment with doxorubicin. In this clinical trial, researchers are adding a new drug called bortezomib to chemotherapy with doxorubicin to see if it can cause liver tumors to shrink or stop growing better than doxorubicin alone. Bortezomib, a proteasome inhibitor, blocks the activity of a number of proteins important for cell survival, tumor growth, and angiogenesis (the formation of new blood vessels to the tumor). In other types of cancer, bortezomib has been shown to delay tumor growth and enhance the cell-killing effects of chemotherapy.
"Results from our laboratory studies suggest that combining doxorubicin and bortezomib is more effective against liver cancer than either agent alone," said Dr. Berlin. "We hope that by adding bortezomib to the standard treatment for liver cancer, we can better control this difficult-to-treat disease."
Who Can Join This Trial?
Researchers seek to enroll 40 patients aged 18 and over with a confirmed diagnosis of hepatocellular carcinoma that is not amenable to curative surgery. See the list of eligibility criteria at http://cancer.gov/clinicaltrials/ECOG-E6202.
Where Is This Trial Taking Place?
Study sites in the United States are recruiting patients for this trial. See the list of study sites at http://cancer.gov/clinicaltrials/ECOG-E6202.
Contact Information
See the list of study contacts at http://cancer.gov/clinicaltrials/ECOG-E6202 or call NCI's Cancer Information Service at 1-800-4-CANCER (1-800-422-6237). The toll-free call is completely confidential.
An archive of "Featured Clinical Trial" columns is available at http://cancer.gov/clinicaltrials/ft-all-featured-trials.
|
 |
 |
 |
 |
Featured Meetings and Events |
 |
|
Molecular Imaging Probes Described
The November 15 Clinical Cancer Research includes a comprehensive review of a technology called molecular imaging probes and their use in the development of cancer drugs. The article, "The Progress and Promise of Molecular Imaging Probes in Oncologic Drug Development," is the second in a series of publications written by members of the NCI-FDA IOTF. The authors review the state of the science, discuss clinical applications of imaging probes, and make recommendations for advancing the field in the future. The first article in the IOTF series, "Progress and Promise of FDG-PET Imaging for Cancer Patient Management and Oncologic Drug Development," appeared in the April 15 Clinical Cancer Research.
Workshop Addresses Cancer Health Disparities
On November 17-18, virtually all of the top leadership joined more than 200 employees for the first NCI-wide meeting on one of the central issues of the day, "Enhancing Interactions to Reduce Cancer Health Disparities." Program co-chair Dr. Leonora Johnson, director of the Office of Education and Special Initiatives, told the group they were there to help "build synergy around NCI efforts to reduce disparities by enhancing our communications, stimulating our interactions across NCI, and trying hard to leverage our strengths through information sharing and increasing collaboration."
Dr. Mark Clanton, deputy director, NCI, and deputy director for Cancer Care Delivery Systems, remarked that the gathering was another important step toward reducing cancer health disparities, which was recently named one of NCI's seven strategic priorities for reaching the 2015 challenge goal.
Dr. John Niederhuber, deputy director, NCI, and deputy director for Translational and Clinical Sciences, added that "we will not be able to meet those challenges down the road, unless we first solve this crucial issue along the way." He predicted that, in just the next decade, the face of medicine will change dramatically, mediated by new technologies for screening, detection, and genomics. "If we don't figure out how to translate this new era to these special populations, they will be left even further behind. It's a challenge we have to meet…and we will," he said.
Teleconference Focuses on NIH Clinical Center
The next teleconference in the "Understanding NCI" series will take place on December 16 at 1:00 p.m. EST. Interested individuals should call 1-800-857-6584 (Passcode: 4683#). Toll-free playback will be available until 11:30 p.m. EST on Jan. 16, 2006, at 1-800-216-4418.
This teleconference will focus on the NIH Clinical Center and describe how cancer patients participate in clinical research to find new treatments for cancer at NIH's world-renowned research hospital.
Dr. John Gallin, director of the NIH Clinical Center; Dottie Cirelli, Clinical Center patient recruitment coordinator; and Susan Lowell Butler, patient advocate; will discuss clinical trials at NCI. A question and answer session will follow the panelists' presentations.
The "Understanding NCI" teleconference series is sponsored by the NCI Office of Liaison Activities. For additional information, go to http://la.cancer.gov.
Watch Your E-Mail Box!
Keep an eye out for an e-mail later this week asking you to complete an online survey about the NCI Cancer Bulletin.
Since its debut in January 2004, the NCI Cancer Bulletin has provided its readers with a weekly roundup of news from the cancer community - from research highlights to clinical trials to community updates. From December 1-22, you'll have the opportunity to tell us how we're doing by completing an online reader survey.
By completing this short questionnaire, you'll help us to better meet the needs of our readers. Your feedback is vital in shaping future issues of the Bulletin.
All survey responses are confidential and respondents can choose to answer or skip any questions in the survey. For more information, please contact Nina Goodman at goodmann@mail.nih.gov or 301-435-7789.
Special Issue on NCI Training Opportunities
Don't miss next week's NCI Cancer Bulletin, which will highlight training programs at NCI. This special issue will include features about training opportunities in basic, clinical, and population sciences; a comprehensive list of NCI's training resources; and a conversation with John Burklow, a former NCI intern who is now associate director of the NIH Office of Communications.
|
|
 |
 |

Vanderbilt-Ingram Cancer Center
Director: Dr. Raymond N. DuBois • 691 Preston Building, Vanderbilt University, Nashville, TN 37232-6838 • Phone: 615-936-1782 • Web site: http://www.vicc.org
 Background
Background
Vanderbilt-Ingram Cancer Center was established in 1993 as the umbrella organization over cancer-related research, clinical care, and education at Vanderbilt University Medical Center. Under the leadership of its founding director, Dr. Harold L. Moses, the center was awarded a Cancer Center Support Grant in 1995 and has remained continuously funded since then. In 2001, Vanderbilt-Ingram was designated as a Comprehensive Cancer Center, making it the only such center in Tennessee. In 2005, Dr. Moses was succeeded by Dr. Raymond N. DuBois as director. As director emeritus, Dr. Moses continues as a senior scientist and advisor.
Patient Care
Vanderbilt-Ingram Cancer Center emphasizes individualized cancer care developed and delivered through a comprehensive, multidisciplinary team approach, with particular strengths in lung, gastrointestinal, breast, and head and neck cancers, as well as melanoma and sarcoma. Pediatric cancer care is delivered in the Monroe Carell Jr. Children's Hospital at Vanderbilt, listed among the top 10 children's hospitals in the country by Child magazine. Vanderbilt-Ingram offers more than 200 clinical trials for adults and children at its main campus and through 15 members of its affiliate network in Tennessee, Kentucky, and Georgia.
Research
Vanderbilt-Ingram Cancer Center's research enterprise emphasizes translational research and builds on a strong legacy of basic science in growth factors and signal transduction. It includes seven formal research programs covering the areas of signal transduction and cell proliferation, host-tumor interaction, gastrointestinal cancer, breast cancer, genomics and proteomics, cancer prevention and control, and experimental therapeutics. Since its inception, competitive NCI grant funding has grown to more than $50 million per year; total annual research funding, including private sources, tops $130 million. Vanderbilt-Ingram is home to three NCI Specialized Programs of Research Excellence in breast, gastrointestinal, and lung cancers; a Digestive Disease Center; and a Mouse Models of Human Cancer Consortium grant.
Other Notable Programs
Through the Meharry-Vanderbilt Alliance, Vanderbilt-Ingram and its neighbor, Meharry Medical College, are working together to understand and address health disparities in cancer through collaborative research, education, and clinical care initiatives. This work includes the Southern Community Cohort Study, enrolling more than 100,000 people (two-thirds of them African American) in clinical trials with the goal of eliminating the racial and regional gaps in cancer incidence and mortality.
Vanderbilt-Ingram has developed a strong program in patient and community education, reaching thousands of community members with prevention and awareness information each year. This effort includes initiatives to assist patients and caregivers in making informed decisions about their care, such as a Patient Resource Center and the Cancer Information Program, a toll-free service staffed by oncology nurses to assist patients, families, and referring physicians with cancer information and to facilitate second opinions and clinical trials accrual.
|
 |
|