 |
|
 |

Treatment for Advanced Liver Cancer Increases Survival
The targeted drug sorafenib 1 (Nexavar) has improved the survival of patients with advanced liver cancer, a fatal disease that is becoming more common worldwide.
The final-stage, randomized study 2 found that patients taking sorafenib lived nearly 3 months longer than patients taking a placebo. This was clinically significant, and the trial was stopped early because preliminary results clearly favored sorafenib. Read more 3 


ASCO 2007: Steady Progress Against Cancer
On June 1-5, Chicago played host to this year's American Society of Clinical Oncology (ASCO) meeting. This year set an attendance record with more than 30,000 participants. Throughout the meeting one sensed the excitement of steady, continued progress. There was also anticipation of even greater changes that will occur in the coming years as laboratory science is enabled by new and rapidly evolving technology. The anticipation was clearly about earlier diagnosis, new and reliable biomarkers, highly characterized tumors, and more targeted therapies.
For example, as the lead story in this issue of the NCI Cancer Bulletin discusses in greater detail 3, a phase III European clinical trial found that, compared with placebo, the multitargeted agent sorafenib 1 (Nexavar) improves survival in advanced hepatocellular carcinoma (HCC). There was a small, but statistically significant, improvement, marking the first time a systemic treatment has proven effective against advanced HCC, a notoriously intractable disease that is increasing in incidence in the U.S. The result clearly sets the stage for further trials testing sorafenib in combination with other targeted agents to treat HCC. Read more 4 
 |
The NCI Cancer Bulletin is produced by the National Cancer Institute (NCI). NCI, which was established in 1937, leads the national effort to eliminate the suffering and death due to cancer. Through basic, clinical, and population-based biomedical research and training, NCI conducts and supports research that will lead to a future in which we can identify the environmental and genetic causes of cancer, prevent cancer before it starts, identify cancers that do develop at the earliest stage, eliminate cancers through innovative treatment interventions, and biologically control those cancers that we cannot eliminate so they become manageable, chronic diseases.

For more information on cancer, call 1-800-4-CANCER or visit http://www.cancer.gov.

NCI Cancer Bulletin staff can be reached at ncicancerbulletin@mail.nih.gov. |
|
 |
 |

Treatment for Advanced Liver Cancer Increases Survival
The targeted drug sorafenib 1 (Nexavar) has improved the survival of patients with advanced liver cancer, a fatal disease that is becoming more common worldwide.
The final-stage, randomized study 2 found that patients taking sorafenib lived nearly 3 months longer than patients taking a placebo. This was clinically significant, and the trial was stopped early because preliminary results clearly favored sorafenib.
"For the first time we have a drug that works for these patients," said Dr. Joseph Llovet of the Mount Sinai School of Medicine and the University of Barcelona. He presented the results June 4 at the American Society of Clinical Oncology (ASCO) annual meeting.
Sorafenib is a pill that patients can take at home. The drug, which is approved for kidney cancer, was well tolerated by the 602 patients in the international study. The most common side effects included diarrhea and skin reactions in the hands and feet.
Dr. Llovet noted that there have been more than 100 unsuccessful clinical trials for advanced liver cancer in the last 30 years. Surgery and chemotherapy are used to treat patients in the earlier stages of disease, but there has been no successful "systemic" treatment, such as a drug, for advanced cases.
Sorafenib will now become the standard treatment for patients with advanced liver cancer, and having this regimen as a platform will accelerate clinical trial efforts to identify other agents, said Dr. A. William Blackstock of the Wake Forest University School of Medicine at the meeting.
Until now, experimental therapies for liver cancer have been compared with placebos. Many patients, particularly in the U.S., are reluctant to join clinical trials if they have a 50-percent chance of receiving a sugar pill. Participation in trials may now increase, with sorafenib replacing placebos as the standard control.
"We can now move forward in this disease," said Dr. Blackstock.
The next steps include testing sorafenib earlier in the disease and eventually in combination with other targeted therapies. Bevacizumab 5 (Avastin), erlotinib 6 (Tarceva), and sunitinib 7 (Sutent) have all been tested for liver cancer in phase II studies.
Like these drugs, sorafenib interacts with a small number of proteins. The drug inhibits cell growth and the formation of blood vessels that feed tumors (angiogenesis).
Liver cancer is the fifth most common cancer and the third leading cause of cancer death worldwide. The disease is most prevalent in the developing world, but it appears to be increasing in the U.S. and Europe.
In the trial, the sorafenib group lived on average 10.7 months compared with 7.9 months for the placebo group - a more than 40-percent improvement in survival time.
Sorafenib is the "first convincing and rigorously tested treatment" to show a survival benefit for these patients, said Dr. Philip James Johnson of the Institute for Cancer Studies at Birmingham University in the U.K., who discussed the results in a special session at ASCO.
Dr. Johnson cautioned that it is not yet known how the drug might perform in different ethnic groups and in patients with poor liver function. Most participants were European and had relatively good liver function.
Nonetheless, he concluded, the study marks "the dawn of a new era" in the treatment of liver cancer.
- Edward R. Winstead
|
 |
 |

ASCO 2007: Steady Progress Against Cancer
On June 1-5, Chicago played host to this year's American Society of Clinical Oncology (ASCO) meeting. This year set an attendance record with more than 30,000 participants. Throughout the meeting one sensed the excitement of steady, continued progress. There was also anticipation of even greater changes that will occur in the coming years as laboratory science is enabled by new and rapidly evolving technology. The anticipation was clearly about earlier diagnosis, new and reliable biomarkers, highly characterized tumors, and more targeted therapies.
For example, as the lead story in this issue of the NCI Cancer Bulletin discusses in greater detail 3, a phase III European clinical trial found that, compared with placebo, the multitargeted agent sorafenib 1 (Nexavar) improves survival in advanced hepatocellular carcinoma (HCC). There was a small, but statistically significant, improvement, marking the first time a systemic treatment has proven effective against advanced HCC, a notoriously intractable disease that is increasing in incidence in the U.S. The result clearly sets the stage for further trials testing sorafenib in combination with other targeted agents to treat HCC.
Also impressive was a larger, phase III clinical trial that showed a significant treatment benefit 8 against another difficult to treat disease, small-cell lung cancer (SCLC). Using prophylactic cranial irradiation, or PCI, in patients with extensive SCLC who had responded to chemotherapy, not only was the risk of symptomatic brain metastases reduced compared to those not receiving PCI, but there was a highly significant survival improvement at one year. There seemed to be consensus at the meeting that this finding should immediately change clinical practice.
After demonstrating particularly powerful prognostic prowess 9 in metastatic breast cancer, new data presented at ASCO suggested that levels of circulating tumor cells (CTCs) - tumor cells circulating freely in blood - in men with metastatic, hormone-refractory prostate cancer are predictive of prognosis and response to chemotherapy. This new study also suggests CTC levels may be a better surrogate of treatment efficacy than PSA levels.
During the meeting, preliminary data 10 were presented from the first prospective, multicenter phase II clinical trial in the U.S. testing gefitinib 11 (Iressa) as a first-line therapy in patients with advanced non-small-cell lung cancer with genetic mutations known to correspond with gefitinib response. The initial findings demonstrated strong progression-free survival, and the estimated median overall survival of approximately 21 months would be a significant improvement compared with historical rates. The trial, called iTARGET, represents an important step toward more individualized treatment.
Finally, it is important to touch on the results of a small, but entirely new type of clinical trial being pioneered at NCI that we believe will ensure promising agents get translated to the clinic more quickly and efficiently than in the past. Following new FDA guidance 12 released last year - and developed with the aid of the FDA-NCI Interagency Oncology Task Force - this "early phase I trial 13" involved only six patients. It tested an inhibitor of an enzyme called PARP that plays a critical role in DNA repair. Assays developed as part of the trial showed that the agent, ABT-888, was hitting its intended target in tumor cells, as well as in white blood cells, suggesting that future early-phase trials of the drug can use white blood cells as biomarkers of the compound's effectiveness.
Just before the ASCO meeting began, NCI's Scientific Director for Clinical Research, Dr. Lee Helman, participated in a meeting with the Sarcoma Alliance for Research through Collaborations to review the findings from phase I clinical trials testing investigational monoclonal antibodies that inhibit IGF-1R, including some extremely promising results seen in patients with Ewing's sarcoma, a cancer rare in adults but common in children. In some cases, there have been complete responses in patients with refractory, progressive disease who had failed multiple therapies. Based on these results, several phase II studies have been planned, at least one of which is scheduled to launch in the fall. I am very hopeful that positive results of these trials may be presented at future ASCO meetings.
This year's ASCO meeting demonstrated the important progress being made against different cancer types through varied approaches. It demonstrates how we are learning to design better trials and take advantage of new technologies. Most important, it confirms that we are improving outcomes for more and more people who receive a cancer diagnosis.
Dr. John E. Niederhuber
Director, National Cancer Institute |
 |
 |
Folic Acid Study Shows Surprising Results
A study 14 that set out to test folate for prevention of early-stage colon cancer instead found a higher incidence of colorectal adenomas in the test group. This multi-institutional NCI-funded research, performed by the Polyp Prevention Study Group, appeared in the June 6 Journal of the American Medical Association.
The cohort included 987 people who had a history of colorectal adenomas, precursor lesions for cancer. Half of these people received 1 mg/day of folic acid and the other half received a placebo. The average person gets about 0.2 - 0.4 mg of daily folate in their diet. Participants were monitored with colonoscopies after 3 and 5 years.
With an average follow-up of 3 years, colorectal adenomas occurred in 42.4 percent of participants who received the placebo and in 44.1 percent of those who received folic acid. At the 5-year follow-up, participants in the folic acid group also had higher rates of advanced lesions and greater numbers of lesions than the control group.
An accompanying editorial speculates that the most likely explanation for this increase in advanced lesions (known precursors to colorectal cancer) is that they are promoted by increased folate.
The editorial also notes that a history of colorectal adenomas was a prerequisite for inclusion in the study, and the endpoint was whether additional adenomas formed, not whether cancer was prevented in this high-risk group. "The question of efficacy of folate in cancer prevention is not resolved…Animal experiments showing chemopreventive effects of folate, as well as the strong observational epidemiological evidence, speak to [its] potential…if taken early," the editorialists wrote.
Meta-Analysis Suggests Cisplatin Superior to Carboplatin for Advanced NSCLC
Cisplatin 15 is likely a better option than carboplatin for patients with advanced-stage non-small-cell lung cancer (NSCLC), according to a meta-analysis of nine randomized clinical trials comparing the two drugs.
The analysis, which involved data on nearly 3,000 individual patients, revealed a superior response rate in patients with NSCLC treated with a cisplatin-based chemotherapy regimen compared with carboplatin-based regimens, and a small but statistically significant improvement in overall survival in patients with nonsquamous NSCLC and those in whom cisplatin was combined with so-called third-generation chemotherapy drugs, such as gemcitabine 16, paclitaxel 17, and docetaxel 18.
"The superiority of cisplatin over carboplatin was not achieved at the cost of a statistically significant increase in the incidence of severe side effects," wrote lead author Dr. Andrea Ardizzoni, of University Hospital in Parma, Italy, and colleagues in the June 6 Journal of the National Cancer Institute (JNCI). They reported that, while cisplatin-based regimens were associated with a greater incidence of high-grade nausea, vomiting, and kidney problems, carboplatin was associated with more drastic drops in platelet counts (thrombocytopenia).
Based on clinical trial results, the two drugs have been considered to be equally effective in treating advanced NSCLC, and U.S. oncologists have favored carboplatin because it has been associated with fewer side effects and is easier to administer.
In an accompanying editorial in JNCI, Dr. Christopher G. Azzoli, from Memorial Sloan-Kettering Cancer Center, and colleagues noted that more effective antinausea medications could help to decrease cisplatin's toxicity burden. They also cited cisplatin's increased effectiveness in patients with nonsquamous disease, which they argued was particularly important given the success 19 seen in a recent U.S. phase III study in the same patient population treated with a combination of the targeted agent bevacizumab 5 (Avastin) and carboplatin and paclitaxel.
Overall, the editorial states, "the apparent superiority of cisplatin over carboplatin…should not be taken lightly, particularly in patients being treated with a curative intent."
Meanwhile, a European phase III trial presented 20 at the ASCO annual meeting found that combining bevacizumab with cisplatin and gemcitabine provides a slight improvement - less than a month - in median progression-free survival compared with chemotherapy alone.
|
 |
 |
Preventive Radiation Reduces Lung Cancer Brain Metastases
According to results recently presented at the ASCO annual meeting, prophylactic cranial radiation following treatment with chemotherapy doubles survival at 1 year and reduces the risk of developing brain metastases among patients with extensive-disease small-cell lung cancer (SCLC).
About 70 percent of SCLC patients have disease that has already spread extensively at the time of their diagnosis, and a significant number of patients develop brain metastases. Previous studies have shown that prophylactic cranial irradiation (PCI) prevents brain metastases and improves survival in SCLC patients who have local disease and a complete response to initial chemotherapy. New results presented at the ASCO meeting indicate that this strategy remains sound, even when SCLC has spread extensively.
Findings were presented by lead author Dr. Ben Slotman of the VU University Medical Center in Amsterdam. The trial randomized 286 patients who had responded to 4 to 6 cycles of chemotherapy to observation or PCI consisting of 20 to 30 Gy administered in 5 to 12 fractions. At 1 year, symptomatic brain metastases occurred in 14.6 percent of patients treated with cranial radiation compared with 40.4 percent of patients in the observation group. Survival was doubled at 1 year for patients treated with cranial radiation compared with those in the observation group (27.1 versus 13.3 percent, respectively). Radiation was well tolerated and the most common side effects were headache, nausea and vomiting, and fatigue.
Children Survive Neuroblastoma with Less Intensive Treatment
On Sunday, June 3, researchers from the Children's Oncology Group presented results at the ASCO annual meeting from a multinational study showing that a treatment regimen more patient-friendly than the current standard can achieve comparable survival rates among infants and children with intermediate risk neuroblastoma.
Researchers substituted carboplatin for cisplatin, a drug that can cause long-term side effects such as hearing loss, in the multi-agent drug treatments that they administered to study patients. They also reduced the length and number of cycles so that patients received 10 to 18 days of treatment over an 84- to 168-day period, as opposed to the standard 71 days of treatment over 286 days. The researchers compared the survival rate achieved by the new treatment with that observed for prior clinical trials of standard treatments.
After an average follow-up of 3 years, survival among the 467 infants and children was 96 percent, which is comparable to or better than that seen in large trials of standard treatment. Furthermore, less than 2 percent of the patients had major damage to their heart, kidney, liver, or hearing - a better than usual outcome.
"The paradigm we are continually striving for is to cure as many children as possible while reducing the burden of treatment," said the study's lead author, Dr. David Baker of Princess Margaret Hospital for Children in Perth, Australia, in an ASCO press briefing. "This goes a long way toward meeting that goal."
Kidney Cancer Patients Benefit from Avastin
Bevacizumab 5 (Avastin) is the fourth targeted drug in recent years to help patients with advanced kidney cancer, a disease that historically has been difficult to treat. A final-stage, randomized trial 21 presented at the ASCO annual meeting found that the combination of bevacizumab and interferon was more effective than interferon and placebo. Adding bevacizumab nearly doubled the time the disease took to progress - from 5.4 months to 10.2 months - without creating significant new toxicities.
Interferon was the standard treatment for advanced kidney cancer when the trial began. But last year three targeted drugs - sunitinib 7 (Sutent), sorafenib 1 (Nexavar), and temsirolimus 22 (Torisel) - emerged as the first new kidney cancer medicines in two decades, changing the standard of care. The new results demonstrate for the first time that bevacizumab, which is approved for advanced colorectal and non-small-cell lung cancers, is also effective against kidney cancer.
"The benefits of bevacizumab and interferon were greater than we expected," said lead investigator Dr. Bernard Escudier of the Gustave Roussy Institute in France. "We now need studies to compare the different therapies." Bevacizumab will likely be tested as a single agent against the other therapies in the coming years, he said.
The response rate in the trial of 649 patients was 31 percent for the bevacizumab group compared with 13 percent for the placebo group. After an interim analysis showed a clear benefit, all patients were offered the bevacizumab combination. Preliminary data suggest that bevacizumab may prolong survival, but additional studies are needed.
Combinations of targeted therapies may be needed to achieve the maximum benefit for patients. Toward this end, an early-stage clinical trial presented at ASCO showed that some patients tolerated a combination of sunitinib and bevacizumab. As dosage information becomes available, the combination may be appropriate for phase II trials in metastatic renal cell carcinoma as well as other cancers, the researchers said.
Cetuximab Extends Survival in Recurrent Head and Neck Cancer
Cetuximab 23 (Erbitux), a monoclonal antibody targeting the epidermal growth factor receptor, has proven effective in treating several kinds of head and neck cancer. It was approved last year by the FDA for initial treatment of advanced squamous cell carcinoma of the head and neck (SCCHN). Researchers at last week's ASCO meeting reported the results of the European EXTREME trial 24, and added to accumulating evidence that cetuximab also has a role in treating the disease when it recurs or metastasizes.
Lead author Dr. Jan B. Vermorken from the University of Antwerp in Belgium called the survival benefit - a 21-percent risk reduction with cetuximab patients surviving 10.1 months, 2.7 months longer than those receiving standard care - "among the longest ever seen in a large clinical trial among these patients." For more than two decades, progress in this setting had plateaued. Patients with recurrent or metastatic SCCHN usually receive platinum-based, palliative chemotherapy, sometimes with an intent to cure, but most do not survive beyond 6 to 7 months.
All 442 patients received standard care: up to six cycles of chemotherapy with 5-fluorouracil 25 plus either carboplatin or cisplatin 15. The experimental group also received cetuximab, until the disease progressed or unacceptable toxicity levels were reached. The most common side effect associated with cetuximab was a controllable rash.
Shark Cartilage Ineffective Against Lung Cancer
A clinical trial to rigorously evaluate shark cartilage as a cancer therapy found no benefits for patients. Lung cancer patients who took AE-941 (Neovastat) along with chemotherapy and radiation lived no longer than patients who did not (about 15 months), researchers reported at the ASCO annual meeting. The final-stage clinical trial 26 was cosponsored by NCI and included 384 patients.
Physicians know that many cancer patients consume natural products that have not been scientifically tested and that may interact with conventional treatments. The cartilage study was designed to see whether a natural product developed as a pharmaceutical 27 and put through standard clinical testing might benefit cancer patients. Unlike the products sold in stores and over the Internet, AE-941 was available only through the trial.
Early testing suggested that the drug may block the growth of blood vessels that feed tumors, but in the end the results were negative. "AE-941 is not an effective therapeutic agent for lung cancer," said lead investigator Dr. Charles Lu of the University of Texas M.D. Anderson Cancer Center.
|
 |
 |

Slowly but Surely, Turning Science into Medicine
The theme of this year's ASCO annual meeting was "Translating Research into Practice." The phrase is open to interpretation, but many would agree that translation is an art, not a science, and that it usually takes a long time.
Consider the example of Met, a gene discovered at NCI in the early 1980s. Two decades later, the gene has emerged as an important player in a variety of cancers, including lung, gastric, and melanoma. Many companies are developing drugs to block signals from the Met protein, which can drive cells to grow and spread.
Whether any of these drugs will be safe and effective is an open question. But studying Met has led to new insights into how cells communicate and what can go wrong in cancer, making it a model for developing targeted therapies.
At the meeting, many researchers got their first look at clinical results for Met inhibitors. The news was positive. Two drugs - one developed by ArQule (called ARQ 197) and another by Exelixis (called XL880) - may have benefited some patients and were well tolerated.
"These are two interesting novel agents and both have encouraging antitumor activity," said Dr. Francisco Esteva of the University of Texas M. D. Anderson Cancer Center, who discussed the presentations at the meeting.
Each drug was tested against multiple cancers, and the drugs themselves were different: ARQ 197 inhibits Met alone, while XL880 inhibits Met and another signaling protein, VEGFR2.
Met plays an important role in early development. But the gene is less active later in life, and this helps make it an attractive therapeutic target.
In one XL880 trial, several patients with papillary renal cell cancer appeared to respond. This disease is difficult to treat and can occur because Met is mutated or amplified (extra copies of the gene are present in a cell).
The results are "exciting," said Dr. George Vande Woude, whose laboratory at NCI discovered Met and led the early work on the gene. "This is some of the first evidence that the strategy of inhibiting Met is working in the clinic."
Dr. Vande Woude now directs the Van Andel Research Institute in Grand Rapids, MI, which maintains an online database 28 of studies on Met (technically called c-Met) and cancer. Collectively, the studies tell the story of Met research and provide an indication of how much time and money may be required to take a discovery from the laboratory to the clinic.
"Translation takes time, and there is no shortcut," commented Dr. Vande Woude. He noted that work on trastuzumab 29 (Herceptin), one of the successful new targeted drugs, began shortly before Met was discovered.
For many years, drug developers thought that inhibiting Met might affect the liver or other organs, but research eventually allayed these concerns. "Various groups then moved forward aggressively with Met inhibitors," said Dr. Bart Lutterbach of Merck, who studies Met in lung and gastric cancers.
Mutations and amplifications of Met may be relatively rare in many cancers, noted Dr. Lutterbach. But for patients whose tumors depend on Met signaling, blocking these signals will be necessary to treat the disease.
The Met protein, which sits on the surface of cells, is a tyrosine kinase receptor. Other members of this family include the targets of gefitinib 11 (Iressa) and imatinib 30 (Gleevec).
Over the last 20 years Met has been a tool for understanding how kinase receptors can be deregulated, said Dr. Morag Park of McGill University, who discovered the gene while working with Dr. Vande Woude at NCI.
"Met has led us to a much deeper understanding of signaling pathways involved in cancer," she added. "The important question to ask about Met now is whether it works in a synergistic way with other signals involved in cancer."
Dr. Park predicted that considerable "crosstalk" among signaling pathways will be found in cancer cells when the studies are possible.
A striking example 31 of this phenomenon may have been discovered recently in lung cancer. When the signaling protein EGFR was blocked by a drug, lung cancer cells simply amplified Met to take its place and rendered the drug useless, researchers reported in the April 26 Science.
In light of this cooperation, a comprehensive understanding of how signals are transmitted in cells may be required to treat some cancers. And patients may one day take multiple drugs, as HIV patients do, in an effort to prevent resistance.
"By using combinations of targeted therapies, it should be possible to reduce the likelihood that tumors can escape the control of individual drugs," said Dr. Vande Woude.
At the same time, Met inhibitors may work synergistically with other inhibitors. Dr. Ravi Salgia of the University of Chicago and his colleagues have tested a Met inhibitor that cooperated with the drug rapamycin in some tumors.
Dr. Salgia is now focusing on how to identify lung cancer patients who may benefit from anti-Met therapy. These patients would have increased Met activity as a result of mutations, amplifications, or perhaps drug resistance.
"There are a lot of unanswered questions we need to figure out," said Dr. Salgia. "But working to understand pathways such as Met may open windows of opportunity for other therapies."
Phase II trials are underway for XL880, and positive results 32 have been reported. Many other experimental agents are waiting in the wings.
"We need to move forward with these agents because they are the next generation of cancer therapies," said Dr. Patricia LoRusso of the Barbara Ann Karmanos Cancer Institute in Detroit, who presented results on XL880 at ASCO.
"We are finally starting to turn science into medicine, and it's exciting," she added.
- Edward R. Winstead
|
 |
 |

Dietary and Herbal Therapy for Brain Cancer
Name of the Trial
Phase II Randomized Study of Adjuvant Boswellia serrata Combined with a Low-Fat, Arachidonic Acid-Free Vegan Diet Versus a Standard Diet Alone in Patients with Newly Diagnosed or Recurrent High-Grade Gliomas (CASE-CCF-7348). See the protocol summary at http://cancer.gov/clinicaltrials/CASE-CCF-7348.
 Principal Investigator Principal Investigator
Dr. Glen Stevens, Cleveland Clinic Foundation
Why This Trial Is Important
High-grade gliomas are among the most common and aggressive forms of adult brain cancer. Swelling of the brain (brain edema) is an often debilitating symptom of glioma and may continue to affect patients even if the tumor is surgically removed.
Resin from the Boswellia serrata tree (frankincense) has been shown in animal and human studies to reduce inflammation, which is a primary cause of brain edema. Additionally, laboratory studies suggest that B. serrata resin may also cause human brain cancer cells to undergo programmed cell death (apoptosis).
In this trial, patients will be randomly assigned to take an herbal preparation of B. serrata orally four times a day and eat a low-fat vegan diet for 6 months or to eat a normal low-fat diet for 6 months. Vegan diets lack arachidonic acid, a chemical found in meat that is converted in the brain to signaling molecules called eicosanoids that may promote inflammation and tumor growth. Doctors want to see if B. serrata and a vegan diet can help reduce brain edema, tumor growth, and levels of 5-lipoxygenase, an enzyme that helps convert arachidonic acid to eicosanoids, in these patients.
"Some small studies have suggested that frankincense extract may help limit brain edema and even have an anti-tumor effect," said Dr. Stevens. "We hope that dietary changes in conjunction with use of this herbal preparation will help improve patient outcomes and act in a complementary fashion with standard treatments for high-grade gliomas."
Who Can Join This Trial
Researchers will enroll 70 patients aged 18 and over with newly diagnosed or recurrent high-grade glioma who have undergone surgery to remove their cancer. See the list of eligibility criteria at http://cancer.gov/clinicaltrials/CASE-CCF-7348.
Study Site and Contact Information
This trial is being conducted at the Cleveland Clinic Taussig Cancer Center. For more information, call the Taussig Cancer Center toll free at 1-800-862-7798.
An archive of "Featured Clinical Trial" columns is available at http://cancer.gov/clinicaltrials/ft-all-featured-trials. |
 |
 |
CCR Intern Wins Intel Foundation Award
 Dayan "Jack" Li, a high school intern in CCR's 33 Laboratory of Pathology 34, was awarded an Intel Foundation Young Scientist Award and a $50,000 college scholarship at the Intel International Science and Engineering Fair (ISEF) on May 18. Dayan "Jack" Li, a high school intern in CCR's 33 Laboratory of Pathology 34, was awarded an Intel Foundation Young Scientist Award and a $50,000 college scholarship at the Intel International Science and Engineering Fair (ISEF) on May 18.
Mr. Li, under the guidance of Dr. David D. Roberts, worked with cells from the inside of human umbilical veins to examine the effects of thrombospondin-1 (TSP1) and nitric oxide (NO) on angiogenesis. His objective was to determine how to inhibit this process, which is essential to tumor growth and metastasis. He found that when TSP1 was combined with NO, the reaction switched from inhibitory to stimulatory.
The Intel event is the world's largest precollege celebration of science. Held annually in May, the Intel ISEF brings together nearly 1,500 students from more than 40 nations.
Free Telephone Workshop for Cancer Survivors
NCI, in collaboration with CancerCare, the Lance Armstrong Foundation, the Intercultural Cancer Council, Living Beyond Breast Cancer, and the National Coalition for Cancer Survivorship, will present the workshop, "Finding Hope and Meaning after Treatment," on June 19 from 1:30-2:30 p.m., EDT. This is the final installment of the three-part telephone workshop series "Cancer Survivorship: Living With, Through, & Beyond Cancer."
This free series offers cancer survivors, their families, friends, and health care professionals practical information to help them cope with concerns and issues that arise after treatment ends. Parts I and II of the series are available as podcasts on the CancerCare Web site 35.
If Memory Serves...
With the encouragement of NCI representatives, in 1939, seven U.S. states began to include cancer control in their health departments' missions; three states established cancer commissions. NCI also began to distribute information on cancer for public education, and produced a movie for this purpose with the help of the American Society for Control of Cancer that was designed for nonscientific viewers. Eventually, the Institute published "What to Know, What to Do about Cancer" - a prelude to NCI's "What You Need to Know About..." series - and distributed 48,000 copies for free. Read more 36)
For more information about the birth of NCI, go to http://www.
cancer.gov/aboutnci/ncia.
NCI Helps Create Radiation Emergencies Management Web Site
After months of development by an interagency team that included two NCI experts, a unique Web site was unveiled on March 8 by the Department of Health and Human Services (HHS). The Radiation Event Medical Management 37 (REMM) site was established to provide just-in-time information for diagnosis and treatment guidance to health care providers - primarily physicians - who do not have formal radiation medicine expertise. In the event of mass casualties during a radiological and/or nuclear event, REMM is a one-stop, algorithm-based response, backed by an exhaustive catalog of information and links to relevant Web sites. The Web-based system can be downloaded in advance of such an emergency where Internet access might be compromised. The information has been vetted by some 45 subject experts in the fields involved.
The site emerged from work at the Office of Preparedness and Emergency Operations in the Office of the Assistant Secretary for Preparedness and Response at HHS. Dr. Norman Coleman of NCI's Division of Cancer Treatment and Diagnosis 38 was the team leader; Dr. Judith L. Bader, Captain, USPHS, of NCI's Office of Communications and Education is the managing editor of REMM.
NCI Releases New Tobacco Control Monograph
NCI has released Greater than the Sum: Systems Thinking in Tobacco Control, the latest in the tobacco control monograph series. The monograph describes key lessons from the first 2 years of the Initiative on the Study and Implementation of Systems (ISIS), an NCI-funded project that explored systems thinking approaches and methodologies to public health.
The monograph is available online and can be ordered at http://dccps.cancer.gov/tcrb/monographs/.
|
|
 |
 |

Salk Institute for Biological Studies Cancer Center
Director: Dr. Walter Eckhart • 10010 North Torrey Pines Road, La Jolla, CA 92037 • Phone: 858-453-4100 ext. 1386 • Web site: http://www.salk.edu
Background
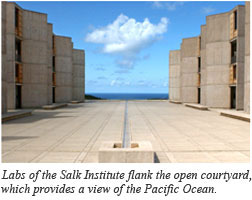 In 1962, Dr. Jonas Salk, developer of the polio vaccine, established the Salk Institute for Biological Studies as a collaborative research organization with seed money from the March of Dimes and a land grant from the City of San Diego. He and architect Louis Kahn designed a research campus on the Torrey Pines Mesa that overlooks the Pacific Ocean. The Cancer Center at the Salk Institute took root in 1970 with core grant funding from NCI. In 1962, Dr. Jonas Salk, developer of the polio vaccine, established the Salk Institute for Biological Studies as a collaborative research organization with seed money from the March of Dimes and a land grant from the City of San Diego. He and architect Louis Kahn designed a research campus on the Torrey Pines Mesa that overlooks the Pacific Ocean. The Cancer Center at the Salk Institute took root in 1970 with core grant funding from NCI.
Today, Cancer Center investigations comprise approximately half of the research conducted by the Salk Institute and occupy more than 60,000 square feet of laboratory space within the original campus. This research supports 22 faculty members, 150 postdoctoral researchers, 45 graduate students, and 80 research assistants.
Research Activities
Over the past three decades, researchers in the Cancer Center have made important contributions to the understanding of cancer, including discovery of tyrosine phosphorylation and elaboration of its role in cell growth control; identification of nuclear hormone receptors and elucidation of their role in physiology and development; characterization of transcription factors that control gene expression and cell growth, differentiation, and patterning; and development of viral vectors for gene therapy.
The Salk Institute Cancer Center currently focuses on three research areas: molecular biology and genetics, growth control, and cell and developmental biology. Within these areas, scientists are studying signal transduction pathways using phosphorylation and ubiquitination that regulate cell size and cell proliferation in normal cells, cancer cells, and animal models; the functions of tumor suppressor proteins, including p53, LKB1, and APC; the response of cells to DNA damage and how this is perturbed in cancer cells; the involvement of telomere dysfunction in cancer; the connections between aging and cancer; and the role of stem cells in cancer.
Other Notable Programs
As a basic research facility, the Salk Institute does not conduct studies with human patients. However, the Salk Institute collaborates with outside clinical facilities, including the University of California, San Diego, and hospitals in the greater San Diego area.
Research underway in the Cancer Center is supported by competitively awarded grants of approximately $16 million. In addition, Cancer Center members have been working with The Genomics Institute of the Novartis Research Foundation to carry out genome-wide screens, and the Salk Institute is part of the San Diego Consortium for Regenerative Medicine, which has plans to establish a facility that will serve the La Jolla mesa area, funded in part by the California Institute for Regenerative Medicine (CIRM). Most recently, the Salk Institute received a $2.3 million facilities grant from CIRM to fund the development of shared laboratory space where investigators will conduct scientific research on human embryonic stem cells.
NCI recently designated two new Cancer Centers: Stanford Comprehensive Cancer Center and the Dan L. Duncan Cancer Center at Baylor College of Medicine. |
 |
 |
Following are newly released NCI research funding opportunities:
Community Clinical Oncology Program
Announcement Number: RFA-CA-07-048
Letter of Intent Receipt Date: June 18, 2007
Application Receipt Date: July 18, 2007
This is a renewal of RFA-CA-07-025 and will use the U10 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3730. Inquiries: Dr. Lori Minasian - minasilo@mail.nih.gov
Minority-Based Community Clinical Oncology Program
Announcement Number: RFA-CA-07-049
Letter of Intent Receipt Date: June 18, 2007
Application Receipt Date: July 18, 2007
This is a renewal of RFA-CA-07-025 and will use the U10 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3731. Inquiries: Dr. Worta McCaskill-Stevens - mccaskiw@mail.nih.gov
A Data Resource for Analyzing Blood and Marrow Transplants
Announcement Number: RFA-CA-07-506
Letter of Intent Receipt Date: June 25, 2007
Application Receipt Date: July 25, 2007
This funding opportunity will use the U24 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3732. Inquiries: Dr. Roy S. Wu - wur@ctep.nci.nih.gov
NCMHD Community-Based Participatory Research Initiative in Reducing and Eliminating Health Disparities: Intervention Research Phase
Announcement Number: RFA-MD-07-003
Letter of Intent Receipt Date: July 31, 2007
Application Receipt Date: Aug. 31, 2007
This funding opportunity will use the U24 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3733. Inquiries: Dr. Kenneth Chu - KC10D@NIH.GOV
Omics and Variable Responses to CAM: Secondary Analysis of CAM Clinical Trials
Announcement Numbers: PAR-07-377 and PAR-07-378
Application Receipt Dates: Aug. 14, 2007; Aug. 14, 2008; Aug. 14, 2009
This funding opportunity will use the R01 (PAR-07-377) and R21 (PAR-07-378) award mechanisms. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3735. Inquiries: Dr. Nancy Emenaker - emenaken@mail.nih.gov
Behavioral and Social Science Research on Understanding and Reducing Health Disparities
Announcement Numbers: PAR-07-379 and PAR-07-380
Letter of Intent Receipt Dates: Aug. 20, 2007; Aug. 20, 2008; Aug. 20, 2009
Application Receipt Dates: Sept. 19, 2007; Sept. 19, 2008; Sept. 18, 2009
This funding opportunity will use the R01 (PAR-07-379) and R21 (PAR-07-380) award mechanisms. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3736. Inquiries: Dr. Shobha Srinivasan - ss688k@nih.gov
Biology of Breast Pre-Malignancies
Announcement Number: RFA-CA-07-047
Letter of Intent Receipt Date: Oct. 14, 2007
Application Receipt Date: Nov. 14, 2007
This funding opportunity will use the R01 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3729. Inquiries: Anne S. Tatem - tatema@mail.nih.gov |
 |
|
Table of Links
| 1 | http://www.cancer.gov/cancertopics/druginfo/sorafenibtosylate |
| 2 | http://www.cancer.gov/clinicaltrials/100554 |
| 3 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_061207/page2 |
| 4 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_061207/page3 |
| 5 | http://www.cancer.gov/cancertopics/druginfo/bevacizumab |
| 6 | http://www.cancer.gov/cancertopics/druginfo/erlotinibhydrochloride |
| 7 | http://www.cancer.gov/cancertopics/druginfo/sunitinibmalate |
| 8 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_061207/page5 |
| 9 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_051507/page5 |
| 10 | http://www.asco.org/portal/site/ASCO/menuitem.34d60f5624ba07fd506fe310ee37a01d/
?vgnextoid=76f8201eb61a7010VgnVCM100000ed730ad1RCRD&vmview=abst_detail_view
&confID=47&abstractID=30746 |
| 11 | http://www.cancer.gov/cancertopics/druginfo/gefitinib |
| 12 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_011706/page2 |
| 13 | http://www.asco.org/portal/site/ASCO/menuitem.34d60f5624ba07fd506fe310ee37a01d/
?vgnextoid=76f8201eb61a7010VgnVCM100000ed730ad1RCRD&vmview=abst_detail_view
&confID=47&abstractID=35251 |
| 14 | http://www.clinicaltrials.gov/ct/show/NCT00272324?order=1 |
| 15 | http://www.cancer.gov/cancertopics/druginfo/cisplatin |
| 16 | http://www.cancer.gov/cancertopics/druginfo/gemcitabinehydrochloride |
| 17 | http://www.cancer.gov/cancertopics/druginfo/paclitaxel |
| 18 | http://www.cancer.gov/cancertopics/druginfo/docetaxel |
| 19 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_010307/page4#b |
| 20 | http://www.asco.org/portal/site/ASCO/menuitem.34d60f5624ba07fd506fe310ee37a01d/
?vgnextoid=76f8201eb61a7010VgnVCM100000ed730ad1RCRD&vmview=abst_detail_view
&confID=47&abstractID=30666 |
| 21 | http://www.cancer.gov/clinicaltrials/CALGB-90206 |
| 22 | http://www.cancer.gov/cancertopics/druginfo/fda-temsirolimus |
| 23 | http://www.cancer.gov/cancertopics/druginfo/cetuximab |
| 24 | http://www.cancer.gov/clinicaltrials/NCT00122460 |
| 25 | http://www.cancer.gov/cancertopics/druginfo/fluorouracil |
| 26 | http://www.cancer.gov/clinicaltrials/MDA-ID-99303 |
| 27 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_072605/page4 |
| 28 | http://www.vai.org/met |
| 29 | http://www.cancer.gov/cancertopics/druginfo/trastuzumab |
| 30 | http://www.cancer.gov/cancertopics/druginfo/imatinibmesylate |
| 31 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_051507/page6 |
| 32 | http://www.asco.org/portal/site/ASCO/menuitem.34d60f5624ba07fd506fe310ee37a01d/
?vgnextoid=76f8201eb61a7010VgnVCM100000ed730ad1RCRD&vmview=abst_detail_view
&confID=47&abstractID=35500 |
| 33 | http://ccr.nci.nih.gov |
| 34 | http://ccr.cancer.gov/labs/lab.asp?labid=106 |
| 35 | http://www.cancercare.org/get_help/tew_calendar.php |
| 36 | http://www.cancer.gov/aboutnci/if-memory-serves |
| 37 | http://remm.nlm.gov |
| 38 | http://dctd.cancer.gov |
|
 |