 |
 |

|
Testimony
Wednesday, March 1, 2006 Chairman Deal, Rep. Brown, distinguished members of the Subcommittee, thank you for the opportunity to update you on the new Medicare prescription drug coverage, and especially the steps we are taking to address transition issues. The vast majority of beneficiaries are using their coverage effectively, plans are filling over a million prescriptions a day, and each week hundreds of thousands more beneficiaries are enrolling in the new program. Prescription drugs are a critical component of 21st Century medicine, but until recently the Medicare program did not include an outpatient prescription drug benefit. Now Medicare�s new prescription drug benefit provides seniors and people with disabilities with comprehensive prescription drug coverage, the most significant improvement to Medicare coverage in 40 years. Millions of seniors and people with disabilities are already using this benefit to save money, stay healthy, and gain peace of mind, rather than simply paying the bills when they get sick. Because of strong competition in the prescription drug marketplace, there has been slower drug cost growth in recent years, due in part to improving generic drug availability. Consequently, the new Medicare prescription drug coverage is costing much less for beneficiaries, taxpayers, and the States than anticipated. For example, beneficiary premiums are now expected to average $25 a month � down from the $37 projected in last July�s budget estimates � and the overall cost to taxpayers for 2006 has dropped about 20 percent since the July 2005 estimate, according to the CMS Office of the Actuary. The savings result from lower than expected costs per beneficiary; projected enrollment in the drug benefit has not changed significantly. For the 10-year period from 2006-2015, the net total cost to Medicare of the drug benefit is now estimated to be about $130 billion less - $797 billion compared to an estimated $926 billion last year. In addition, the state phase-down contributions are now projected to be $37 billion (about 27 percent) less over the 10-year period. We already are hearing reports from our partners about the cost savings people with Medicare are experiencing. For example, Barbara from Lynchburg, Virginia, with the assistance of a community based organization, selected and enrolled in a plan that will save her $2,400 a year on her drug costs. On average, seniors who previously did not have drug coverage are saving $1,100 on their annual drug costs by selecting a plan in the new Medicare prescription drug benefit, compared to paying directly for their drug costs. The savings for beneficiaries who now qualify for the low-income subsidy (and who did not previously receive Medicaid drug coverage) is substantially greater, amounting to over 95 percent of drug costs on average. While considerable progress has been made, change of this magnitude in such a short time span is bound to encounter some difficulties. CMS is very concerned about anyone who has experienced problems in obtaining their medicines. We make no excuses for the problems. They are important, they are ours to solve, and we are finding and fixing them. Specifically, a significant portion of the problems for beneficiaries centered on certain beneficiaries who enrolled or switched plans late in a month, particularly dual eligible beneficiaries, those individuals who qualify for both Medicare and Medicaid. We are taking action to address these issues so that all beneficiaries enrolled in a Medicare prescription drug plan can obtain their medications without incident. CMS also is working to correct data transmission problems between Medicare, health plans, pharmacists, and the States. Customer service also is a priority, and we are working to eliminate any delays or other difficulties for those needing assistance. In order to assist pharmacists, who have been outstanding in their commitment to service, CMS is working to ensure they have the resources and support they need. CMS also is coordinating with the States that used their state reimbursement systems to pay for prescriptions that should be paid by the new Medicare prescription drug plans. CMS believes they should be reimbursed for any legitimate expenses beyond the payments they will receive from the plans and is doing so through a new demonstration program. We also are monitoring plan activities and will use our enforcement measures, if necessary, to ensure they are adhering to the requirements of participating in the Medicare prescription drug program. These efforts build on the preparations that were made long before the January 1, 2006 launch of the Medicare prescription drug benefit. CMS and Partners Conduct Extensive Outreach and Education for Beneficiaries CMS worked with the plans, pharmacists, States, and hundreds of other partners leading up to the start of the drug benefit to educate beneficiaries and their caregivers about the Medicare prescription drug benefit and help people understand how to make decisions about the prescription drug plans based on cost, coverage, convenience, and peace of mind. These efforts are continuing with particular emphasis on rural areas and beneficiaries who may qualify for the low-income subsidy. In addition to print, radio and television advertisements, CMS has a multi-pronged approach to raise awareness and assist beneficiaries and their caregivers in making decisions about prescription drug plans. President Bush, Secretary Leavitt, and I, along with CMS� regional office staff, have traveled over 200,000 miles across the country in a mobile office bus to form grassroots partnerships that help people with Medicare make an informed decision about prescription drug coverage. About 73 percent of these mobile office stops have taken place in rural communities throughout the country. Many Members of Congress have served as honorary chairs for these events and we appreciate their involvement in forging over 240 grassroots community and statewide networks, each led by a community partner. The mobile office reached rural areas across the country to complement our dedicated funding for research and outreach to rural areas. To date, 235 Members or their staff have participated in events and we welcome your involvement in future activities to reach beneficiaries, especially those who can benefit from the low income subsidy. In addition to the mobile office events, the CMS regional offices along with state health insurance assistance programs, senior advocacy organizations, and agencies on aging have held thousands of information and enrollment events. Since January CMS and its partners have hosted over 2,000 events. These organizations also are providing personalized counseling on request to help beneficiaries enroll in plans that best meet their needs. CMS worked with the Social Security Administration and various organizations to provide training and conduct outreach to beneficiaries who may qualify for low-income assistance. These organizations include for example, the Access to Benefits Coalition, Case Management Society of America, the National Association of Community Health Centers the Visiting Nurses Association of America, AARP, and CARxE (a private group focusing on outreach to low income beneficiaries through faith-based efforts). In addition, CMS provided special training for social service coordinators to help them counsel low-income seniors. CMS also worked with social workers and many sub-specialty organizations such as the Oncology Social Workers, who have a desire to help their client base and their community make decisions about the Medicare prescription drug benefit. CMS also has a contract with the National Association of Area Agencies on Aging (n4a) to target beneficiaries and their caregivers that are hard to reach including minority, low-income, limited English speaking, homebound, and rural populations. Strategies included contracting with Aging Network community-based organizations and nine National Aging Organizations with local affiliates to conduct outreach to low-income populations. The nine organizations include the National Association of Nutrition and Aging Services Providers, Meals on Wheels Association of America, National Hispanic Council on Aging, Asociacion Nacional Pro Personas Mayoras, The National Alliance for Hispanic Health, National Center and Caucus for Black Aged, Inc., National Asian Pacific Center on Aging, National Adult Day Services Association, and National Council for Independent Living. In addition to events around the country, we are providing a number of ways for people to get information. The Medicare & You 2006 handbook included information about the new prescription drug coverage. Also, the 1-800-Medicare helpline (including TTY assistance) and www.medicare.gov are available 24-hours a day with assistance in English and Spanish, and help available in many other languages as well. Strong Enrollment Continues to Grow As shown in Figure 1, as of February 13 about 4.9 million people have enrolled individually in a stand-alone prescription drug plan, and more than 400,000 beneficiaries have also newly enrolled in Medicare Advantage (MA) plans that are generally providing more comprehensive and lower-cost drug coverage. About 6.2 million dual eligible individuals also are enrolled in Medicare prescription drug plans, including 560,000 in Medicare Advantage plans, many of whom have more comprehensive coverage than before (for example, about one in four states had limits on the number of prescriptions for Medicaid beneficiaries, and Medicare coverage has no such limits). Another 4.7 million people are enrolled in a Medicare Advantage plan, and this coverage is now much more comprehensive and less costly (previously, while most MA plans provided drug coverage, the coverage generally included caps and other limits). About 6.4 million retirees are enrolled in employer- or union-sponsored retiree plans receiving the Medicare Retiree Drug Subsidy and another 1 million retirees are in employer coverage that incorporates or supplements Medicare�s coverage, so that high-quality retiree coverage has more secure financial support. Separate from the new Medicare drug benefit, another estimated 500,000 retirees from employers not utilizing the Medicare retiree subsidy are continuing in coverage that is as good as Medicare�s. An additional 3.1 million retirees are receiving prescription drug coverage either through TRICARE or the Federal Employee Health Benefits Program (FEHBP). 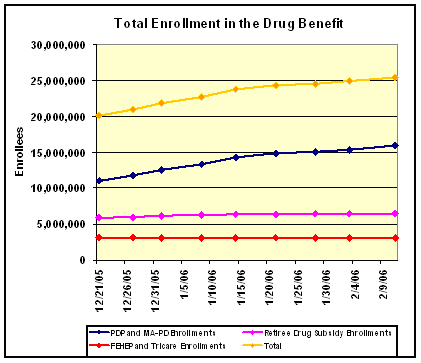
Figure 1: Enrollment in Medicare Prescription Drug Benefit, Medicare Advantage-PDPs, the Retiree Drug Subsidy, FEHBP, and TRICARE Although more than 25 million Medicare beneficiaries now have prescription drug coverage and CMS is encouraged by the strong enrollment numbers, outreach efforts will continue to promote enrollment for those who will benefit from this program and who have not yet enrolled. The open enrollment period for the new drug benefit continues until May 15, 2006 and we are encouraging and helping people with Medicare to review their options and select a plan that works best for them. Competition Helps Lower Drug Prices CMS analyses demonstrate that Medicare beneficiaries with common chronic conditions can save a substantial amount on their drug bills by enrolling in a Medicare prescription drug plan (PDP) compared to what they would pay with no drug coverage. For instance, people with Medicare who select the lowest-cost plan in their area can save up to 71 percent off the prices they would pay without prescription drug coverage. The analysis also demonstrates that a range of plans available to beneficiaries can also provide large savings. This is true for a very broad range of plans if beneficiaries are willing to use generic versions of their existing drugs, when available, which are required to have the same active ingredients and work in the same way as the brand-name drug. These results indicate that beneficiaries can see substantial savings on their drug bills by focusing on a few plans with the features they prefer � such as a low premium, or fixed copayments, or coverage in the gap. Even larger savings are possible � as much as 83 percent � by switching to drugs in the same class that work in very similar ways to a beneficiary�s current brand-name drug. For example, there are many drugs available that work in very similar ways to treat common conditions like stomach acid problems, Allergic rhinitis, high blood pressure, and high cholesterol levels. According to Consumers Union, considering these drugs can save beneficiaries billions more in drug costs each year. Beneficiaries can get personalized information on these additional savings from medicare.gov, 1-800-MEDICARE, and many of Medicare�s partners. A number of external reports strongly support these findings. For example, the Pharmaceutical Care Management Association (PCMA) released a study in February 2006 indicating that Medicare drug plans offer significant price discounts compared to what beneficiaries would pay without coverage. The study found an average savings for beneficiaries of 35 percent at participating retail pharmacies and 46 percent through mail order pharmacies. Further, for 25 commonly used medications, the PCMA study found savings from 18 percent on brand name drugs at retail pharmacies to 26 percent at mail order pharmacies. In addition, a January 2006 report prepared by the Lewin Group demonstrates that beneficiaries with chronic conditions, particularly those with multiple conditions, will see significant savings on their prescription drug bills by enrolling in a Medicare prescription drug plan. For example, while beneficiaries with one chronic condition will save on average $396 on their medications with Medicare drug coverage, accounting for 26 percent of their current drug spending, those with four or more conditions will save an average of $1,774, or 41 percent, on their medications. These studies have made �apples to apples� comparisons of drug prices available at retail pharmacies instead, for example, of common, but misleading, comparisons between retail pharmacy and mail-order prices. For this reason, in their recent forecast of prescription drug spending trends, the independent Medicare actuaries have concluded that overall drug spending will be slightly lower as a result of the Medicare drug benefit, even though Medicare beneficiaries will be able to fill millions more prescriptions than would have been possible without the drug coverage. Market Forces Drive Plan Simplification CMS also is working to make it as easy as possible for beneficiaries to review the different options available to them in selecting a plan. As individuals have different needs and preferences when it comes to their health-care coverage, presenting plan features in a way that facilitates comparison on the basis of plan attributes and performance indicators will make it easier for beneficiaries to choose the plan with the features that are most important to them. In our research of Medicare beneficiaries, overall drug cost is generally the most important single factor to most beneficiaries. Other important plan attributes include the premium, the deductible, whether the plan provides a set copayment amount or a percentage coinsurance, and more comprehensive coverage in the �coverage gap.� Breadth of formulary (some beneficiaries prefer �open� formularies) and access to a particular pharmacy are also important to many beneficiaries. The substantial savings available to beneficiaries from many plans mean that beneficiaries can focus just on a small number of specific plans that have the features they most prefer. Medicare and its partners are already making available personalized information on these plan features, and we are working with many outside organizations to enhance the resources available to beneficiaries to identify the specific plan or plans that are a good fit based on their own preferences. Addressing Coverage Problems for Dual Eligible and Late Enrollees 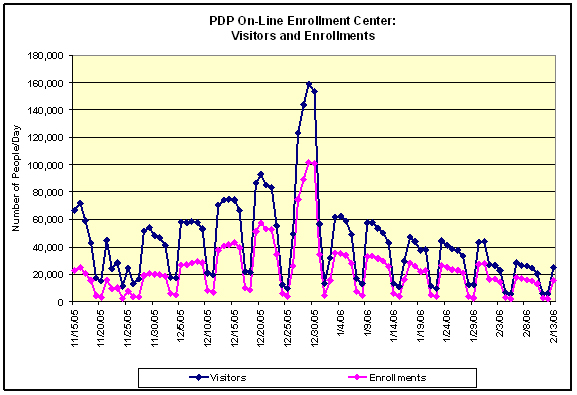
Figure 2: Prescription Drug Plan On-Line Visitors and Enrollments Some people with Medicare prescription drug coverage who enrolled or switched plans late in the month, particularly dual eligible beneficiaries, experienced problems when attempting to fill prescriptions early the next month. The information systems did not have sufficient time to reflect this change and accommodate the fact that hundreds of thousands of beneficiaries switched plans in the last half of December, as reflected in our early January problems. CMS is working to minimize problems associated with switching plans and late-month enrollments in the future as we do not want anyone with Medicare who is enrolled in a plan to leave the pharmacy without the prescriptions they need. Because it takes time to process enrollments, there are real advantages to joining a Medicare drug plan at the beginning of the month. Almost all who join or change plans before the 15th of each month will get their prescriptions filled quickly and conveniently beginning with the next month. Early enrollments allow Medicare and the plans time to update systems and plans time to mail important documents (e.g., confirmation letter, membership card, welcome package) before the effective date of coverage. Early enrollees can get the most out of their coverage from the first day it is effective. Enrollees who join later in the month may have to spend extra time at the pharmacy to get their prescriptions filled, especially if they try to use their coverage shortly after enrolling. To make people aware of the advantages of enrolling early in the month, CMS updated its online enrollment center messages and modified scripts used in our call centers, and we are communicating this information to pharmacists, States, and advocacy organizations. These educational activities may already be having an effect: In the last week of January, only about 24,000 people switched plans, down from the hundreds of thousands of individuals who were auto-enrolled and elected a different plan in the last half of December. This reduced the problems of incomplete information at the pharmacy counter significantly at the start of February. To improve the information available to Part D plans about their dual eligible and low-income members, CMS provided the Medicare prescription drug plans with several files during January of all the people with Medicare who are either dual eligible or qualify for the low-income subsidy. We have continued to provide such sources of information to confirm plan enrollments in February. The plans use this data to cross-check with their own records to correct any errors or omissions. As plans process these data and improve their beneficiary information databases, the workload of the pharmacists is reduced and the vast majority of dual eligible individuals get their drugs more smoothly. With correct data, pharmacists identify plans in which dual eligible individuals are enrolled and ensure that correct and appropriate copayments are charged to the individual with Medicare. As a result of these data exchanges, we expect fewer problems for people with Medicare at the pharmacy. CMS Automatically Enrolled Full Benefit Dual Eligible Individuals into Plans Also, while other individuals generally have the opportunity to change plans only at the end of the calendar year, dual eligible individuals have the opportunity to change plans at any time. This flexibility allows them further opportunities to select a plan that best meets their needs. CMS also has worked with States to identify and auto-enroll individuals who are about to become full-benefit dual eligible prior to the end of their Medicaid drug coverage to work toward a seamless transition on an on-going basis. This includes those Medicaid individuals who will age into Medicare or who will reach the end of the 24-month Medicare disability waiting period. Point-of-Sale System Facilitates Enrollment Through this point-of-sale system, beneficiaries who present at a pharmacy with evidence of both Medicaid and Medicare eligibility, but without current enrollment in a prescription drug plan, can leave the pharmacy with a filled prescription and the claim for their medication submitted to a single account for payment. A CMS contractor will follow up to validate eligibility and facilitate enrollment of the full-benefit dual eligible individual into a prescription drug plan. CMS has provided information on the WellPoint system to pharmacy associations, plans, and individual pharmacies. This information describes how the process of POS-facilitated enrollment starts at the pharmacy with the pharmacist verifying dual eligibility and billing a special WellPoint account in order to ensure that the individual with Medicare receives the prescription. CMS Worked To Achieve a Smooth Transition in Long Term Care Facilities Cognitively impaired individuals represent a particularly difficult group to educate about their enrollment options. Much of this population, specifically full benefit dual eligible individuals, was auto-enrolled into the new prescription drug benefit. CMS encouraged nursing homes to determine into which plans their residents were auto-enrolled prior to January 1, 2006. As part of this initiative, CMS established dedicated call lines and overnight mail options to allow nursing homes to fax and mail beneficiary information to CMS customer service representatives (CSRs). This strategy enabled CMS to help nursing homes identify the plans for more than 500,000 residents. Pharmacists used the electronic eligibility and enrollment verification (E1) system (described below) to identify the remainder. By notifying plans that their dual eligible enrollees reside in nursing homes, and by assisting LTC facilities in working to correct cases where copay information is not up to date, CMS is ensuring nursing home residents have access to Medicare drug coverage without premiums and copays. CMS Provides Education on the Transition Policy CMS guidance to plans includes a 90 to 180 day transition period for LTC facilities to accommodate the needs of Medicare beneficiaries residing in those facilities. In general, plans are providing 90 day transition periods with many offering the option of extending to 180 days. However, the LTC emergency first-fill policy is unique to this setting and continues throughout the entire year for any off-formulary prescription written. In addition, plans are required to cover drugs as prescribed during the 7 to 14 days allowed for initial exceptions and appeals processes. It is of vital importance that beneficiaries, caregivers, advocates, providers, and pharmacists understand the most expeditious and successful way to transition from drugs on Medicaid formularies to drugs on the plan formularies. Therefore, CMS is providing appropriate education materials to people with Medicare, caregivers, advocates, providers, and pharmacies. These materials will explain the basics of how to successfully transition from one medication to another, the steps that should be taken, and tips for beneficiaries on how to work with their physicians and pharmacists during the transition. CMS also will use earned media, teleconferences and Open Door Forums to provide information about transition policies. CMS is encouraging the new Medicare prescription drug plans to also provide information on how people can transition to an alternate medication. Correcting Initial Data Transmission Issues As an additional safeguard in mid-January, CMS contracted with Electronic Data Systems (EDS) to help CMS work together with the plans, States, and pharmacies to resolve challenging data translation issues. EDS has assisted with our implementation of steps to improve communications and understanding among CMS, plans, and states to support smooth transactions. EDS is providing regular feedback and recommendations to CMS and we expect them to complete a further review with additional recommendations by the end of March. We are working with plans, States, and our other partners to implement their recommendations on an ongoing basis, achieving the goals outlined below by mid-April. Many plans are sending CMS daily files reflecting their enrollment transactions, and reliably use our responses to these daily files as well as our weekly summaries of the results for timely and accurate updates of their systems. Our goal is that plans covering 90 percent of the enrollee population will use these daily and weekly data transfer processes successfully to reduce lags in obtaining updated beneficiary information. To check and further assure the accuracy of the information exchange between plans and CMS, we have sent special updated data files, including full copayment information, on the full dual and low-income subsidy enrollment in plans. Our goal is to achieve, by ten days before a new coverage month begins, at least a 95 percent match for enrollment and LIS copayment information on applicable beneficiaries between Medicare and the plans. As a result, adjustments and additional batch data processing by plans near the end of the month can be limited, while addressing the needs of late-enrolling beneficiaries. We have already seen the match rate for plan enrollment and copayment information increase since mid-January, exceeding 90 to 95 percent before the end of the month. CMS continues to work on matching data files with the States, so that appropriate information for dual eligible individuals is available to CMS, plans, and pharmacists. We obtained a match rate of greater than 99 percent for duals submitted by the States in the fall of 2005, and we expect to maintain a high match rate. Planning Started Early for Information and Technology Requirements These IT systems support the key critical business processes that CMS uses to manage the Medicare Advantage and prescription drug benefit programs. The integrated system provides CMS with the ability, among other things, to enroll people with Medicare into prescription drug plans, make payments to plans, and ensure that beneficiaries receive their drug coverage. In preparation for MMA implementation, CMS refined its systems to accept, process, and reply to plan transactions on a daily basis, a far quicker turnaround than the monthly reporting cycle used under the Medicare Advantage program. CMS is now working with plans to change their operational processes to incorporate this faster processing and reporting cycle. The integrated information technology system also allows CMS to pay the Retiree Drug Subsidy to approved plan sponsors and track True-Out-of-Pocket Expenses (TrOOP � costs borne by the enrollee) for people with Medicare. In addition, the updated systems ensure the correct premium amount is either paid directly to the plan or provided to the Social Security Administration to withhold from a beneficiary�s Social Security check. Through contracts with telecommunications clearinghouses that currently service the majority of retail pharmacies, the pharmacies will be able to perform real-time eligibility determinations and will be able to route claims to primary, and if applicable, secondary plans for proper adjudication to accurately coordinate benefits. The new and modified systems also were designed to ensure only authorized individuals have access to Medicare information. CMS worked closely with industry experts to implement nine system modules. Implementation included application development and integration efforts, system engineering activities, and validation and testing. In order to meet the deadlines, CMS worked creatively and collaboratively to compress what would ordinarily be an 18 to 24-month systems development process. CMS ensured that the necessary computer and network capacity and capabilities were in place as the CMS IT applications came online. These enhancements included:
CMS implemented backup and parallel support systems to minimize any vulnerabilities and also oversaw the implementation of a secure, Internet-based computing environment in the CMS data center. If these systems had not come online on schedule, CMS would not be able to enroll beneficiaries or pay the health plans that are administering the new benefit. CMS set new standards for documenting requirements, program management, managing change, testing systems, and documenting and ensuring that system development life cycle reviews were undertaken. Providing High Level Customer Service CMS Improves 1-800 MEDICARE Call Center to Reduce Wait Times 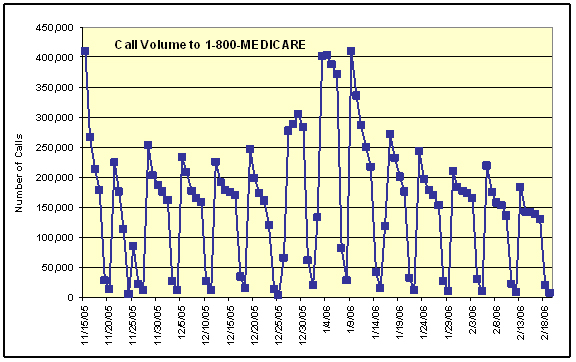
Figure 3: Call Volume 1-800 MEDICARE CMS has increased the number of CSRs from 3,000 in June of 2004 to as many as 7,800 to handle beneficiary calls. We have also acquired additional infrastructure including telephone lines, workstations, and seats at call center sites. We have refined our CSR scripts by reducing redundant information, indexing scripts for quick access, and including probing questions to help the CSRs better identify the caller�s concerns. CMS has implemented a major enhancement through the use of Smart Scripts, which provide the CSRs with an easily followed path of responses to the most frequently asked questions. Smart Scripts are a new type of script that has hyperlinks built into the body of the text that when activated will take the CSR directly to related information about that subject. In addition, we have CSRs participate in the content workgroups for the actual development of scripts and job aides. CMS also has implemented a CSR feedback system and streamlined our approval process for updating the scripts in a timely manner to respond to the changing needs of our customers or to incorporate policy updates. CMS hired and trained additional staff to exclusively use the Prescription Drug Plan Finder tool to handle only prescription drug plan calls. All CSRs receive one week of classroom training followed by two or three additional days of practice calls, simulation, quality monitoring, and follow-up coaching to ensure peak performance. CSR certification with a written examination and test calls is required prior to taking live calls. Calls are being handled on an in-bound basis and steps CMS has taken to strengthen the call centers� capabilities and reduce wait times have made it possible to address beneficiaries� concerns as they arise. CMS customer satisfaction surveys indicate that the bulk of callers who interact with our CSRs, 84 percent, are satisfied with their experience. They are particularly pleased with how courteous and patient the CSRs are (rated at 97 and 95 percent, respectively). These responses came not only from people with Medicare, but also friends or relatives calling on their behalf, who made up 48 percent of callers during December, 2005. In addition to beneficiary satisfaction surveys, CMS also evaluates the 1-800- MEDICARE CSRs through �mystery shopping� to ensure they are providing accurate and complete responses to callers. �Mystery shopping� calls are made to CSRs by an independent specialized quality evaluation contractor who has developed scenarios and scripts to measure the CSRs on various topics to determine if CSRs are being �fully responsive.� A response is considered �fully responsive� if all key points are conveyed to a caller. The independent contractor consistently has found that the information provided is fully responsive most of the time and that an inaccurate response occurs less than 1 percent of the time. CMS� Medicare website, www.medicare.gov, has also been a source of useful information for people with Medicare. Since the first of the year, our frequently asked questions have been accessed more than one million times. CMS also has responded to more than 12,500 e-mails received through the site, with 93 percent of them being resolved satisfactorily in the first response. CMS Works with Plans to Improve Their Customer Service While many plans are now providing timely phone access, some have not responded adequately. Therefore, CMS has increased monitoring of plans� call center activities to help assure a high level of performance. We are surveying all prescription drug plans to assess whether they provide correct information to beneficiaries and pharmacists within a reasonable time. We expect continuing improvements, as we address systems and data transfer issues. We expect plans to generally answer calls within an average response time of five minutes, and while many plans have already made major steps toward this or better performance, we will take further enforcement actions against plans that do not make substantial progress in the weeks ahead. CMS Provides Caseworkers for One-on-One Counseling CMS has established a system to help resolve urgent issues on a case-by-case basis. CMS has hundreds of trained caseworkers who are working as rapidly as possible to resolve urgent issues to help ensure that people with Medicare get their prescriptions filled. CMS urges people with Medicare or their family members who are having difficulties to call 1-800-MEDICARE, and if necessary, their case will be forwarded to our caseworkers. Urgent cases have high priority for rapid resolution. While the number of individual cases is small in comparison to the millions of prescriptions and individuals who are successfully receiving their prescriptions, CMS is committed to ensuring that every individual receives his or her needed medicines, is properly identified, and is charged the appropriate copays in the future. CMS Takes Steps to Identify Areas of Concern CMS Applauds and Supports the Outstanding Efforts of Pharmacists CMS Provides Dedicated Support to Pharmacists 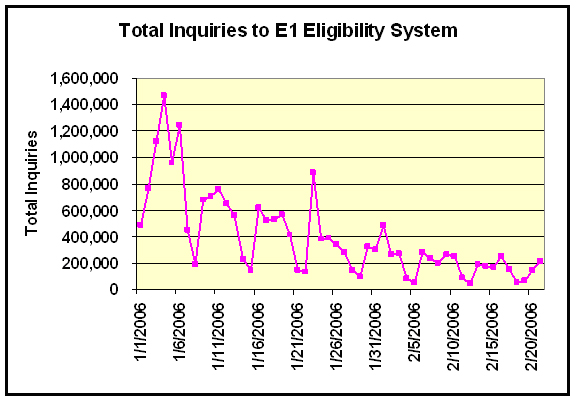
Figure 4: Total Inquiries to E1 Eligibility System Pharmacists can also call plans directly, on lines dedicated for pharmacists. They can contact Medicare�s own CSRs on the toll-free pharmacy support phone lines if need be, and CMS also has specially trained case workers in our regional offices who can intervene in special cases to make sure that enrollees get the medications they need. To help resolve issues pharmacists encounter in dispensing medications to those newly enrolled in the Medicare prescription drug plans, CMS has increased its call handling capacity at the pharmacist help line and the line is now available 24 hours a day. This increased capacity has reduced the wait time to less than a minute for pharmacists who want to use this mode of communication for eligibility and enrollment determination. CMS Supports Simplification Initiatives CMS has also identified a number of business process issues that can be simplified for plans, physicians and beneficiaries. On February 7, CMS posted to its website a model form for beneficiaries to use in requesting a coverage determination. The form was developed with input from the American Medical Association and others and is accompanied by instructions. We have also posted contact information for every drug plan for those wishing to pursue an appeal. To facilitate communications between pharmacists and physicians, we recently posted a form for pharmacists to use to inform physicians that their patient�s plan is requiring use of another drug, step therapy, or prior authorization. We have also encouraged plans to accept prior approval requests by fax, rather than requiring phone calls from physicians, since that is less time consuming for the physicians. We recently sent information to the plans which will expedite their processes for making sure they are not inappropriately paying for drugs that should be covered under Part B, and we have worked with Epocrates, an electronic prescribing software company, to ensure that their product provides accurate and easy access to plan formularies. We�ve also held weekly prescribers� conference calls and bi-weekly meetings with the AMA and other organizations to find out what prescribers are experiencing, to supply them with information on our activities and answer their specific questions. CMS issued a fact sheet February 24, 2006, to provide physicians with updated, practical information about the exceptions and appeals processes. This fact sheet describes the physician�s role in these processes and emphasizes the short decision making timeframes. Finally, CMS has identified a number of areas where plans can improve the data they transmit to the independent review entities that make appeals decisions and will be reiterating or extending its guidance to plans in this area. Medication Therapy Management Each Part D sponsor must have a MTM program for beneficiaries who have multiple chronic diseases and are taking multiple Part D drugs with annual costs of at least $4000. MTM programs may be furnished by a pharmacist or other qualified provider and must be developed in cooperation with pharmacists and physicians. This creates opportunities for the pharmacists to play active roles in the MTM services provided. To realize the full potential of MTM, quality metrics for MTM and related pharmacy services must be developed so that more can be done to support high-quality pharmacy care. To this end, on April 24th, CMS will convene a broad community of stakeholders to encourage the development of a Pharmacy Quality Alliance. Our goal is to help support the development of valid quality indicators and improved measurement of the value of pharmacy services. Similar to our efforts in support of the Ambulatory Care Quality Alliance and Hospital Quality Initiative, we will support a broad stakeholder effort to improve health care quality and patient safety in pharmacy care through a collaborative strategy for:
This dialogue should highlight the role of the pharmacist as a member of the integrated health care team and recognize the value the pharmacist can bring to the equation of total patient care. CMS may further support this collaborative process by developing a demonstration project to provide further evidence on the impact of MTM and other pharmacist interventions that could help promote high quality patient care and lower costs in both the Medicare and Medicaid programs � a win-win for plans, pharmacists, and most importantly, beneficiaries. There is still more CMS can do to assist pharmacists. CMS continues to engage in rigorous outreach to the pharmacy community, through national, state and local pharmacy organizations and their newsletters and email lists, as well as their standards organization and technical societies. Outreach efforts have also involved hundreds of town hall and state pharmacy association meetings around the country. We have held numerous national conference calls and posted extensive information on a portion of the CMS website dedicated to pharmacists. Specifically promoting the new pharmacy tools, we produced a CD-ROM that was distributed by all national associations, and held special training events around the country conducted by CMS pharmacists from our ten regions. We will continue our outreach efforts in the coming weeks. Physician Outreach Provides Information about Formularies, Exceptions, Appeals, and Expedited Requests Physicians are a key partner in the implementation of the Medicare prescription drug benefit and CMS conducted extensive outreach about formularies, exceptions, appeals, and expedited requests to promote effective interactions with pharmacists and beneficiaries. CMS used the Physicians Regulatory Issues Team (PRIT) website to provide advice for providers and an invitation for them to call or email CMS with issues or concerns about the Medicare prescription drug benefit. We have received and responded to over 200 emails from providers. In addition, CMS sent a letter to physicians outlining specific sources of help and information including the following.
CMS Works With States
CMS also engaged the States in a series of summits, conference calls, and workshops to discuss and address implementation issues associated with the MMA. These gatherings include monthly all-State conference calls; State Pharmacy Assistance Program (SPAP) Workgroup conference calls; and conferences hosted by organizations representing the States. In addition, CMS provided States with:
Finally, CMS has worked diligently with States to appropriately identify their full benefit dual eligible individuals. CMS validated the information that States reported to minimize reporting errors, mistakes, and omissions that may affect the identification of the States� full benefit dual eligible residents. These validation data matches achieved rates of over 99 percent for all States, according to an independent evaluation completed in the fall of 2005. Reimbursing States for Assisting in the Transition Process To that end, we have established a demonstration project to reimburse States for costs they incur by covering drugs that should be covered by the appropriate plan. Under the demonstration, Medicare will reimburse States by reconciling drug payments with prescription drug plans, and by paying any differential between the drug plan reimbursement and Medicaid costs, as well as certain state administrative costs. As of February 16, 2006, forty-five States and the District of Columbia have been accepted into the demonstration program. Of the States accepted into the demonstration program, about 15 did not activate their state payment systems and are seeking reimbursement only for administrative costs. CMS is asking States to implement steps to help assure that pharmacists have: checked enrollment status through a card, plan letter, or eligibility query; attempted to contact the plan or the Medicare line in case of incorrect copayments or coverage information (where phone wait times are reasonable); and, in the presence of evidence of Medicaid eligibility, billed through WellPoint. States that work with CMS to implement best practices like these to support pharmacists in using the new Medicare systems have already limited billing to their state systems, often to just a very small fraction of dual eligible beneficiaries and most States do not need to use their billing system at all. In New York, for example, claims fell from over 40,000 paid claims a day during the third week of January to less than 4,000 paid claims per day since February 16 after one modification in the system was made to ensure claims were processed in accordance with the interim billing instructions, which help assure that the Medicare drug plan is billed first. While daily payments to the pharmacists dropped to only a small fraction of total drug expenditures, CMS cannot draw firm conclusions until pharmacists have additional time to use the system. Of those States that are using their payment systems and have implemented steps like these, most have had only limited drug claims. For example, Florida has had fewer than 100 claims billed to its system and Pennsylvania has incurred fewer than ten thousand claims over the past two months. In these States, the State claims account for well under one percent and three percent, respectively, of the prescriptions for dual eligible beneficiaries. Among the small number of States that have the highest rates of claims billed to their state systems, most are including drug claims billed for other beneficiaries. For example, New Jersey, Connecticut, Maine and Vermont included claims for beneficiaries enrolled in state pharmacy assistance programs only some of whom are included as eligible in CMS� instructions to States for participation in the demonstration. Upon receipt of appropriate and correct claims data from a state, we plan to provide estimated payments within four weeks. CMS recently contracted with Public Consulting Group to coordinate claims processing, payment and reconciliation between the States and the Medicare prescription drug plans. On February 23, CMS extended the demonstration through March 8, 2006. If States are following our guidelines and acting as a payer of last resort, we will consider granting further limited extensions to the demonstration as necessary. At this time, States do not need to file separate extension applications. We are in weekly, if not daily communication, with the States and monitoring metrics such as claims volume. Monitoring Plan Compliance with CMS Requirements Extensive Plan Formulary Requirements Provide Access to Needed Prescription Drugs In addition, each Medicare prescription drug plan�s formulary was developed and reviewed by the plan�s pharmacy and therapeutics committee. Each formulary must be consistent with widely used industry best practices. Furthermore, CMS compared the prescription drug plans� use of benefit management tools to the way these tools are used in existing drug plans to ensure they are being applied in a clinically appropriate fashion. Prescription drug plan formularies typically include upwards of 80 percent of the 100 most commonly used drugs. In the long-term care setting, most Medicare prescription drug plan formularies are in general more robust than State preferred drug lists or commercial formularies. Plans must accommodate within a single formulary structure the needs of long-term care residents by providing coverage for all medically necessary medications at all levels of care. Coverage of all medically necessary medications may include, but is not limited to, alternative dosage forms such as liquids that can be administered through feeding tubes, intravenous medications, or intramuscular injections. CMS will review any request for deletion of a drug from a plan�s formulary to ensure continued access to a broad range of drugs. Plans cannot remove a drug from their formulary without, among a number of other steps, first obtaining CMS approval and providing a 60-day notice to their enrollees. In addition, CMS developed specific procedures for timely exceptions and appeals to ensure that enrollees receive prompt decisions regarding whether medications are medically necessary. Using those procedures, a Medicare beneficiary can get coverage for a drug that is not on a plan�s established formulary. For example, if the enrollee is requesting coverage of a non-formulary drug, the drug may be covered if the prescribing physician determines that all of the drugs on the formulary would not be as effective as the non-formulary drug or would have adverse effects for the enrollee, or both. The plan would have to review the physician�s determination and must make its decision as expeditiously as the enrollee�s health condition requires after it receives the request, but no later than 24 hours for an expedited coverage determination or 72 hours for a standard coverage determination. We are collecting information on the use of a plan�s appeals and grievance processes. Ensuring Pharmacists Receive Prompt and Accurate Payments from Plans Anticipating Next Steps CMS is continuing to work with the prescription drug plans to assure accurate and up-to-date information on all their dual eligible beneficiaries through additional file checking and more frequent data exchanges. We will continue to improve data translation among Medicare, the health plans, and States to continue reductions in the number of rejected or delayed transactions. CMS also is monitoring plans� customer service and hotline wait times, while also providing responsive service through 1-800-MEDICARE. Aggressive outreach, education, and monitoring efforts are continuing, with particular focus on the transitional coverage for a beneficiary�s current drugs. CMS continues to work with the States participating in the reimbursement program to assure effective use of Medicare coverage by connecting beneficiaries to their new Medicare prescription drug plans and helping pharmacists use Medicare backup systems if necessary. As implementation continues, and more and more beneficiaries select and enroll in a new prescription drug plan, CMS will continue to improve the program and problem solve, guided by the lessons we have learned to date. Conclusion Last Revised: March 2, 2006 |