Press Release
May 05, 2009
Flow of Potassium Into Cells Implicated in Schizophrenia
Blocking Errant Protein Could Stem Runaway Brain Activity in Psychosis
A study on schizophrenia has implicated machinery that maintains the flow of potassium in cells and revealed a potential molecular target for new treatments. Expression of a previously unknown form of a key such potassium channel was found to be 2.5 fold higher than normal in the brain memory hub of people with the chronic mental illness and linked to a hotspot of genetic variation.
An extensive series of experiments suggest that selectively inhibiting this suspect form could help correct disorganized brain activity in schizophrenia — without risk of cardiac side effects associated with some existing antipsychotic medications. Scientists at the National Institutes of Health and European colleagues report on threads of converging evidence in the May, 2009 issue of the journal Nature Medicine.
"The end game in linking genes with complex disorders like schizophrenia requires that we not only demonstrate statistical association, but also show how a gene version acts biologically to confer risk," explained Daniel Weinberger, M.D., director of National Institute of Mental Health's (NIMH) Genes Cognition and Psychosis Program, who led the research. "We found schizophrenia-like effects in brain circuitry and mental processing in perfectly healthy people who carry the risk-associated version of this potassium channel gene, even though they don't show any psychotic behavior."
Evidence suggests that schizophrenia stems from complex interactions between multiple genes and environmental factors. Several candidate genes have recently been statistically linked to the illness in large genome-wide association studies.
"Our study goes further, spanning discovery of a new gene variant, confirmation of its association with the illness, and multi-level probes into how it works — in human post mortem brain tissue, the living human brain, and neurons," added Weinberger.
By regulating the flow of potassium ions into the cell, potassium channels control when neurons fire — electrically discharge and release a chemical messenger that signals neighboring neurons in a circuit. This flow is regulated, in part, by activity of the chemical messenger dopamine, the main target of antipsychotic medications used to treat schizophrenia.
One type of potassium channel, called KCNH2, attracted the researchers' interest for its potential role in sustaining the type of neuronal firing that supports the higher mental functions disturbed in schizophrenia. Spurred by hints from postmortem studies of genetic variation linked to schizophrenia in the genomic neighborhood of KCNH2, the researchers analyzed the gene's association with the illness in 5 independent samples comprising hundreds of families. This pinpointed 4 variations associated with schizophrenia within a small region of the KCNH2 gene.
"Yet this statistical association didn't imply a mechanism," said Weinberger. "It didn't explain how KCNH2 might increase risk for schizophrenia. So we went back to the post-mortem brain tissue in search of an answer."
It was only then that the researchers discovered a previously unknown version of KCNH2, called Isoform 3.1, that soared to levels 2.5 times higher-than-normal in the hippocampus (memory hub) of people who had schizophrenia — especially those with the risk-associated variations. Isoform 3.1 was also higher-than-normal in healthy individuals who carried the risk-associated variations. This signaled the existence of a risk-associated version of the KCNH2 gene.
Healthy controls carrying the risk gene version also:
- Performed significantly worse-than-normal on measures of IQ and mental processing speed. Previous studies have linked similar performance with genetic risk for schizophrenia.
- Inefficiently processed memory in the hippocampus and working memory in the prefrontal cortex, as revealed by functional MRI (magnetic resonance imaging) scans. Although they performed similarly to controls on these tasks, their brains had to work harder to compensate for disordered tuning of circuitry — a phenomenon previously implicated in schizophrenia.
- Showed significantly decreased volume in the hippocampus — a heritable trait — in anatomical MRI scans.
In addition, Isoform 3.1:
- Showed levels 1,000 times lower in the heart than the other main form of KCNH2 and does not exist in lower animals, suggesting that it has evolved a unique role in the primate brain. Mutant forms of KCNH2 in the heart can lead to arrhythmias and even sudden death — a rare risk of taking antipsychotic medications, many of which interact with KCNH2. So targeting this brain-specific form potentially opens the way to development of new treatments free of such cardiac side-effects.
- Dramatically changed activity in rodent brains toward a neuronal firing pattern that may be important for thinking and memory tasks unique to primates.
- Is expressed much more prior to birth, compared to the other main form of KCNH2, suggesting that it plays a prominent role in the early stages of brain development.
- Is associated with a hotspot of variation in an area that controls gene expression, hinting that the suspect variations may contribute to schizophrenia risk by over-expressing Isoform 3.1.
Even though it is normally important for our higher order executive functioning, such over expression of Isoform 3.1 in schizophrenia could result in "abnormally increased neuronal excitability, runaway circuit activity and inefficient information processing," suggested Stephen Huffaker, Ph.D., the article's lead author, now a medical student at Harvard. The researchers propose that a treatment designed to inhibit just Isoform 3.1, might spare any heart-related side effects while improving the disorganized neural firing characteristic of the brain in schizophrenia.
In addition to the NIMH, researchers from the NIH's National Institute on Child Health and Human Development (NICHD) also participated in the research.
Reference:
A primate-specific, brain isoform of KCNH2 affects cortical physiology, cognition, neuronal repolarization and risk of schizophrenia. Huffaker SJ, Chen J, Nicodemus KK, Sambataro F, Yang F, Mattay V, Lipska BK, Hyde TM, Song J, Rujescu D, Giegling I, Mayilyan K, Proust MJ, Soghoyan A, Caforio G, Callicott JH, Bertolino A, Meyer-Lindenberg A, Chang J, Ji Y, Egan MF, Goldberg TE, Kleinman JE, Lu B, Weinberger DR.Nat Med. 2009 May 3.
A rat neuron modified to express Isoform 3.1, a variant of the KCNH2 potassium channel protein found to be genetically associated with Schizophrenia.
Source: NIMH Genes Cognition and Psychosis Program
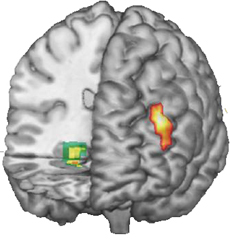
Areas in the prefrontal Cortex (right) and hippocampus (left) where activity differed in healthy control subjects during thinking tasks, depending on whether they had the risk version of the KCNH2 potassium channel gene. Functional magnetic resonance imaging data superimposed on 3-D MRI reconstruction of the brain.
Source: NIMH Genes Cognition and Psychosis Program
The mission of the NIMH is to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery and cure. For more information, visit the NIMH website.
The National Institutes of Health (NIH) — The Nation’s Medical Research Agency — includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. It is the primary federal agency for conducting and supporting basic, clinical and translational medical research, and it investigates the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit the NIH website.
