NIAID Researchers Developing Vaccine for Chlamydia
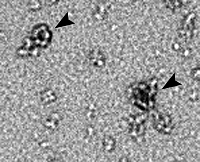 |
| This electron micrograph shows the flower-like structure of polymorphic membrane protein D (PmpD) after it was purified from the surface of the C. trachomatis bacterium. Scientists are hoping to develop PmpD into a vaccine candidate to prevent chlamydial infection. Credit: NIAID |
The bacterium Chlamydia trachomatis is among the oldest and most prevalent causes of infectious disease on earth. The World Health Organization (WHO) estimates that between 80 and 140 million people are infected with C. trachomatis, mostly women and children in developing countries, making chlamydia the most common bacterial disease in the world.
In the United States, chlamydia is perceived primarily as a “silent” disease that, despite showing no symptoms in more than half of the infected population, can damage reproductive organs and cause infertility. Chlamydia is the most reported sexually transmitted infection in the United States, and, in 2006, U.S. cases for the first time topped 1 million, according to the Centers for Disease Control and Prevention (CDC).
But in more than 50 developing countries, C. trachomatis is known for causing blindness. WHO estimates that untreated cases of the disease trachoma have left about 6 million people blind in Africa, the Middle East, Central and Southeast Asia, and Latin America. Trachoma causes eyelids to fold inward, so that the eyelashes rub the eyeball and scar the cornea, which can result in impaired vision and blindness.
In 1997, WHO coordinated a multinational program to eliminate blinding trachoma by 2020, called Global Elimination of Trachoma (GET2020). Because chlamydia is easily treated and cured with medical care, GET2020 has highlighted four areas for eliminating trachoma: eyelid surgery, facial cleanliness, environmental changes, and antibiotics.
Another focus of the WHO effort is to develop a vaccine to prevent chlamydial infection. One of the greatest challenges to fighting chlamydial infection is that people do not develop a sustained protective immune response to the infection. Understanding how C. trachomatis evades host immunity is central to developing a vaccine. That’s where NIAID scientists hope to contribute.
A Promising Re-Start
In 1975, Harlan Caldwell, Ph.D., now chief of NIAID’s Laboratory of Intracellular Parasites, was a graduate student at the University of Washington. He observed that blood samples from people who suffered different chlamydial diseases all appeared to have antibodies against the same protein antigen from C. trachomatis. He suspected that the antigen played a key role in the spread of disease, but at that time there was no equipment to further study the hypothesis.
The materials went into the freezer until, some 30 years later, while conferring with a colleague about C. trachomatis surface proteins, Dr. Caldwell recalled the earlier work. He had an idea of how to use new technology to study its potential to prevent C. trachomatis from spreading.
Now, based on successful initial laboratory test results, NIAID has sought patent protection on the concept, and Dr. Caldwell’s research group has begun to study animal models. But much work remains to be done to understand how C. trachomatis spreads and evades human immunity.
Deconstructing PmpD
Dr. Caldwell’s group is trying to confirm that the protein antigen he identified, known as polymorphic membrane protein D, or PmpD, has an active role in suppressing an immune response. That information could become the basis for a multivalent vaccine, or a vaccine that prevents infection from all 15 varieties of C. trachomatis. If PmpD indeed suppresses host immunity, then a vaccine that neutralizes PmpD could prevent infection and allow protective immunity to develop.
In its latest work, published online November 10, 2008, in Infection and Immunity, the group observed structural details of PmpD, showing that it exists in two forms that could each promote infection. Though they do not know the precise mechanisms involved, the scientists hypothesize that one form, found on the cell surface, is a flower-like structure that could help the bacteria attach to host cells and invade them. The other form is soluble; the scientists suggest its fragments could be released into the environment around a cell, where they act on and suppress cells involved in the immune response.
Understanding how these forms of PmpD function is critical to the design of a vaccine. Ultimately, as their work advances, Dr. Caldwell’s group will be trying to learn whether a PmpD-based vaccine can generate multi-functional, neutralizing antibodies that can block C. trachomatis infection.
back to top