|
Methods of Treatment
Cancer of the larynx may be treated with
radiation therapy,
surgery,
or chemotherapy.
Some patients have a combination of therapies.
Radiation therapy (also called radiotherapy)
uses high-energy x-rays to kill cancer cells. The rays are aimed at the tumor and the
tissue around it. Radiation therapy is local therapy. It affects cells only in the treated area. Treatments are usually given 5 days a week
for 5 to 8 weeks.
Laryngeal cancer may
be treated with radiation therapy alone or in combination with surgery or
chemotherapy:
Radiation therapy alone: Radiation therapy is used alone for small
tumors or for patients who cannot have surgery.
Radiation therapy combined with surgery: Radiation therapy may be used to shrink a
large tumor before surgery or to destroy cancer cells that may remain in the
area after surgery. If a tumor grows
back after surgery, it is often treated with radiation.
Radiation therapy combined with chemotherapy:
Radiation therapy may be used before, during, or after chemotherapy.
After radiation
therapy, some people need feeding tubes placed into the abdomen. The feeding tube is usually temporary.
|
These are
questions you may want to ask your doctor before having radiation therapy:
Why
do I need this treatment?
What
are the risks and side effects of this treatment?
Are
there any long-term effects?
Should
I see my dentist before I start treatment?
When
will the treatments begin? When
will they end?
How
will I feel during therapy?
What
can I do to take care of myself during therapy?
Can
I continue my normal activities?
How
will my neck look afterward?
What
is the chance that the tumor will come back?
How
often will I need checkups?
|
Surgery is an operation in which a doctor
removes the cancer using a scalpel or
laser while the patient is asleep. When patients need surgery, the type of
operation depends mainly on the size and exact location of the tumor.
There are several
types of laryngectomy (surgery
to remove part or all of the larynx):
Sometimes the surgeon also removes the lymph nodes in the neck. This is
called lymph node dissection. The surgeon also may remove the thyroid.
During surgery for cancer of the larynx, the surgeon may need to make a
stoma. (This surgery is called a
tracheostomy.) The stoma is a
new airway through an opening in the front of the neck. Air enters and leaves
the windpipe (trachea) and lungs through this opening. A
tracheostomy tube, also
called a trach (“trake”) tube, keeps the new airway open. For
many patients, the stoma is temporary. It is needed only until the patient
recovers from surgery. More information about stomas can be found in the
“Living with a Stoma” section.
After surgery, some
people may need a temporary feeding tube.
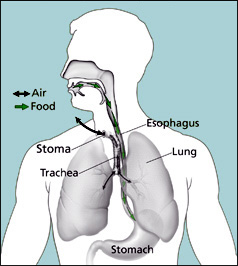
This picture shows the pathways
for air and food after a total laryngectomy.
|
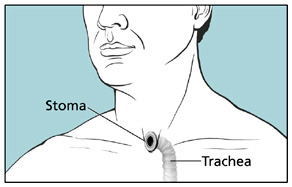
The stoma is the new opening into the trachea.
|
|
Here are some
questions to ask the doctor before having surgery:
How
will I feel after the operation?
Will
I need a tracheostomy?
Will
I need to learn how to take care of myself or my incision when I get home?
Where
will the scars be? What will they
look like?
Will
surgery affect my ability to speak?
If so, who will teach me how to speak in a new way?
When
can I get back to my normal activities?
|
Chemotherapy is the use of drugs to kill cancer cells. Your doctor
may suggest one drug or a combination of drugs.
The drugs for cancer of the larynx are usually given by injection into the
bloodstream. The drugs enter the
bloodstream and travel throughout the body.
Chemotherapy is used
to treat laryngeal cancer in several ways:
Before surgery or radiation therapy: In some cases, drugs are given to try to
shrink a large tumor before surgery or radiation therapy.
After surgery or radiation therapy: Chemotherapy may be used after surgery or
radiation therapy to kill any cancer cells that may be left. It also may be used for cancers that have
spread.
Instead of surgery: Chemotherapy may be used with radiation
therapy instead of surgery. The larynx
is not removed and the voice is spared.
Chemotherapy may be
given in an outpatient part of the hospital, at the doctor’s office, or at
home. Rarely, a hospital stay may be
needed.
|
These are questions you may want to ask your doctor before having chemotherapy:
Why do I need this treatment?
What will it do?
Will I have side effects? What can I do about them?
How long will I be on this treatment?
How often will I need checkups?
|
Back to Top
< Previous Section | Next Section > |