Skip directly to the search box, site navigation, or content.
Investigation Update: Outbreak of Salmonella Typhimurium Infections, 2008–2009
Update for April 29, 2009 (FINAL web update)
Today's Highlights

- The numbers of new cases have declined substantially since the peak in December, but illnesses are still being reported among people who ate the recalled brands of peanut butter crackers after the recall. The outbreak is expected to continue at a low level for the next several months since consumers unaware that they have recalled products in their home continue to consume these products, many of which have a long shelf-life. Consumers should avoid eating recalled products. (See consumer recommendations below).
- Case count is 714 in 46 states with latest confirmed, most recent reported illness beginning on March 31, 2009.
- Major national brands of jarred peanut butter found in grocery stores are NOT on the Peanut Corporation of America (PCA) recall list.
- Consumers may use FDA’s online database* to see if foods are on the recall list. Those without Internet access may call 1-800-CDC-INFO (available 24 hours a day, seven days a week) for product recall information.
- Timeline of Infections: Multistate Outbreak of Salmonella Infections Associated with Peanut Butter and Peanut Butter-Containing Products --- United States, 2008—2009 (PDF 149KB)
- CDC Podcast - Salmonella Typhimurium Outbreak in Peanuts - Update
- Information for Pet Owners: Questions and Answers Related to the Salmonella Typhimurium Outbreak and Pets
- Information for Veterinarians: Information Regarding Peanut Butter and Peanut-Product Recall and Pets
- Additional Advice for Consumers
- Salmonella Signs and Symptoms
- Multistate Outbreak of Salmonella Infections Associated with Peanut Butter and Peanut Butter-Containing Products --- United States, 2008--2009. Morbidity and Mortality Weekly Report, January 29, 2009 / 58;85-90.
- Salmonella Strains Tables for Outbreak Related to Peanut Butter and Peanut-Containing Products
- CDC Podcast - What Kids Need to Know About Peanut Butter and Salmonella
- CDC Podcast - Salmonella Serotype Typhimurium Outbreak in Peanut Butter and Peanut Butter-Containing Products
- CDC's Role During a Multi-State Foodborne Outbreak Investigation
- CDC’s Role in Food Safety
- CDC E-cards Related to Salmonella Outbreak
Outbreak Investigation | Recommendations/Advice to Consumers | Clinical Features/Signs and Symptoms | CDC's Role in Food Safety | Previous Updates
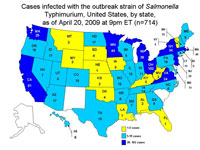
Persons Infected with the Outbreak Strain of Salmonella Typhimurium, United States, by State, September 1, 2008 to April 20, 2009
CDC is collaborating with public health officials in many states and the United States Food and Drug Administration (FDA) to investigate a multistate outbreak of human infections due to Salmonella serotype Typhimurium.
As of 9PM EDT, Monday, April 20, 2009, 714 persons infected with the outbreak strain of Salmonella Typhimurium have been reported from 46 states. The number of ill persons identified in each state is as follows: Alabama (2), Arizona (14), Arkansas (6), California (81), Colorado (18), Connecticut (11), Florida (1), Georgia (6), Hawaii (6), Idaho (17), Illinois (12), Indiana (11), Iowa (3), Kansas (2), Kentucky (3), Louisiana (1), Maine (5), Maryland (11), Massachusetts (49), Michigan (38), Minnesota (44), Missouri (15), Mississippi (7), Montana (2), Nebraska (1), New Hampshire (14), New Jersey (24), New York (34), Nevada (7), North Carolina (6), North Dakota (17), Ohio (102), Oklahoma (4), Oregon (15), Pennsylvania (19), Rhode Island (5), South Dakota (4), Tennessee (14), Texas (10), Utah (8), Vermont (4), Virginia (24), Washington (25), West Virginia (2), Wisconsin (5), and Wyoming (2). Additionally, one ill person was reported from Canada.
Among the persons with confirmed, reported dates available, illnesses began between September 1, 2008 and March 31, 2009. Patients range in age from <1 to 98 years. The median age of patients is 16 years which means that half of ill persons are younger than 16 years. 21% are age <5 years, 17% are >59 years. 48% of patients are female. Among persons with available information, 24% reported being hospitalized. Infection may have contributed to nine deaths: Idaho (1), Minnesota (3), North Carolina (1), Ohio (2), and Virginia (2).
On November 10, 2008, CDC's PulseNet staff noted a small and highly dispersed multistate cluster of 13 Salmonella Typhimurium isolates with an unusual DNA fingerprint or pulsed-field gel electrophoresis (PFGE) pattern reported from 12 states. On November 25, CDC's OutbreakNet team, working with state and local partners, began an epidemiologic assessment of that cluster, which had increased to 35 isolates. On December 2, CDC and state and local partners began an assessment of a second cluster of 41 Salmonella Typhimurium isolates. The PFGE patterns of the second cluster were very similar to the patterns in the first cluster and were first noted by PulseNet on November 24, as a cluster of 27 isolates that had subsequently increased to 41 isolates. Neither of these patterns were seen previously in the PulseNet Salmonella Typhimurium database. The clusters also appeared similar epidemiologically, so the two patterns were grouped together as a single outbreak strain, and the investigations were merged.
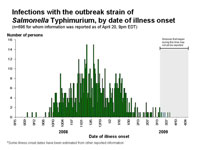
The outbreak can be visually described with a chart showing the number of persons who became ill each day. This chart is called an epidemic curve or epi curve. The epi curve and information about interpreting it may be found here. It shows that most illnesses began after October 1, 2008. Illnesses that occurred after March 16, 2009 may not yet be reported due to the time it takes between when a person becomes ill and when the illness is reported. This takes an average of 2 to 3 weeks. Please see the Salmonella Outbreak Investigations: Timeline for Reporting Cases for more details.
The numbers of new cases have declined substantially since the peak in December, but illnesses are still being reported among people who ate the recalled brands of peanut butter crackers after the recall. The outbreak is expected to continue at a low level for the next several months since consumers unaware that they have recalled products in their home continue to consume these products, many of which have a long shelf-life.
Consumers should check at home for recalled peanut butter containing products and discard them.
Outbreak Investigation
The investigation is ongoing, and CDC and state and local public health partners are continuing surveillance to identify new cases or ill persons and to interview ill persons to ask about a range of exposures to peanut butter and other peanut-containing products.
Peanut Butter
Preliminary analysis of the first national case-control study conducted by CDC and public health officials in multiple states on January 3 and 4, 2009, comparing foods eaten by ill and well persons indicates that peanut butter is a likely source of the bacteria causing the infections.
An investigation by the Minnesota Department of Health suggested King Nut brand creamy peanut butter as a likely source of Salmonella infections among many ill persons in Minnesota. The Minnesota Department of Agriculture Laboratory isolated the outbreak strain of Salmonella Typhimurium from an open 5-pound container of King Nut brand creamy peanut butter. King Nut creamy peanut butter is distributed in many states to establishments such as long-term care facilities, hospitals, schools, universities, restaurants, delis, cafeterias, and bakeries. It is not sold directly to consumers and is not known to be distributed for retail sale in grocery stores.
The Connecticut Department of Public Health Laboratory and the Georgia Department of Agriculture independently isolated Salmonella from unopened 5-pound containers of King Nut brand peanut butter. Officials in Connecticut have identified the Salmonella found in their container as the outbreak strain. Further tests are pending in Georgia to determine if the Salmonella in their container is also the outbreak strain.
The Michigan Department of Community Health isolated Salmonella from an unopened 5-pound container of King Nut brand peanut butter. They have identified the Salmonella found in their container as the outbreak strain. For more information, you may view a table that summarizes the several different strains of Salmonella identified during the outbreak investigation related to peanut butter and peanut containing products.
To date, 19 clusters of infections in five states have been reported in schools and other institutions, such as long-term care facilities and hospitals. King Nut brand peanut butter was present in all facilities.
Seven people from Colorado became ill in December and January and reported eating fresh, in store ground peanut butter purchased from one health food store chain. Preliminary information suggests that the peanuts came from the Peanut Corporation of America facility in Texas. However, the ultimate source of peanuts remains under investigation.
King Nut is produced by Peanut Corporation of America (PCA) in Blakely, Georgia. King Nut peanut butter was not sold directly to consumers but was distributed to institutions, food service providers, food manufacturers and distributors in many states and countries. Peanut butter and peanut paste is commonly used as an ingredient in many products, including cookies, crackers, cereal, candy, ice cream, pet treats, and other foods.
Other Peanut-Containing Products
To clarify whether other peanut-containing foods are associated with the outbreak, CDC along with state partners conducted a second national case-control study. Between January 17 and 19, 2009, telephone interviews were conducted with 95 persons who became ill with the outbreak strain and 405 well persons. Preliminary analysis of data received as of 9PM, Sunday, January 28, reveals an association between illness and consumption of pre-packaged peanut butter crackers, specifically with Austin and Keebler brands.
Austin and Keebler brand peanut butter crackers are produced by the Kellogg Company in North Carolina, using peanut paste from the Peanut Corporation of America. On January 14, 2009, the Kellogg Company put a precautionary hold on these peanut butter crackers, and on January 16 recalled these products. Other peanut containing products produced by a variety of companies may have been made with the ingredients recalled by PCA. CDC and state health departments continue to investigate the association of other brands and foods that contain peanut butter with illness.
Salmonella Typhimurium was isolated in Canada from Austin brand peanut butter crackers purchased in the United States. Officials in Canada have identified the Salmonella found in these peanut butter crackers as the outbreak strain. Salmonella resembling the outbreak strain was isolated by a private laboratory from three intact packages of Austin brand Toasty peanut butter crackers obtained from a patient’s home in Oregon. For more information, you may view a table that summarizes the several different strains of Salmonella identified during the outbreak investigation related to peanut butter and peanut containing products.
On February 6, Oregon public health officials confirmed that this Salmonella outbreak can also affect pets. One laboratory-confirmed case of Salmonella in a dog from an Oregon household was reported, and further characterization of this Salmonella isolate is pending. Salmonella resembling the outbreak strain was isolated by a private laboratory from recalled dog biscuits from this dog’s household. More information on how this outbreak may affect pets is available to consumers. Information for veterinary professionals is also available.
On January 28, 2009, PCA announced a voluntary recall of all peanuts and peanut products processed in its Blakely, Georgia facility since January 1, 2007. In addition to peanut butter and peanut paste, the expanded recall includes roasted peanuts and other peanut products and was based in part on laboratory testing information from the company. On January 28, 2009, the facility reported that production of all peanut products had stopped. For the latest information on the PCA recall, please visit the FDA website*.
More than 2833 peanut-containing products produced by a variety of companies may have been made with the ingredients recalled by PCA. The list of currently recalled products can be found on the FDA website*. FDA and the product manufacturers are working to determine the list of affected products, which may be extensive. Many companies have already announced whether their products include ingredients being recalled by Peanut Corporation of America, Georgia, and more companies are expected to make similar announcements. The current list of recall announcements from companies and more information about FDA’s investigation can be found at the FDA website*.
Recommendations
Based on available information, CDC and FDA recommendations include:
For consumers
- Consumers should avoid eating recalled products that contain peanut butter, including Austin and Keebler brand peanut butter crackers.
- Major national brands of jarred peanut butter found in grocery stores are NOT on the Peanut Corporation of America (PCA) recall list.
- Any product that is on the recall list should be disposed of in a safe manner. Any
recalled product should be thrown away to prevent Salmonella infections in
humans, pets, or other animals. This product should be disposed of in a closed
plastic bag and placed in a sealed trash can to prevent people or animals,
including wild animals, from eating it. - Consumers also should avoid eating products made with peanut butter,
peanut paste, or other peanut-containing products if they are unsure whether
these products have been recalled. - Consumers with pets should know that some pet foods and pet treats may contain peanut butter, including dog biscuits and bird food. If you have a recalled pet product
in your household, do not feed it to your pet or other animals. Consumers also should avoid feeding products made with peanut butter, peanut paste, or other peanut-containing products to their pets if they are unsure whether these products have been recalled. For more information about this outbreak and your pet, you may visit Questions and Answers Related to the Salmonella Typhimurium Outbreak and Pets. - To determine whether a product has been recalled, consumers can search the
list of recalled products at the Food and Drug Administration (FDA) website or
telephone the company that distributed the product at the phone number on the
package. - Consumers without internet access can telephone 1-800-CDC-INFO
(1-800-232-4636), 24 hours a day, 7 days a week, for product recall information
from the FDA website and for other information on salmonellosis. - Persons who think they might have become ill from eating peanut butter or
peanut-containing products should consult their health-care providers. - Infants, elderly persons, and persons with impaired immune systems are more
likely than others to develop severe illness.
For retailers
- Stop selling recalled products.
For directors of institutions and food service establishments
- Ensure that they are not serving recalled products.
For manufacturers
- Inform consumers about whether their products could contain peanut butter or other peanut-containing products from Peanut Corporation of America. If a manufacturer knows their products do not contain peanut-containing products from PCA, they should inform consumers of that.
To date, no association has been found with major national brand name jars of peanut butter sold in grocery stores.
For more information
- For the latest information about the epidemiological investigation, go to the CDC Salmonella Typhimurium Outbreak Investigation Update website.
- For the latest information about recalled products, go to FDA Salmonella Typhimurium Outbreak site*.
- More general information about Salmonella can be found on the CDC Salmonella website.
Public health officials will advise the public if more products are identified as being associated with the outbreak.
Clinical Features/Signs and Symptoms
Most persons infected with Salmonella develop diarrhea, fever, and abdominal cramps 12–72 hours after infection. Infection is usually diagnosed by culture of a stool sample. The illness usually lasts 4 to 7 days. Although most people recover without treatment, severe infections may occur. Infants, elderly persons, and those with impaired immune systems are more likely than others to develop severe illness. When severe infection occurs, Salmonella may spread from the intestines to the bloodstream and then to other body sites and can cause death unless the person is treated promptly with antibiotics.
More general information about Salmonella can be found here under Salmonella FAQs.
More information on this investigation can be found below.
- Connecticut Department of Consumer Protection press release
- Georgia Department of Agriculture
- Minnesota Department of Health and Minnesota Department of Agriculture press release
- Oregon Public Health Officials Confirm First Salmonella Case in Dog
- FDA – Salmonella Typhimurium Outbreak
- More information on Salmonella
CDC's Role in Food Safety
As an agency within the U.S. Department of Health and Human Services (HHS), CDC leads federal efforts to gather data on foodborne illnesses, investigate foodborne illnesses and outbreaks, and monitor the effectiveness of prevention and control efforts. CDC is not a food safety regulatory agency but works closely with the food safety regulatory agencies, in particular with HHS’s U.S. Food and Drug Administration (FDA) and the Food Safety and Inspection Service within the United States Department of Agriculture (USDA). CDC also plays a key role in building state and local health department epidemiology, laboratory, and environmental health capacity to support foodborne disease surveillance and outbreak response. Notably, CDC data can be used to help document the effectiveness of regulatory interventions.
Previous Updates on this Outbreak
- March 17, 2009
- March 10, 2009
- March 03, 2009
- February 24, 2009
- February 19, 2009
- February 17, 2009
- February 12, 2009
- February 09, 2009
- February 05, 2009
- February 02, 2009
- January 29, 2009
- January 26, 2009
- January 23, 2009
- January 22, 2009
- January 21, 2009
- January 20, 2009
- January 19, 2009
- January 17, 2009
- January 16, 2009
- January 15, 2009
- January 14, 2009
- January 12, 2009
- January 9, 2009
- January 8, 2009
Content Source: National Center for Zoonotic, Vector-Borne, and Enteric Diseases (ZVED)
Languages
Quick Links
Contact CDC