A Message from the NIDCR Director
 The National Institute of Dental and Craniofacial Research (NIDCR) remains committed to improving the oral, dental and craniofacial health of the nation. Our priority setting is driven by seeking a balance between scientific opportunity and the potential for our research to positively impact people’s lives.
The National Institute of Dental and Craniofacial Research (NIDCR) remains committed to improving the oral, dental and craniofacial health of the nation. Our priority setting is driven by seeking a balance between scientific opportunity and the potential for our research to positively impact people’s lives.
The future of the Institute will be shaped not only by the remarkable advances of modern science and technology, but also by the stark reality that our oral health community is at a crossroads. More than ever before, we need closer integration among research, practice and education to understand and eventually remediate the many disorders affecting the oral and craniofacial complex. Yet cutting-edge research and trends in dental education appear to be veering apart, posing unique challenges at a time when greater cross-talk among clinicians, scientists and educators is vital for progress.
Can we achieve a future in which smart, early interventions avert suffering from chronic orofacial pain, craniofacial disorders and oral cancer? Can we develop prevention and care delivery platforms that empower all Americans to preserve their oral health for their entire lifetime? Will we successfully bioengineer salivary glands and replacement teeth, or discover small molecules to prevent the formation of oral biofilms? Can the salivary glands be a gateway to the body for the delivery of precise molecular therapies with few side effects?
Each of these goals is attainable. We can realistically improve our own oral health and that of our children and generations to come through creativity, diligence and adherence to a strong commitment to evidence based and research-driven practice and health outcomes.
In charting a course for the next five years, my colleagues and I at the NIDCR have worked closely with our stakeholders to carefully consider the Institute’s strengths, opportunities and resources to derive a plan for how we can best map these to the oral health needs of the nation. Our strategic funding decisions consider emerging opportunities, successes and failures on an ongoing basis to inform programmatic activities.
Collectively, this input yields a highly diverse range of opinion and perspective. It has helped to paint a picture of how the NIDCR should evolve to successfully achieve its mission to improve the oral health of the American public. It is clear that the oral, dental and craniofacial community must remain multifaceted and diverse, so that our future investments can transform many areas simultaneously.
Moving forward, the 2009-2013 NIDCR Strategic Plan is built on four key goals: widening our scope of inquiry, strengthening the research pipeline, fostering novel clinical research avenues, and eliminating oral health disparities.
Widen the Scope of Inquiry. The tools of modern science show us that diseases have no disciplinary boundaries. Our best chance for understanding complex diseases such as cleft lip and cleft palate, dental caries, chronic pain and oral cancer is to embrace the newest technologies and advances as well as to open our doors to expertise from different fields. Thus, our first strategic goal asserts that it is critical that we bring the best science to bear on problems in oral, dental and craniofacial health through multi- and interdisciplinary research. This investment requires a healthy marriage between creative individual investigator-driven research and team science approaches.
Keep the Pipeline Strong. Our second strategic goal is to strengthen the workforce of researchers dedicated to solving urgent problems in oral, dental and craniofacial health. We need to work hard to draw curious minds to oral health research—it is our responsibility to inspire and support the next generation of scientists from a diverse array of backgrounds and biomedical and behavioral disciplines. Our future depends on training the scientists of tomorrow and giving them the opportunities to make discoveries.
Promote Clinical Innovation. Today, we are on the verge of many opportunities to develop tailored, preemptive oral health care. Targeted and more facile diagnostic tests, new drugs and biologics, practice-based research venues, and culturally sensitive behavioral interventions will provide novel clinical avenues to improve oral, dental and craniofacial health. Promoting innovative clinical research, our third strategic goal, requires not only resources but also a new mindset to embrace and apply new approaches to solving old problems.
Address Health Disparities. The most challenging issue we face as health professionals, educators and scientists is the stubborn reality that health disparities continue to exist in our country. We must improve our understanding of what causes inequality at individual, community and societal levels. This knowledge will inform the development of practical and culturally appropriate interventions. Thus, our fourth strategic goal is to apply rigorous, multidisciplinary research approaches to eliminate disparities in oral, dental and craniofacial health by improving health in diverse populations.
Now is the time to showcase the integral importance of oral, dental and craniofacial research toward solving problems in health and informing our understanding of many different diseases and conditions. As always, I welcome your continued input as we strive to improve the nation’s oral health through sound science.
Lawrence A. Tabak, D.D.S., Ph.D.
Director, NIDCR
Strategic Goals and Objectives
The 2009-2013 NIDCR Strategic Plan provides a guide for the Institute’s funding decisions and defines the areas that will be closely monitored for key developments and innovations that can be applied to oral, dental and craniofacial health. The Goals and Objectives presented throughout this Plan strike a careful balance between basic and applied research; address workforce issues; and confront the vexing problem of health disparities. Clearly, the Goals and Objectives herein do not encompass the entire range of NIDCR-supported research that collectively contributes to our overall mission, but they do capture the areas that offer the most significant scientific promise in the near term. We will continue to monitor new discoveries across NIDCR’s portfolio of research and to pursue emerging opportunities to further enhance our progress.
Goal I: Bring the best science to bear on problems in oral, dental, and craniofacial health.
Science is advancing rapidly and the next generation of technological innovation may greatly accelerate the next breakthroughs in oral, dental and craniofacial research. Researchers have created prototypes for “labs-on-a-chip,” bioengineered tissue replacements, and developed powerful molecular imaging tools that provide a new window into complex biological systems about which we continue to learn. This emerging wave of knowledge and tools will accelerate the development of molecular-based oral health care, and thus it is vital that the NIDCR support a diverse portfolio of research to achieve that end.
Objective I-1: Integrate molecular, clinical, and population health approaches to improve diagnostics and optimize outcomes.
Most oral diseases and disorders arise from the interplay of complex biological, behavioral, environmental and genetic factors. Scientists now have the tools to understand health and disease from a powerful systems perspective. Such deep insights will enhance our ability to predict and more effectively manage many oral, dental and craniofacial disorders. However, understanding and addressing complex oral diseases will take more than figuring out the molecular pieces of the puzzle. It will require melding these advances with state-of-the-science clinical and epidemiological approaches to more precisely identify diseases at their earliest inception, direct individualized therapies, and predict disease outcomes.
The NIDCR will support a variety of efforts to integrate the basic, clinical, and population sciences to help clinicians devise prevention strategies, early detection and diagnostic tools and personalized therapies. Oral health research stands to benefit greatly from this complementary and integrated approach.
One area that offers great opportunity is oral and pharyngeal cancer, which kills more than 8,000 Americans each year. These deaths are particularly tragic because, in most cases, detection and treatment of early stage oral cancer results in much higher survival rates than if the disease is diagnosed and treated at late stages. Despite annual U.S. spending of approximately $3.2 billion1 on head and neck cancer treatment, relative survival rates have not improved during the past 16 years and remain among the lowest of all major cancers. Oral cancer survival among African American men has actually decreased2. The NIDCR will support development of a multifaceted program that integrates several new technologies and methods into a clinical protocol aimed to improve oral cancer detection and survival. Approaches under development include devices to aid in earlier detection: rapid gene-expression measurement tools that assess suspicious lesions removed for biopsy and integration of screening, diagnosis and treatment. For example, toward achieving this goal, NIDCR-supported researchers recently devised a customized optical device3 that allows clinicians to visualize in a completely new way areas in the oral cavity that may be developing oral cancer. An Institute priority is to conjoin these efforts with the results of research to reduce oral cancer in high-risk groups. Approaches include genetic association studies and research on improving community outreach, education and behavioral modification.
Dental caries, or tooth decay, offers another prime example where an integrative approach could offer new therapeutic insights. Over the last several decades, dental researchers have made tremendous progress in defining events in the decay process and learning how to reverse them. However, identifying more precisely the genes and pathways that characterize decay will allow scientists to more clearly define how bacteria thrive and communicate within a biofilm. The Institute will also support research to further develop and refine sensitive imaging tools that will enable detection of the earliest signs of enamel demineralization. Approaches to halt and remineralize these early lesions would save the tooth from further decay and avert the need for invasive restorations. Recognizing the role of oral health behavior in tooth decay--and especially the role of families in the development of childhood caries--the Institute seeks to recruit the interest of behavioral science experts to investigate the role of behavioral change in oral health improvement.
The integration of existing knowledge with the results of genetic, behavioral, epidemiological and clinical studies will identify practical solutions to confront stubbornly evasive diseases such as oral cancer, caries, HIV/AIDS-associated oral diseases and other conditions.
Objective I-2: Increase the Institute’s commitment to basic and applied research in the behavioral and social sciences.
Community characteristics and the organization of health care systems are key aspects of the social context that contribute to oral health. Many of the opportunities for improving oral health lie in achieving behavioral, lifestyle and social changes—objectives that are shared with many other scientific areas.
Drawing from the expertise of diverse fields within the social and behavioral sciences presents an important opportunity to develop models and approaches that will produce meaningful improvements in oral health. This approach dovetails with the view of oral health as an essential component of general health as cited in the Surgeon General’s report on oral health in America (2000)4.
The NIDCR will seek to engage researchers in child development, family theories, social systems, geriatrics, and treatment adherence to broaden the understanding of oral health and frame new approaches to improve it. Other vital areas for NIDCR investment include behavioral interventions in non-dental settings, interventions for reducing risk behaviors and the integration of evidence-based health recommendations into communities. Recognition of multiple principal investigators on NIH research applications5 should smooth the way for such collaborations across and within disciplines.
Objective I-3: Embrace and support genetic, genomic, and proteomic research approaches to address oral, dental, and craniofacial diseases.
The NIDCR will prioritize research that exploits advances in the genetics, genomics and proteomics of dental, oral and craniofacial diseases. The development of quantitative approaches to better understand the developmental and physiological circuitry underlying craniofacial structures in both health and disease will play an increasingly important role. Bioinformatics and computational approaches are necessary to integrate, analyze and model the large data sets generated by these modern research tools. The Institute will encourage efforts to share bioinformatics platforms between intramural and extramural projects.
The emerging science of genome-wide association studies, or GWAS, and other rapidly evolving genome-wide technologies is producing exciting findings in oral, dental and craniofacial health, including those from an ongoing NIDCR-funded GWAS of oral clefts and dental caries. A recent family-based genome-wide linkage study indicated possible developmental links between cleft lip and/or palate, caries and a range of dental malformations6 and identified several candidate genes for caries risk, pointing unexpectedly to genetic loci for salivary flow and diet preference7. The NIDCR’s continued support of genomic approaches may yield important new insights into the causes and progression of other complex conditions such as temporomandibular muscle and joint disorders associated with chronic orofacial pain, oral cancer, periodontal diseases and Sjögren’s syndrome.
In addition to funding innovative, investigator-initiated genomics and proteomics projects, the NIDCR supports the recently launched FaceBase Consortium8. This project will establish a publicly available database to serve as a resource that will promote enhanced understanding of the genetic and environmental influences that drive craniofacial development. These efforts will likely yield new opportunities for preventing and treating craniofacial defects. The FaceBase Consortium will provide researchers a portal and a platform to provide access to large data sets. This will facilitate the analysis, integration and dissemination of research results, fostering interactions and collaborations with the Consortium and with the broader scientific community. The Consortium also will house projects for the development of novel methods and technologies that could be applied to probe molecular, cellular, and physiological processes during craniofacial development.
Objective I-4: Promote the oral cavity as a model for understanding other organ systems and diagnosing a range of health conditions.
NIDCR-supported research using the oral cavity as a research tool and delivery platform will pave the way to a future of targeted therapies for a range of conditions. Therapeutic manipulation of immune and/or humoral responses through gene delivery approaches such as RNA interference via the oral cavity may lead to better control of autoimmune diseases such as Sjögren’s syndrome, which destroys salivary function and the production and secretion of tears. Another expected benefit of immune modulation via the mouth is the potential for novel ways to halt the chronic inflammation that causes periodontal disease, a condition that affects an estimated 80 percent of U.S. adults and has a well-documented link with diabetes9, 10.
Saliva-based diagnostic tests offer significant potential for improving both oral and general health. Thus further development and validation of these approaches will enable improved pre-emptive care by detecting molecular markers predictive of disease before symptoms arise, or by providing diagnosis of the earliest signs of disease. Recently, a consortium of NIDCR-supported research groups compiled the first comprehensive list of proteins secreted by the major salivary glands11, leading to a compendium of salivary proteins that will form the basis for future efforts in salivary diagnostics and therapeutics.
The NIDCR participates in the trans-NIH Human Microbiome Project12, which will lay a foundation for efforts to explore how complex communities of microbes interact with the human body to influence health and disease. This project supports the development of innovative technologies and computational tools; coordination of data analysis; and an examination of ethical, legal and social implications of human microbiome research. The choice of five sampling sites—the skin, vagina, gastrointestinal tract, nose and oral cavity—will enable a broad-based discovery approach that will have important implications for systemic health in addition to oral, dental and craniofacial health.
Objective I-5: Facilitate reconstruction and regeneration of diseased or damaged oral and craniofacial tissues and organs through biological, bioengineering and biomaterials research approaches.
The NIDCR has a longstanding interest in oral, dental, and craniofacial tissue and organ reconstruction and regeneration, and was a pioneer in the study of the chemical properties and molecular structure of collagen and other extracellular matrix components--key elements of bones, teeth and the periodontium (the tissues that surround and support teeth). The ultimate goal of tissue engineering and regenerative medicine is to create, rebuild and preserve permanent, functional tissues by applying both biological and engineering principles. Future effort capturing new knowledge in developmental biology, immunology and computational modeling provides unprecedented opportunity to develop biomimetic and bioengineering tools that coax the body to repair itself. Creating fully functional craniofacial bone, salivary glands, and artificial teeth with performance properties equivalent to natural tissues or organs is also an Institute priority area with potential for significant impact on a range of conditions.
NIDCR-funded research in craniofacial tissue and organ reconstruction not only will inform approaches to correct craniofacial birth defects, but also address the urgent needs of the thousands of Americans who suffer disfiguring wounds and chronic pain from accidents or military conflicts. Through the integration of tissue engineering and regenerative medicine, biomaterials approaches, nanotechnology efforts, and stem cell research, NIDCR-supported scientists will create new options for reconstructing malformed parts of the craniofacial complex or injured tissues of the face and head caused by severe trauma. Cutting-edge techniques, such as stem cell-mediated regeneration, have the potential to supplant the use of artificial materials--metals, plastics, and latex—that are limited in their ability to functionally replace missing structures.
Even today, virtually everyone in the U.S. is at risk for tooth decay, which remains the single most common chronic childhood disease--five times more common than asthma13. Despite steady progress in learning how to better formulate and cure, or harden, dental composites in a damaged tooth, large composites shrink and stress the teeth to which they are bonded. Recent estimates say that a general dentist spends 70 percent14 of his or her time replacing dental restorations that result from secondary decay and/or restoration fracture. It thus will be important to improve our ability to predict and design the structural and mechanical properties of dental materials. The NIDCR will support research that explores whether oral biofilms accelerate the degradation of dental resin composites, leading to secondary decay and restoration failure as previous studies have suggested. The Institute will also support research toward a new generation of materials, including nanocomposites and smart self-healing materials with enhanced adhesive bonding to a tooth’s surface, improved durability, better aesthetics, and maximum biocompatibility.
Goal II: Strengthen the pipeline of researchers dedicated to solving problems in oral, dental and craniofacial health.
Scientific research holds great promise for targeted prevention and treatment strategies, and thus it is vital that oral health care become more science-based in the coming years. The oral health community must ready itself for fuller integration into the primary health care network. Developing and maintaining a robust and diverse pipeline of oral, dental and craniofacial researchers is the best way to assure that evidence-based oral health comes to fruition.
Objective II-1: Encourage schools of dentistry to create vibrant research pathways for students and faculty.
The oral cavity offers unique attributes for basic and clinical research, and so the dental research community can contribute to biomedical research at multiple levels. However, there is a relative scarcity of dentist-scientists who receive competitive funding from the NIH. Researchers in schools of dentistry now receive less than half of the NIDCR extramural budget, and this proportion has been steadily decreasing with time (See Figure 2).
The need to act now is urgent: While it is important to welcome, and retain, the expertise and different viewpoints of researchers outside of traditional dentistry, we must continue to maintain a critical mass of investigators with a unique and intimate knowledge of orofacial structures. The high demand for dental clinicians, coupled with the onerous level of indebtedness of many dental school graduates, has led the large majority of dental school graduates to pursue careers in private practice.
Yet, if the oral health community is to assume an authoritative position in primary health care by contributing creatively and substantially to the evidence research base, it is essential that we recruit, educate and train future scientific leaders in academic dentistry. Attracting such students requires that schools of dentistry establish research paths, and then identify and mentor students poised to pursue research career training.
The NIDCR will continue to provide leadership for rigorous training and career development that promote interest in academic dentistry (see Objective II-2 below).
Objective II-2: Emphasize the training and career development investment of individuals.
Currently, the NIDCR offers a range of training opportunities for both individuals and institutions at the pre-doctoral and post-doctoral levels, along with combined-degree programs (D.D.S./Ph.D.). Mentored career development programs at the post-doctoral level and the recently introduced K99/R00 Pathway to Independence15 award encourage early-stage investigators to achieve earlier scientific independence. Other NIDCR training programs encourage independent scientists to update their skills or make career changes; provide salary support; or provide protected time for research.
Recently, NIDCR staff undertook an analysis of training data to assure that the Institute’s research training investment is targeted to best achieve its goals. NIDCR staff ascertained the professional outcomes of NIDCR trainees and examined data from the annual survey of U.S. schools of dentistry conducted by the American Dental Education Association. This analysis demonstrated that those trainees who are supported by an individual fellowship are more likely to obtain independent NIH research funding, particularly with respect to R01s, than those supported by an institutional training grant. These data revealed that a significantly higher proportion of faculty with prior NIH career development (K) awards were in full-time employment than were those who had prior NIH training grant or other NIH fellowship award support (T- and F- awards, respectively).
The NIDCR will therefore increase its emphasis on individual awards, shifting research training away from institutional awards. The Institute will also expand its pre-doctoral research training pool by reissuing the institutional training grant program as a T90/R90 mechanism that will allow support of foreign-trained, non-U.S. citizen dentists for Ph.D. degree and postdoctoral training. This pool of talented young investigators has not been tapped because of restrictions on the standard NRSA programs; however, the Institute believes these individuals could significantly enhance the value and outcome of NIDCR institutional training programs. The NIDCR has also joined the NIH-wide solicitation to support pre-doctoral Ph.D. trainees on F31 individual fellowships, and will continue efforts to recruit and retain new and early-career investigators in oral health disparities research to ensure future research capacity.
The Institute will also partner with schools of dentistry to provide the training and mentorship that emerging clinician scientists require (see Objective III-4 below).
Objective II-3: Welcome new disciplines poised to expand oral, dental and craniofacial research.
As a discipline, oral health research offers a unique window of accessibility to study inflammation, microbial biofilms, bone metabolism and repair, and exocrine glands and their secretions in real time. The NIDCR strongly believes that now is the time to proactively communicate the value of oral, dental and craniofacial research as it relates to the larger biomedical construct.
Offering new programs to recruit and train Ph.D. students and postdoctoral fellows trained in other areas of biomedical research to dental and craniofacial research careers may be a fruitful approach to tap a robust source of new independent investigators. To attract these individuals to pursue research topics relevant to the mission of the NIDCR, the Institute will develop mechanisms to support non-dentist Ph.D.s to receive two years of training in an area of oral pathobiology. In addition, the NIDCR will develop a new infrastructure program designed to encourage the recruitment of new faculty into oral health research and provide much-needed, state-of-the-art equipment to conduct modern scientific research. The Institute will also explore ways to engage behavioral and social scientists in oral health research (see Objective I-2). These opportunities may include oral health training and mentoring for early-career investigators, oral health retraining and networking for established investigators from other fields, and funding for translational research that applies cutting-edge behavioral or social science methods or constructs toward improving oral health. Because it will always be important to retain dental expertise within scientific teams pursuing oral health issues, the current environment presents a good opportunity for cross-disciplinary training that can build the next generation of dental/non-dental research teams.
There is also an urgent need to introduce under-represented groups into the dental research pipeline, since current numbers neither reflect the U.S. population as a whole, nor the census of dentists in training across the nation. One of the NIDCR’s highest priorities will be to emphasize training and career development programs for scientists from diverse backgrounds.
Goal III: Identify innovative clinical research avenues to improve oral, dental and craniofacial health.
The nation’s progress against oral diseases will be accelerated by rigorous clinical studies whose outcomes have the potential to fundamentally change dental practice and improve oral, dental and craniofacial health. Research designs and analytic methods that enhance the efficiency and lower the cost of clinical studies are needed--in particular, the use of biomarkers as surrogate endpoints, the availability of more accurate and sensitive validation reference standards, and the development of more accurate measures of disease susceptibility. The NIDCR recognizes the need for partnering with the extramural research community, professional and scientific organizations, industry, and other public and private institutions that can facilitate the development of new approaches and technologies to enhance the conduct of oral disease clinical trials.
One particularly important venue for cross-disciplinary collaboration is the Clinical and Translational Science Award (CTSA) program16This NIH-funded national clinical research consortium is transforming how clinical and translational research is conducted across the country. The NIDCR strongly encourages its investigators to interface with the CTSAs to take full advantage of this important resource. At the end of fiscal year 2008, 23 schools of dentistry and programs were actively participating in this program that also offers multi-disciplinary training to junior clinical researchers.
Objective III-1: Conduct well-designed, definitive clinical research studies that improve oral, dental and craniofacial health and support more effective care delivery and health policies.
The NIDCR is committed to identifying effective preventive, diagnostic and treatment approaches for craniofacial, oral and dental diseases. The Institute’s highest priority in this area will be to fund clinical trials that can provide scientific evidence to change clinical practice or health policy. The Institute will support all stages of innovative treatment approaches to facilitate the translation of science into clinical practice. Areas of interest for NIDCR-supported clinical investigations include:
- early detection and identification of risk factors for dental caries, periodontal disease, oral cancer, orofacial clefts, Sjögren’s Syndrome, HIV/AIDS-associated oral diseases and chronic orofacial pain;
- interventions based on relationships between oral infectious diseases and other conditions such as diabetes and pulmonary disease;
- novel treatment strategies for chronic oral health disorders and diseases including orofacial pain associated with temporomandibular muscle and joint disorders as well as oral cancer;
- prevention and treatment of oral disease in underserved populations;
- new approaches for preventing and treating mucosal infections;
- investigations of mechanisms leading to salivary dysfunction associated with Sjögren’s syndrome; and
- evaluation and treatment of skeletal diseases and craniofacial malformations.
The NIDCR’s intramural research program provides a valuable opportunity to conduct translational and clinical research relevant to the mission of the Institute. In particular, this program takes advantage of the combined expertise and resources, including the NIH Clinical Center, available to the thousands of researchers from various ICs working on the NIH campus in Bethesda, Maryland. NIDCR intramural scientists, as appropriate, translate basic research findings into phase I clinical trials of novel treatments to evaluate their safety in people.
Over the next five years, intramural scientists will conduct clinical studies including a targeted oral cancer therapy; the use of adult stem cells to heal wounds with new bone; and development of a unique compound that can selectively delete specific cells from the nervous system that produce intractable chronic pain.
Objective III-2: Support practice-based research and create a national-level dental practice collaborative for community-based research and oral health surveillance.
The capacity of the oral health research community to conduct clinical research and to use science-based findings depends on a critical mass of investigators skilled in the design and conduct of clinical trials and community-based research. The NIDCR will support oral health scientists and practitioners with specific expertise in areas such as prevention and health promotion, diagnostic technology, drug development and testing, and community-based investigations, as well as in translational research.
In 2005, the NIDCR awarded three 7-year grants to establish practice-based research networks (PBRNs) that are conducting well-designed clinical studies that address everyday issues in the delivery of oral health care. The impetus behind the networks is the need for science-based data to guide dental treatment decisions. Each regional network conducts short-term clinical studies that compare the benefits of different dental procedures, dental materials, and prevention strategies under a range of patient and clinical conditions. Other network projects, such as surveys and de-identified reviews, as allowed by the Health Insurance Portability and Accountability Act, estimate disease prevalence, treatment trends, and the prevalence of less common oral conditions among individuals accessing dental care.
The success of the PBRNs, or any practice-based collaborative program, depends on a focus on real-world clinical issues and the capacity to generate information that will be of practical value to practitioners and patients alike. It is critical that these studies center on topics and procedures that clinicians themselves identify as relevant and helpful to their clinical decision making. Over the next five years, the NIDCR will support a second generation of practice-based research efforts that will build and expand on the work undertaken thus far.
Objective III-3: Provide resources to promote product and clinical development toward the ultimate commercialization of oral health therapies.
Looking forward, it is important that the NIDCR adopts the most innovative technologies to advance the development of novel oral health products and therapies. To accelerate technology development, the Institute will fund interdisciplinary research approaches with an emphasis on basic and translational studies. Biomimetics, nanotechnology and nanoscience, diagnostic technologies, stem cell research and materials science (including biocompatibility), and the use of technologies to deliver evidence-based behavioral interventions all fall within the sphere of this research area. In order for these discoveries to improve health and quality of life, they need to be incorporated into everyday practice. For that reason, the Institute will emphasize technology transfer as an important research component and will support small business innovation grants to help speed the translation of scientific findings into practice.
The NIDCR is a leader in the development of saliva-based diagnostic tests for a variety of diseases and conditions, including oral cancer. Miniaturization of detection devices will ultimately allow for the placement of a sentinel device directly in the mouth, potentially yielding real-time surveillance of hundreds of biomarkers that could alert people to consult their health professionals at the earliest sign of disease. Adequate technologies to develop salivary diagnostics on a large scale do not yet exist, but are essential for creating a battery of tests and diagnostic panels for predicting or detecting the onset and progression of diseases. The Institute will support research to develop such technologies as the first step in building the scientific infrastructure required to expand salivary diagnostics. Already, NIDCR-funded scientists have begun to evaluate which of the gene products in saliva correlate with various disease processes by completing the first full catalogue of salivary proteins17.
Objective III-4: Ensure breadth and depth of the clinical research pipeline, fostering collaboration between oral health care practitioners, clinical scientists and basic researchers.
The capacity of the oral health research community to conduct clinical research, and to use the findings from that research, needs to be augmented through enhanced training and the creation of an able cadre of scientists skilled at conducting clinical trials and community-based research.
The NIDCR provides several opportunities for combined D.D.S./Ph.D. training. These include:
- an institutional T32 grant program to provide support for an integrated dental and graduate research training program leading to both the D.D.S./D.M.D. and Ph.D. degrees;
- individual predoctoral dental scientist fellowships that broaden the reach of the T32 program by providing individual fellowships to dental scientists at any school of dentistry in the U.S.; and
- the Dental Scientist Training Program (DSTP), modeled after the highly successful Medical Scientist Training Program18 supported by the National Institute of General Medical Sciences.
A recently conducted NIDCR research training program analysis highlighted the troubling pipeline trend that few NIDCR dental school trainees go on to independent research careers. The evidence suggests that dentists are not as successful as those without dental degrees in obtaining independent research funding.
The Institute believes that providing the support for dentist-scientists to obtain high-quality postdoctoral training with protected research time will help them to be more competitive for subsequent, independent awards. Currently, many dentist-scientists do not have a dedicated period of postdoctoral research training, as do their non-dentist Ph.D. counterparts, because most dentists, including dual-degree dentists, combine clinical residency and postdoctoral research experiences. To address this issue, the NIDCR will create a new career development pathway that will enable the Institute and schools of dentistry to work together to provide training and mentorship for clinician scientists. The NIDCR will also introduce a modified K99/R00 award mechanism (see Objective II-2) to enable dentists to pursue a rigorous mentored postdoctoral research experience in a first phase, followed by independent tenure-track support in a second phase.
The NIDCR also encourages the oral health research community to develop and maintain clinical research partnerships with other components of academic health centers, the practicing community, and other sites that support multidisciplinary research teams. In particular, the Institute strongly encourages partnerships that make use of the resources of the NIDCR intramural program and the CTSA consortium (see Goal III).
Goal IV: Apply rigorous, multidisciplinary research approaches to eliminate disparities in oral, dental and craniofacial health.
As the NIDCR moves closer to unlocking the secrets of biology that will benefit the oral health of millions of Americans, the Institute is also keenly aware that many scientific discoveries do not reach all people. This leads to disparities in the health and health care among various groups in the U.S. due to a complicated array of reasons that are still poorly understood and deserving of research. The NIDCR will continue to support studies that will provide a better understanding of the basis of health disparities; to develop and test interventions tailored to underserved populations; and to foster dissemination and implementation research to assure that research findings are translated into practice, policy and action in communities.
Objective IV-1: Identify the full range of factors that contribute to oral health inequality.
The NIDCR will prioritize research that seeks to understand the determinants of inequality in oral health status and quality of life. Studies that explore the root causes of inequality at individual, community and societal levels--as well as those that explore genetic, behavioral, psychosocial and environmental interactions--will serve as the underpinnings for future health disparities interventional research.
The Institute will tackle these problems by funding multidisciplinary teams of anthropologists, behavioral and social scientists, health policy analysts, health services researchers, economists and others to develop prevention and treatment approaches that are effective and practical in populations with health disparities. The Institute will continue its commitment to enrolling and retaining women, children, racial and ethnic minorities and other underrepresented groups in NIDCR-funded clinical research, and emphasize clinical research that meets the needs of specific, vulnerable underserved populations. These efforts will be enhanced by community-based partnerships.
Objective IV-2: Support interventional, dissemination and implementation research to reduce oral health disparities.
The NIDCR will support interventional research that will have a meaningful impact on caries, oral and pharyngeal cancer, and periodontal disease, and that will influence clinical practice, health policy, community and individual action and ultimately eliminate disparities in vulnerable people. The Institute has catalyzed the conduct of interventional health disparities research through its Centers for Research to Reduce Disparities in Oral Health program, which provides a venue for the interaction among scientists from a wide array of disciplines. These multidisciplinary teams target oral health issues in underserved communities, integrating the expertise of oral health professionals, sociologists, economists, anthropologists, psychologists, communications specialists and other health practitioners and researchers. The NIDCR will also fund health disparities interventional research beyond that conducted through the Centers for Research to Reduce Disparities in Oral Health program.
One significant return from the NIDCR’s investment in interventional health disparities research comes from a randomized clinical trial conducted by the NIDCR-supported Center at the University of California, San Francisco. This trial demonstrated that as little as one fluoride varnish treatment a year, in addition to parental oral health counseling, can cut the cavity rate in half for young children at high risk for developing tooth decay19. The results of this study have contributed to policy changes at the state level: As of November 2008, 29 states reimburse physicians for fluoride varnish application to young children20.
Dissemination and implementation research are essential to assure that oral health advancements are appropriately and effectively translated to underserved and vulnerable populations. The NIDCR will support the development of new technologies that are culturally appropriate and affordable, and that can be delivered by workers readily available in communities.
The NIDCR also recognizes a critical need to consider research outcomes in their proper economic and societal contexts. Thus, the Institute will conduct systems-level research to assess the effectiveness of oral health interventions including vulnerable subgroups of the U.S. population. Comparative effectiveness studies will evaluate innovations and determine which represent added value, which offer minimal enhancements to current choices, which fail to reach their potential, and which work for some patients and not for others. The need to develop better evidence about the benefits, risks, and costs of alternative choices is imperative to practical and effective oral health care.
Objective IV-3: Provide science-based information about oral health and disease to health care providers, patients and caregivers, policy makers and the general public.
Many oral diseases and conditions can be prevented or controlled. However, due in part to the challenges of effecting behavioral change, significant gaps persist in oral health. The NIDCR ensures that the American public has access to science-based, unbiased, accessible information about oral health that people can use to make wise decisions about their oral health.
The NIDCR Office of Communications and Health Education produces and disseminates informational materials on a wide variety of topics, ranging from children’s oral health, oral cancer, and periodontal disease, to oral health care for people with disabilities. Some materials are geared toward patients or the general public; others are targeted to health care professionals, teachers or caregivers for special needs patients. The Institute also disseminates information about significant research advances to the media, patient support organizations, professional organizations and the research community. The Institute will continue to support vital communication efforts that can help translate scientific research into bettering people’s lives.
Objective IV-4: Monitor the oral health status of the nation, through periodic epidemiologic and other sentinel surveys.
Documenting the nation’s prevalence of the full range of oral, dental and craniofacial diseases is an important element of a strategic investment in basic and clinical research. The NIDCR uses this information to guide its planning efforts, as well as to assess the value of research investments. These tracking efforts are particularly important given the extent of co-morbidities that accompany oral diseases.
In partnership with the Centers for Disease Control and Prevention and other agencies, the NIDCR will seek and validate new methods to measure and document oral, dental, and craniofacial diseases, disorders and conditions; as well as risk factors and determinants of health disparities at the individual, community and societal levels. Companion to these activities will be an assessment of the social, educational, quality of life, and economic impact of problems related to oral, dental and craniofacial health.
As part of this effort, the NIDCR will enhance its in-house epidemiological expertise to enable a more thorough monitoring of changes in disease status, oral health determinants, access to care, and the use of professional, community and oral health services.
NIDCR at a Glance
Part of the National Institutes of Health, the NIDCR is the federal government’s lead agency for scientific research on oral, dental and craniofacial health and disease. Scientists supported by the NIDCR use modern biomedical research tools to conduct research on the full spectrum of topics related to craniofacial, oral and dental health and disease.
In efforts to improve the oral, dental and craniofacial health of the public, the NIDCR prioritizes scientific opportunities on the basis of their potential impact to improve health, the readiness of the scientific community to accomplish them and their alignment with our core values that are driven by science and protecting the public’s trust.
Figure 1. NIDCR FY 2008 Funding Distribution by Mechanism*
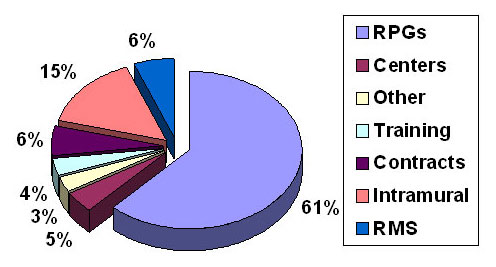
* RPG – Research Project Grants, RMS – Research Management and Support
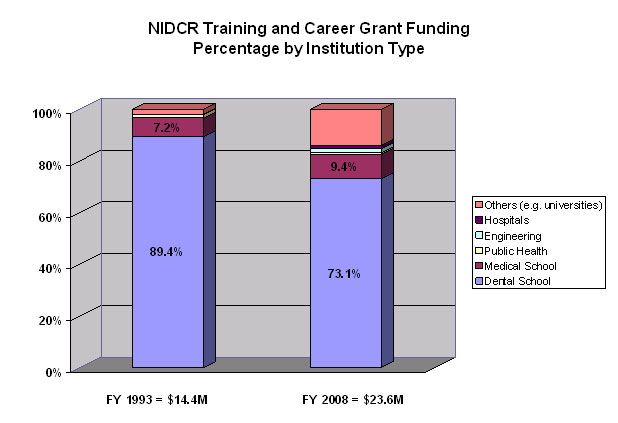
Figures 2 and 3 below show the trends in NIDCR support to academic institutions for extramural research and training/career development. The relative percentage of NIDCR extramural research and career and training funds awarded to schools of dentistry have steadily declined since 1993. Note that total expenditures for research ($262 million for FY 2008 and $99.1 million for FY 1993) are substantially larger than the total NIDCR training and career grant investment ($23.6 million and $14.4 million for FY 2008 and FY 1993, respectively).
Figure 2. Trends in NIDCR Extramural Grant Support to Academic Institutions
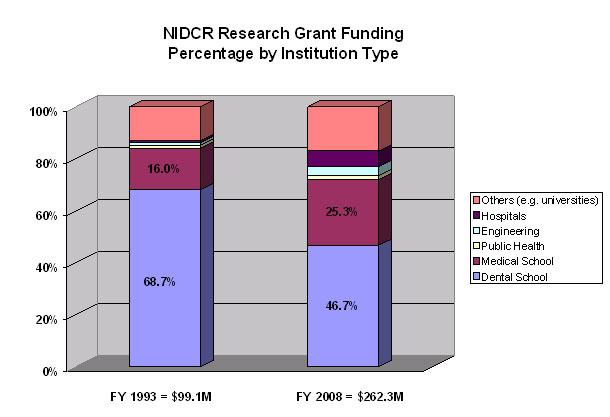
Figure 3. Trends in NIDCR Extramural Training and Career Development Support to Academic Institutions
Appendices
Appendix 1
NIDCR Planning and Priority Setting
In consultation with NIH leadership, the NIDCR engages in long- and short-term science planning to choose priorities for solicited extramural research. Planning activities are developed in consultation with a broad range of key external stakeholders. These include:
- the extramural scientific community;
- health voluntary organizations;
- the Congress;
- the Administration;
- the National Advisory Dental and Craniofacial Research Council and the NIDCR Board of Scientific Counselors;
- Other NIH Institutes and Centers, program offices and other federal agencies
- industry; and
- ad hoc advisory groups.
The Institute also relies on input from a range of conferences and workshops. These consultations review emerging scientific opportunities, identify public health concerns, and provide state-of-the-science assessments. Of course, as an NIH component, the NIDCR conducts its planning and priority setting within a larger context that considers input from the Congress, the Department of Health and Human Services, the NIH, and external peer review.
The initial phase of the 2009-2013 NIDCR strategic planning process focused in large part on securing public and stakeholder input regarding prospective activities, areas of research emphasis, future approaches to research sponsorship, needs, opportunities, and related issues. The input was gathered via five initiatives:
- An open forum listening session--augmented by informal conversations--at the American Association for Dental Research meeting in Dallas, Texas on April 2, 2008
- An open forum listening session held in conjunction with the NIDCR Patient Advocates Forum on the NIH campus on April 21, 2008
- Web-based responses from 140 individuals and organizations to six special strategic planning questions posted on the NIDCR website between May and July, 2008
- Two open forum listening sessions--augmented by informal conversations--at the International Association for Dental Research meeting in Toronto on July 2-3, 2008
- A series of NIDCR staff meetings to obtain input on NIDCR function and goals
The interpretation of these and other public perspectives is an important component of developing a workable, dynamic and responsive 2009-2013 NIDCR Strategic Plan.
Appendix 2
Oral Health: Past, Present, and Future
In June 1948, President Harry Truman signed Public Law 755 that created the then National Institute of Dental Research. This law created a national investment in oral health research to tackle the most pressing problem of the day: rampant decay and tooth loss.
Six decades later, in 2009, widespread fluoridation of our water supply still stands as a major public health breakthrough whose benefits have touched millions of Americans for generations. Other key advances made possible by NIDCR support include the seminal discovery that dental caries, or tooth decay, is an infectious disease, as is periodontal, or gum disease. This understanding has led to new practice strategies, such as routine use of dental sealants and fluoride varnishes as well as an understanding that treating gum disease during pregnancy is safe for both mother and baby.
The U.S. public has derived immeasurable benefits from these investments through improvements in dental health, but also in a wide array of health issues ranging from autoimmune disease to craniofacial birth defects to chronic orofacial pain to oral cancer.
What does the future hold for oral health? The investments we make today will create an exciting tomorrow for oral health prevention. Six decades from now, dentistry should be integrated into the primary health care network of the nation. Bioengineers will have succeeded in creating a lab-on-a chip that will be placed on a small orthodontic bracket within the mouth. This powerful device will enable real-time surveillance of hundreds of biomarkers to signal the earliest moments of disease—not just oral health conditions, but those affecting the rest of the body.
Dental drills will be a thing of the past. Specialized biomaterials such as rinses and biological implants will prevent biofilm formation on teeth, thus averting tooth decay and cavities. Standard equipment in dental offices will include imaging devices that can scan for and spot any unusual sores inside a patient’s mouth and even look for problems in other organs, through detection of sentinel molecules in saliva. Results from the human microbiome initiative will have led to predictive tools that seek and find the bacteria causing periodontal infections and the specific nature of the immune response, so personalized treatments can effectively target both.
Disfiguring birth defects and traumatic injuries from accidents, war, or other violence will be repairable either through the use of small molecules that activate developmental pathways in stem cells within the body or through the use of tissue-engineered replacements. New approaches to treating chronic pain will erase the lost productivity that used to be typical for chronic conditions like temporomandibular muscle and joint disorders.
Dry mouth caused by the destruction of salivary gland tissues by autoimmune disease or cancer will not occur, thanks to gene-transfer or small-molecule therapies. Head and neck cancers will be rare, due to effective prevention methods or tests that detect disease at the earliest moment of inception.
Appendix 3
The 21st-Century Mouth: A Window into Our Health
Why study the mouth? The term “oral cavity” belies the rich potential of this organ as a scientific playground and powerful tool for probing human health.
The oral cavity is an excellent model for studying complex systems. Home to a sophisticated set of functions, every second of every day the mouth exhibits a dynamic interplay between sensation, mechanical function and chemical flux. Multiple tissue types--including bone, nerves and blood--confront a bacterial zoo, crushing mechanical forces and electrical currents.
Microbial Laboratory. A healthy human mouth is home to an enormous variety of microorganisms, including viruses, fungi, protozoa and bacteria. The bacteria alone dominate this scene: Hundreds of millions live in a drop of saliva, accounting for about 1,500 different species in total. Research on this oral microbiome, which is likely to be unique to each individual, will offer the opportunity to look at a range of health issues including nutrition, infections and risk for cancer and other diseases.
Bone Remodeling. Bones of the head and face come in all shapes and sizes. They are subject to a wide range of mechanical loads and physical forces, rather unlike skeletal bones that are more linear in structure and function. Research on craniofacial bone structure and function offers the opportunity to convey lessons learned to more tailored rehabilitation of other bones in the body.
Joint Disorders and Pain. Temporomandibular muscle and joint disorder is a painful condition plaguing many people in the U.S.. But it is also a model system for understanding the complex interactions between sensation, mechanical forces, and tissue and immune function. Understanding temporomandibular muscle and joint disorder holds promise for understanding and treating other complex disorders such as chronic fatigue syndrome, fibromyalgia and chronic pain.
Drug Delivery. The salivary gland serves many functions: secreting proteins and hormones, and of course, keeping our mouth moist. But as a research tool, the salivary gland is a sophisticated bioreactor that may be used to deliver drugs, genes, proteins or other molecules to the bloodstream. It is also a valuable model for understanding basic glandular function—and thus can deepen understanding of how other glands and organs work—the pancreas, lungs, mammary glands and kidneys, for example.
Above all, the mouth is easy to get to—a uniquely tractable system and an excellent window into health and disease.
Appendix 4
Dentist-Scientist Tracks Craniofacial Development
Three quarters of all birth defects in humans disrupt the normal formation of a baby’s head and face. Such malformations have serious effects on quality of life and can impact disease risk, since the bones of the head protect the brain and most of our sensing mechanisms that detect the outside world, eat, breathe and talk.
Researchers know that one of the first steps in the early development of the head and face is the formation of a special set of cells called the cranial neural crest. As an embryo develops inside its mother, subsets of these neural crest cells receive molecular signals prompting them to form bone, cartilage, or teeth that then go on to form specific parts of the head and face.
Developmental biologist Yang Chai, D.D.S., Ph.D., of the University of Southern California in Los Angeles is creating cutting-edge molecular tools to track the fate of neural crest cells and determine which molecules push them to become particular tissue types.
For example, Chai has used genetically engineered mice to pinpoint the roles of certain growth factors critical for the proper formation of the teeth, jaw, and palate (roof of the mouth). By switching on or off the production of the genes that encode the growth factors, Chai has learned which ones are used by the neural crest cells to make specific craniofacial tissues. His research team is now working on how to manipulate the expression of these growth factors in an effort to fix cleft palate in living tissues.
Appendix 5
FDA-Approved Drug May Treat Head and Neck Cancer
As the sixth most common cancer in the developed world, squamous cell carcinoma of the head and neck affects about 45,000 people in the United States. Many of these tumors have disfiguring effects on the mouth and lips, and they can also disrupt a person’s ability to eat and swallow. Even more troubling, about half of the people diagnosed with this type of cancer die within five years, and this has not changed much in the past three decades.
J. Silvio Gutkind, Ph.D., chief of the Oral and Pharyngeal Cancer Branch, Cell Growth Regulation Section, and Molecular Carcinogenesis Section in NIDCR’s Intramural Research Program, has made major strides in combating this difficult disease. After learning that a particular molecular pathway is often revved up in head and neck cancer cells, Gutkind developed a mouse model system to study it further.
In this model, all of the mice develop mouth or tongue tumors after being exposed to a cancer-causing chemical that mimics the effects of tobacco exposure in people. (Smoking and spit tobacco use are main causes of head and neck cancer.)
Since Gutkind and his team already knew that the drug rapamycin could block this overactive molecular pathway, he tried giving it to the mice. Also called Rapamune®, rapamycin was approved by the Food and Drug Administration in 1999 for preventing kidney transplant rejection. Remarkably, not only did rapamycin shrink existing tumors in the mice, it also blocked new ones from forming21,22. The work points to a new, molecular-targeted approach for treating head and neck cancer.
Appendix 6
On a Mission: Improving Oral Health of Poor Youth
Tracy Finlayson, Ph.D., cares deeply about kids—in particular, their oral health. So much so that Finlayson has dedicated her career to the cause and in 2008, the American Public Health Association recognized Finlayson's efforts by awarding her the prestigious Jay S. Drotman Award for young professionals.
Finlayson first got interested in oral health disparities as a college student when she interned with the Head Start Bureau’s Health and Disabilities Branch in Washington, DC. It was summer 2000, and the Surgeon General’s Oral Health Report had just been released.
“I was included in many of the discussions about the challenges in access to care and worse oral health outcomes for many lower income and minority families,” Finlayson says, and the experience cemented her passion for addressing health disparities.
After college, Finlayson pursued her doctorate in health services organization and policy, from the University of Michigan School of Public Health. There, she studied how social and behavioral factors affecting low-income, African American mothers in Detroit affected the health of their young children.
Finlayson learned that if mothers brushed their teeth and felt more confident about being able to get their child's teeth brushed before bed, their children were also more likely to brush. She also found that a mother who felt confident--even when stressed, anxious or tired—could still have a significant impact on her child's health habits.
Although the findings may seem intuitive, Finlayson's work has prompted public health officials to use her results to fashion interventions to combat health disparities in children. Today, she continues to work tirelessly on improving the oral health of our youngest citizens.
Appendix 7
Research Leads Oral Health Scientist to the White House
In a rare opportunity for any researcher, in December 2008 Suchitra Nelson, Ph.D., made a trip from Ohio to the White House in Washington, DC. There, Nelson accepted a Presidential Early Career Award for Scientists and Engineers, an honor that recognizes outstanding young scientists advancing biomedical and behavioral research for the nation. Only about a dozen or so are named each year by the President of the United States.
Nelson is a dental epidemiologist. Her goal is to reduce oral health disparities in underprivileged populations. Very low birth-weight infants (under three and a half pounds) are at high risk for a range of health problems, including poor oral health. They are known to have defects in the protective enamel of baby teeth, for example.
She is conducting a clinical study to determine whether a very low birth weight puts kids at risk for tooth decay later in life. Nelson is gathering data on tooth development and decay; diet, oral hygiene and access to care; as well as demographic factors such as socioeconomic status. She will then compare these variables in normal birth weight infants to look for differences.
Understanding the link between health risk factors such as very low birth weight and poor oral health can point to prevention strategies for special needs children. Those strategies could have wide-ranging effects on improving oral health in poor communities across the country.
Appendix 8
Clinical Innovation for Better Oral Health
The NIDCR currently funds a broad array of clinical studies to improve oral, dental, and craniofacial health:
- Use of genetic analyses for prognosis and guided treatment of oral cancer
- Phase III trial to determine if treatment of periodontal disease improves glycemic control in type II diabetes
- Longitudinal study of young women to determine risk factors for the onset of temporomandibular disorder
- Community-based studies testing interventions to decrease the incidence and severity of early childhood caries in health disparities populations
- Determining the oral health of Hispanic populations enrolled in the Hispanic Community Health Study, conducted in four large U.S. cities
- Determination of the scope of HIV-related oral disease in the era of new generation HIV treatments
- Testing inexpensive topical therapies to manage oral candidiasis in resource-poor settings
- Studies evaluating the role of the autonomic nervous system in Sjögren’s syndrome
- Phase III trial to determine the optimal timing for primary surgery of infants born with cleft palate
Appendix 9
State-of-the-Art Transplant Center
The blood-forming tissue inside our bones may be a gold mine for 21st century oral health and beyond, thanks to innovative research from an NIDCR scientist.
A new clinical research facility just coming online aims to harvest bone marrow stromal cells (a type of “support” cells) and use them to nurse damaged tissues to begin the healing process. Pamela Robey, Ph.D., chief of NIDCR’s Craniofacial and Skeletal Diseases Branch in its Intramural Research Program, is leading a novel, trans-NIH project that will harness the healing power of the bone marrow stromal cells. These seemingly magical cells can be coaxed to become cartilage, bone, marrow, or fat.
The Bone Marrow Stromal Cell Transplantation Center is now establishing procedures to process donor marrow into clinical-grade human bone marrow stromal cells that can reconstruct bones of the head and face. The hope is that since bone marrow stromal cells are easily accessible, they may also find use for treating other conditions such as joint and connective tissue disorders. According to Robey, recent studies suggest that the cells are also useful for tamping down the immune system, which is necessary for treating autoimmune disease and other conditions.
Robey and her team continue to look for ways to grow large quantities of bone marrow stromal cells in a clinical setting. If such cells are going to be used to treat diseases in people and animals, it is vital that the cells are what the researchers think they are. That means finding surface markers or molecular bar codes to identify them precisely after growing them in culture.
It also means figuring out a way to get the cells to grow as they do during normal development, in a three-dimensional environment built from various different types of biomaterials. Currently only one such scaffold--hydroxyapatite–tricalcium phosphate ceramic particles--allows both bone and bone marrow to form. Robey is currently investigating how to tailor the size and shape of new scaffolds to support the growth and proper formation of cells and tissues.
Dozens of investigators, representing 13 NIH Institutes and Centers, have expressed interest in using bone marrow stromal cells for a range of purposes. The Center will operate out of the NIH Clinical Center Department of Transfusion Medicine to ready the cells for diverse clinical protocols. Robey will co-coordinate the project with Harvey G. Klein, M.D., Chief of the NIH Clinical Center Department of Transfusion Medicine.
Appendix 10
Real-World Research
In the United States today, more than 120 primary care practice-based research networks (PBRNs) actively research health issues in communities. These include approximately 20,000 practices of pediatrics, family medicine and general internal medicine, located in all 50 states, and providing care for more than 20 million of people in the U.S.
In 2005, the NIDCR established three regional practice-based research networks devoted to oral health care. Today, in 2009, over 600 practices are enrolled in the NIDCR PBRN program. Collectively, their mission is to create the infrastructure for practicing dentists and dental hygienists to conduct clinical studies on a variety of pressing clinical issues in oral health care. Each network involves community dentists and hygienists that practice in more than 15 states and three Scandinavian countries.
A particular strength of the networks is their ability to use flexible and adaptable common platforms for data collection, data sharing, and communication. Such interoperability provides real strength for communication within and between networks.
Examples of current studies include:
- Complete or Partial Removal of Deep Caries
- Outcomes of Endodontic Treatment and Restoration
- Randomized Controlled Trial of Pulp Capping Materials
- Analgesic Use and Effectiveness in Dental Practice
- Salivary Markers in Caries Risk (pilot stage)
Most PBRN members have a strong interest in restorative dentistry. To diversify the PBRN research portfolio and address a pressing public health issue, the NIDCR asked all three of the PBRNs to develop and participate in a large, trans-network, case-control study on risk factors associated with osteonecrosis of the jaw. This study has been completed and the data are being analyzed in preparation for publication in the scientific literature.
Appendix 11
Saliva Protein “Dictionary” Comes Online
For many decades, researchers have known that saliva is important for more than chewing, tasting, swallowing, and as the first step in digestion: A multitude of proteins and other molecules in saliva also play vital roles in protecting us from bacteria and viruses that can make us sick.
Now, scientists are well on their way to understanding how saliva contributes all of its healthy functions. In March 2008, an NIDCR-supported team of biologists, chemists, engineers, and computer scientists at five research institutions across the country recently mapped the salivary proteome, or “dictionary,” of proteins present in human saliva.
Representing saliva samples from two dozen women and men of various ethnic backgrounds, the saliva catalog contains over a thousand proteins. Over half of the proteins in saliva were also present in blood, and nearly one quarter were the same as those in tears. A database that provides scientists with the raw data from these projects is now available online.
The saliva catalog is an important first step towards being able to use saliva biomarkers to diagnose oral and systemic diseases. Salivary tests based on these biomarkers offer many advantages over blood tests that require a needle stick and can pose contamination risks from blood-borne diseases. However, much effort is still required to enrich and refine the catalog. To realize this goal, it is crucial that the research community actively participates in this effort. In the works is a collaborative, community-based Web portal that will enable scientists to add their own research data to the growing database; share results; curate the data; and discover new knowledge--further enhancing the value of the salivary proteome.
Saliva tests offer many advantages over blood tests that require a needle stick and can pose contamination risks from blood-borne diseases.
Appendix 12
Conquering Oral Health Disparities
Despite remarkable improvement in the Nation’s oral health over the years, not everyone in the U.S. has benefited equally. Oral, dental and craniofacial conditions remain among the most common health problems for low-income, disadvantaged, disabled and institutionalized individuals. Given the diversity of the U.S. population, it is unrealistic to anticipate easy, one-size-fits-all solutions. Approaches that are tailored and targeted to individual, community and societal/environmental-level factors are needed to achieve health equality.
The NIDCR-funded Centers for Research to Reduce Disparities in Oral Health have demonstrated the need to partner with communities throughout the research process in order to fully understand what factors contribute to dental disease in each community and develop appropriate intervention strategies. For example, one Center discovered that only 14 percent of the tooth decay found among children in the poorest sections of Detroit can be attributed to “classical” risk factors. A community’s cultural beliefs about preventive care, understanding of the importance of “baby” teeth, mistrust of drinking tap water, maternal health fatalism, fear of dental care and even the proximity to places of worship and grocery stores contributed to oral health risk. Creative interventions are needed to address these factors.
A primary goal of the NIDCR Oral Health Disparities Centers is to seek creative but practical approaches that are inexpensive, can be easily applied and are exportable to other underserved communities.
- The Boston University Center for Research to Evaluate and Eliminate Dental Disparities is developing interventions to prevent early childhood caries, or ECC, that are appropriate for public housing residents and lay health workers. They also are working on physician-delivered interventions targeted at the caregivers of very young children.
- The University of California, San Francisco Center to Address Disparities in Children's Oral Health is exploring the effectiveness of different public health settings to prevent ECC with fluoride varnish. Additional projects will investigate the preventive effects of other treatments to prevent caries among older children.
- The University of Colorado Center for Native Oral Health Research is developing a research and community practice infrastructure to prevent oral diseases in American Indians and Alaska Natives. Community health workers are a key aspect of the intervention strategies.
- The University of Florida Southeast Center for Research to Reduce Disparities in Oral Health aims to reduce disparities in cancer survival by promoting early detection of oral and pharyngeal cancer through a rural community-based intervention project focused on African Americans.
- The University of Washington Northwest/Alaska/Hawaii Center to Reduce Oral Health Disparities is conducting community-based behavioral research with low-income pregnant women to enhance use of public dental care services for themselves and their infants.
Appendix 13
NIDCR-produced Educational Resources on Oral Health
- Practical Oral Care for People With Developmental Disabilities
- This series gives an overview of physical, mental and behavioral challenges common in patients with autism, Down syndrome, cerebral palsy and intellectual disability and offer strategies for providing oral care.
- A Healthy Mouth for Your Baby
- This easy-to-read brochure is for parents with infants or toddlers. It highlights the importance of using fluoride to protect teeth, cleaning a baby's teeth, and preventing baby-bottle tooth decay.
- Are you at Risk for Oral Cancer? What African American Men Need to Know
- This brochure is part of an information kit that was developed through target-audience focus group studies. It contains easy-to-understand information about the importance of early detection.
- Seal Out Tooth Decay
- This brochure explains the science behind tooth sealants and explains the valuable preventive role of sealants.
Footnotes
1National Cancer Institute: A Snapshot of Head and Neck Cancers web site. Accessed December 8, 2008 at http://planning.cancer.gov/disease/Head_and_Neck-Snapshot.pdf
2Centers for Disease Control and Prevention, Oral Cancer: Deadly to Ignore. Accessed December 8, 2008 at http://www.cdc.gov/Oralhealth/publications/factsheets/oc_facts.htm
3Lane PM, Gilhuly T, Whitehead P, Zeng H, Poh CF, Ng S, Williams PM, Zhang L, Rosin MP, MacAulay CE. Simple device for the direct visualization of oral-cavity tissue fluorescence. J Biomed Opt. 2006;11:024006.
4Oral Health in America: A Report of the Surgeon General, May 2000. Accessed December 8, 2008 at http://www.surgeongeneral.gov/library/oralhealth/
5Multiple Principal Investigators. NIH Office of Extramural Research. Accessed December 23, 2008 at http://grants.nih.gov/grants/multi_pi/
6Vieira AR, McHenry TG, Daack-Hirsch S, Murray JC, Marazita ML. 2008. A genome wide linkage scan for cleft lip and palate and dental anomalies. Am J Med Genet Part A 2008;146A:1406-1413.
7Vieira AR, Marazita ML, Goldstein-McHenry T. Genome-wide scan finds suggestive caries loci. J Dent Res. 2008;87:435-9.
8The FaceBase Project: Functional Genomics of Craniofacial Development and Disease. Accessed December 17, 2008 at http://www.nidcr.nih.gov/GrantsAndFunding/See_Funding_Opportunities_Sorted_By/ ConceptClearance/CurrentCC/FaceBase.htm
9Demmer RT, Jacobs DR Jr, Desvarieux M. Periodontal disease and incident type 2 diabetes: results from the First National Health and Nutrition Examination Survey and its epidemiologic follow-up study. Diabetes Care. 2008;31:1373-9.
10Saremi A, Nelson RG, Tulloch-Reid M, Hanson RL, Sievers ML, Taylor GW, Shlossman M, Bennett PH, Genco R, Knowler WC. Periodontal disease and mortality in type 2 diabetes. Diabetes Care. 2005;28:27-32.
11Hu S, Arellano M, Boontheung P, Wang J, Zhou H, Jiang J, Elashoff D, Wei R, Loo JA, Wong DT. Salivary proteomics for oral cancer biomarker discovery. Clin Cancer Res. 2008;14:6246-52.
12The NIH Roadmap Human Microbiome Project web site. Accessed January 7, 2009 at http://nihroadmap.nih.gov/hmp/
13U.S. Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General--Executive Summary. Rockville, MD. 2000, p.2.
14yas MJ, Anusavice KJ, Frencken JE, Mount GJ. Minimal intervention dentistry--a review. FDI Commission Project 1-97. Int Dent J. 2000;50:1-12.
15NIH New Investigators Program, Pathway to Independence Award web site. Accessed December 23, 2008 at http://grants.nih.gov/grants/new_investigators/pathway_independence.htm
16National Center for Research Resources CTSA web. Accessed December 10, 2008 at http://www.ctsaweb.org/
17Denny P, Hagen FK, Hardt M, Liao L, et al. The proteomes of human parotid and submandibular/sublingual gland salivas collected as the ductal secretions. Proteome Res. 2008;7:1994-2006.
18NIGMS MSTP web site. Accessed January 15, 2009 at http://www.nigms.nih.gov/Training/InstPredoc/PredocOverview-MSTP.htm.
19Weintraub JA, Ramos-Gomez F, Jue B, Shain S, et al. Fluoride varnish efficacy in preventing early childhood caries. J Dent Res 2006;85:172-6.
20States with MEDICAID funding for physician oral health screening and fluoride varnish. American Academy of Pediatrics: Oral Health web site. Accessed January 6, 2009 at http://www.aap.org/commpeds/dochs/oralhealth/pdf/OH-Reimbursement-Chart.pdf
21Amornphimoltham A, Leelahavanichkul K, Molinolo AA, Patel V, Gutkind JS. Inhibition of mTOR by rapamycin causes the regression of carcinogen-induced skin tumor lesions. Clin. Cancer Res. 2008;14: 8094-101.
22Czerninski R, Amornphimoltham P, Patel V, Molinolo AA, and Gutkind JS. Targeting mTOR by rapamycin prevents tumor progression in an oral-specific chemical carcinogenesis model. Cancer Prevention Res. 2009; in press.