Printer-Friendly PDF version  (371KB)
(371KB)
PowerPoint version  (642KB)
(642KB)
Oral or pharyngeal cancer will be diagnosed in an estimated 35,000 Americans this year, and will cause approximately 7,500 deaths. On average, only 60 percent of those with the disease will survive more than 5 years.
 Back to Top
Back to Top
Early Detection Saves Lives
With early detection and timely treatment, deaths from oral cancer could be dramatically reduced.
The 5-year survival rate for those with localized disease at diagnosis is 82 percent compared with only 28 percent for those whose cancer has spread to other parts of the body.
Early detection of oral cancer is often possible. Tissue changes in the mouth that might signal the beginnings of cancer often can be seen and felt easily.
 Back to Top
Back to Top
Lesions that might signal oral cancer
Two lesions that could be precursors to cancer are leukoplakia (white lesions) and erythroplakia (red lesions). Although less common than leukoplakia, erythroplakia and lesions with erythroplakic components have a much greater potential for becoming cancerous. Any white or red lesion that does not resolve itself in 2 weeks should be reevaluated and considered for biopsy to obtain a definitive diagnosis.
Other Possible Signs and Symptoms:
Possible signs and symptoms of oral cancer that your patients may report include: a lump or thickening in the oral soft tissues, soreness or a feeling that something is caught in the throat, difficulty chewing or swallowing, ear pain, difficulty moving the jaw or tongue, hoarseness, numbness of the tongue or other areas of the mouth, or swelling of the jaw that causes dentures to fit poorly or become uncomfortable.
If these problems persist for more than 2 weeks, a thorough clinical examination and laboratory tests, as necessary, should be performed to obtain a definitive diagnosis. If a diagnosis cannot be obtained, referral to the appropriate specialist is indicated.
 Back to Top
Back to Top
Tobacco/Alcohol Use
Tobacco and excessive alcohol use increases the risk of oral cancer. Using both tobacco and alcohol poses a much greater risk than using either substance alone.
Sunlight
Exposure to sunlight is a risk factor for lip cancer.
Age
Oral cancer is typically a disease of older people, usually because of their longer exposure to risk factors. Incidence of oral cancer rises steadily with age, reaching a peak in persons aged 55-64.
Gender
Oral cancer strikes men more than twice as often as it does women.
 Back to Top
Back to Top
A thorough head and neck examination should be a routine part of each patient's dental visit and general medical examination. Clinicians should be particularly vigilant in checking those who use tobacco or excessive amounts of alcohol.
- Examine your patients using the head and neck exam illustrated in this program.
- Take a history of their alcohol and tobacco use.
- Inform your patients of the association between tobacco use, alcohol use, and oral cancer.
- Follow-up to make sure a definitive diagnosis is obtained on any possible signs or symptoms of oral cancer.
 Back to Top
Back to Top
This exam is abstracted from the standardized oral examination method recommended by the World Health Organization. The method is consistent with those followed by the Centers for Disease Control and Prevention and the National Institutes of Health. It requires adequate lighting, a dental mouth mirror, two 2" x 2" gauze squares, and gloves; it should take no longer than 5 minutes.

Figure 1 - Face

Figure 2 - Lips

Figure 3 - Labial mucosa

Figure 4 - Labial mucosa

Figure 5 - Right buccal mucosa

Figure 6 - Left Buccal mucosa

Figure 7 - Gingiva

Figure 8 - Tongue dorsum

Figure 9 - Tongue left margin

Figure 10 - Tongue right margin
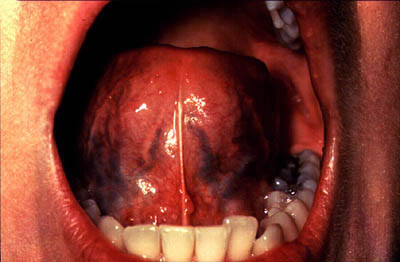
Figure 11 - Tongue ventral

Figure 12 - Floor

Figure 13 - Hard palate

Figure 14 - Oropharynx

Figure 15 - Palpation
 Back to Top
Back to Top
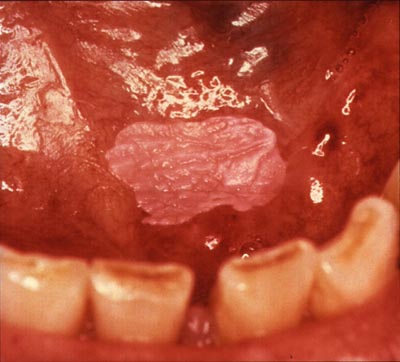
Homogenous leukoplakia in the floor of the mouth in a smoker. Biopsy showed hyperkeratosis.

Clinically, a leukoplakia on left buccal mucosa. However, the biopsy showed early squamous cell carcinoma. The lesion is suspicious because of the presence of nodules.

Nodular leukoplakia in right commissure. Biopsy showed severe epithelial dysplasia.

Erythroleukoplakia in left commissure and buccal mucosa. Biopsy showed mild epithelial dysplasia and presence of candida infection. A 2-3 week course of anti-fungal treatment may turn this type of lesion into a homogenous leukoplakia.
 Back to Top
Back to Top
The examination is conducted with the patient seated. Any intraoral prostheses are removed before starting. The extraoral and perioral tissues are examined first, followed by the intraoral tissues.
I. The Extraoral Examination
- FACE: (Figure 1) The extraoral assessment includes inspection of the face, head, and neck. The face, ears, and neck are observed, noting any asymmetry or changes on the skin such as crusts, fissuring, growths, and/or color change. The regional lymph node areas are bilaterally palpated to detect any enlarged nodes. If enlargement is detected, the examiner should determine the mobility and consistency of the nodes. A recommended order of examination includes the preauricular, submandibular, anterior cervical, posterior auricular, and posterior cervical regions.
II. Perioral and Intraoral Soft Tissue Examination
The perioral and intraoral examination procedure follows a seven-step systematic assessment of the lips; labial mucosa and sulcus; commissures, buccal mucosa, and sulcus; gingiva and alveolar ridge; tongue; floor of the mouth; and hard and soft palate.
- LIPS: (Figure 2) Begin examination by observing the lips with the patient's mouth both closed and open. Note the color, texture and any surface abnormalities of the upper and lower vermilion borders.
- LABIAL MUCOSA: (Figures 3 and 4) With the patient's mouth partially open, visually examine the labial mucosa and sulcus of the maxillary vestibule and frenum and the mandibular vestibule. Observe the color, texture, and any swelling or other abnormalities of the vestibular mucosa and gingiva.
- BUCCAL MUCOSA: (Figures 5 and 6) Retract the buccal mucosa. Examine first the right then the left buccal mucosa extending from the labial commissure and back to the anterior tonsillar pillar. Note any change in pigmentation, color, texture, mobility, and other abnormalities of the mucosa, making sure that the commissures are examined carefully and are not covered by the retractors during the retraction of the cheek.
- GINGIVA: (Figure 7) First, examine the buccal and labial aspects of the gingiva and alveolar ridges (processes) by starting with the right maxillary posterior gingiva and alveolar ridge and then move around the arch to the left posterior area. Drop to the left mandibular posterior gingiva and alveolar ridge and move around the arch to the right posterior area.
Second, examine the palatal and lingual aspects as had been done on the facial side, from right to left on the palatal (maxilla) and left to right on the lingual (mandible).
- TONGUE: (Figure 8) With the patient's tongue at rest, and mouth partially open, inspect the dorsum of the tongue for any swelling, ulceration, coating, or variation in size, color, or texture. Also note any change in the pattern of the papillae covering the surface of the tongue and examine the tip of the tongue. The patient should then protrude the tongue, and the examiner should note any abnormality of mobility or positioning.
(Figure 9) With the aid of mouth mirrors, inspect the right and left lateral margins of the tongue.
(Figure 10) Grasping the tip of the tongue with a piece of gauze will assist full protrusion and will aid examination of the more posterior aspects of the tongue's lateral borders
(Figure 11) Then examine the ventral surface. Palpate the tongue to detect growths.
- FLOOR: (Figure 12) With the tongue still elevated, inspect the floor of the mouth for changes in color, texture, swellings, or other surface abnormalities.
- PALATE: (Figures 13 and 14) With the mouth wide open and the patient's head tilted back, gently depress the base of the tongue with a mouth mirror. First inspect the hard and then the soft palate.
(Figure 14) Examine all soft palate and oropharyngeal tissues.
(Figure 15) Bimanually palpate the floor of the mouth for any abnormalities. All mucosal or facial tissues that seem to be abnormal should be palpated.
 Back to Top
Back to Top
 This information is not copyrighted. Print and make as many photocopies as you need.
This information is not copyrighted. Print and make as many photocopies as you need.
"Detecting Oral Cancer: A Guide for Health Care Professionals" is also available as a poster. Order a free copy.
NOTE: PDF documents require the free Adobe Reader.