What Is Heart Failure?
Heart failure is a condition in which the heart
can’t pump blood the way it should. In some cases, the heart can’t
fill with enough blood. In other cases, the heart can’t send blood to the
rest of the body with enough force. Some people have both problems.
“Heart failure” doesn’t mean that
your heart has stopped or is about to stop working. However, it’s a
serious condition that requires medical care.
Overview
Heart failure develops over time as the pumping of
the heart grows weaker. It can affect the right side of the heart only or both
the left and right sides of the heart. Most cases involve both sides of the
heart.
Right-side heart failure occurs when the heart
can’t pump blood to the lungs, where it picks up oxygen. Left-side heart
failure occurs when the heart can’t pump enough oxygen-rich blood to the
rest of the body.
Right-side heart failure may cause fluid to build up
in the feet, ankles, legs, liver, abdomen, and, rarely, the veins in the neck.
Right-side and left-side heart failure also cause shortness of breath and
fatigue (tiredness).
The leading causes of heart failure are diseases
that damage the heart. These include
coronary
artery disease (CAD),
high
blood pressure, and
diabetes.
Outlook
Heart failure is a very common condition. About 5
million people in the United States have heart failure, and it results in about
300,000 deaths each year.
Both children and adults can have heart failure,
although the symptoms and treatments differ. This article focuses on heart
failure in adults.
Taking steps to prevent CAD can help prevent heart
failure. These steps include following a heart healthy diet, not smoking, doing
physical activity, and losing weight if you’re
overweight
or obese. Working with your doctor to control high blood pressure and
diabetes also can help prevent heart failure.
People who have heart failure can live longer and
more active lives if it’s diagnosed early and they follow their treatment
plans. For most, treatment includes medicines and lifestyle measures.
Currently, there’s no cure for heart failure.
However, researchers are finding and testing new treatments. These treatments
offer hope for better ways to delay heart failure and its complications.
Other Names for Heart Failure
- Dropsy.
- Left-side, or systolic, heart failure. This is
when the heart can't pump enough oxygen-rich blood to the body.
- Right-side, or diastolic, heart failure. This is
when the heart can't fill with enough blood.
Some people have only right-side heart failure. But
all people who have left-side heart failure also have right-side heart failure.
Treatments for right-side heart failure alone differ from treatments for both
right-side and left-side heart failure. Your doctor will plan your treatment
based on your type of heart failure and your unique needs.
What Causes Heart Failure?
Conditions that damage the heart muscle or make it
work too hard can cause heart failure. Over time, the heart weakens. It isn't
able to fill with and/or pump blood as well as it should.
As the heart weakens, certain proteins and other
substances may be released into the blood. They have a toxic effect on the
heart and blood flow, and they cause heart failure to worsen.
Major Causes
The most common causes of heart failure are
coronary
artery disease (CAD),
high
blood pressure, and
diabetes. Treating these problems can prevent or improve heart
failure.
Coronary Artery Disease
CAD occurs when a fatty material called plaque
(plak) builds up in your coronary arteries. These arteries supply oxygen-rich
blood to your heart. Plaque narrows the arteries, causing less blood to flow to
your heart muscle. This can lead to chest pain,
heart attack, and heart damage.
High Blood Pressure
Blood pressure is the force of blood pushing against
the walls of the arteries. Blood pressure is “high” if it stays at
or above 140/90 mmHg over a period of time. High blood pressure stiffens blood
vessels and makes the heart work harder. Without treatment, the heart may be
damaged.
Diabetes
This disease occurs when the level of sugar in the
blood is high. The body doesn't make enough insulin or doesn't use its insulin
properly. Insulin is a hormone that helps convert food to energy. High sugar
levels can damage blood vessels around the heart.
Other Causes
Other diseases and conditions that can lead to heart
failure are:
- Heart
muscle diseases. These diseases may be present at birth or due to injury or
infection.
- Heart valve disorders. These problems may be
present at birth or due to infections, heart attacks, or damage from heart
disease.
- Arrhythmias
(ah-RITH-me-ahs), or irregular heartbeats. These heart problems may be present
at birth or due to heart disease or heart defects.
- Congenital
heart defects. These heart problems are present at birth.
Other factors also can injure the heart muscle and
lead to heart failure. These include:
- Treatments for cancer, such as radiation and
chemotherapy
- Thyroid disorders (having either too much or too
little thyroid hormone in the body)
- Alcohol abuse
- HIV/AIDS
- Cocaine and other illegal drug use
- Too much vitamin E
Heart damage from
obstructive
sleep apnea may cause heart failure to worsen. In obstructive sleep apnea,
your breathing stops or gets very shallow while you’re sleeping. This can
deprive the heart of oxygen and increase its workload. Treating this sleep
problem may improve heart failure.
Who Is At Risk for Heart Failure?
About 5 million people in the United States have
heart failure, and it results in about 300,000 deaths each year. The number of
people who have heart failure is growing. Each year, another 550,000 people are
diagnosed for the first time. Heart failure is more common in:
- People who are 65 or older. Aging can weaken the
heart muscle. Older people also may have had a disease for many years that
causes heart failure. Heart failure is the #1 reason for hospital visits in
this age group.
- African Americans. African Americans are more
likely than people of other races to have heart failure and to suffer from more
severe forms of it. They’re also more likely than other groups to have
symptoms at a younger age, get worse faster, have more hospital visits due to
heart failure, and die from heart failure.
- People who are
overweight
or obese. Excess weight puts a greater strain on the heart. It also can
lead to type II
diabetes, which adds to the risk of heart failure.
Men have a higher rate of heart failure than women.
But in actual numbers, more women have the condition. This is because many more
women than men live into their seventies and eighties when it’s common.
Children with
congenital
heart defects also can develop heart failure. Children are born with these
defects when the heart, heart valves, and/or blood vessels near the heart
don’t form correctly. This can weaken the heart muscle and lead to heart
failure.
Children don’t have the same symptoms or get
the same treatment for heart failure as adults. This article focuses on heart
failure in adults.
What Are the Signs and Symptoms of Heart
Failure?
The most common signs and symptoms of heart failure
are:
- Shortness of breath or trouble breathing
- Fatigue (tiredness)
- Swelling in the ankles, feet, legs, abdomen, and,
rarely, the veins in your neck
All of these symptoms are due to the buildup of
fluid in your body. When symptoms start, you may feel tired and short of breath
after routine physical effort—like climbing stairs.
As the heart grows weaker, symptoms get worse. You
may begin to feel tired and short of breath after getting dressed or walking
across the room. Some people have shortness of breath while lying flat.
Fluid buildup from heart failure also causes weight
gain, frequent urination, and a cough that's worse at night and when you're
lying down. This cough may be a sign of a condition called acute pulmonary
(PULL-mun-ary) edema (e-DE-ma). This is when too much fluid is in your lungs.
This severe condition requires emergency treatment.
Heart Failure Signs and
Symptoms
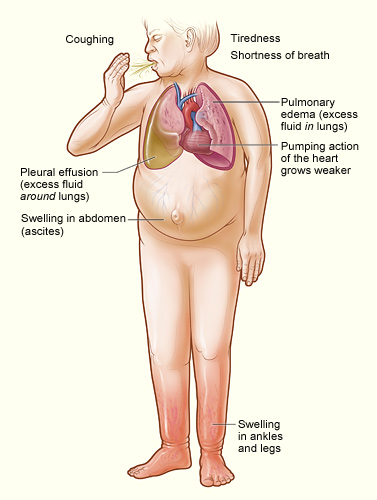
The illustration shows the major
signs and symptoms of heart failure.
How Is Heart Failure Diagnosed?
Your doctor will diagnose heart failure based on
your medical and family histories, a physical exam, and tests. Because the
symptoms of heart failure also are common in other conditions, your doctor
must:
- Find out whether you have a disease or condition
that can cause heart failure, such as
coronary
artery disease (CAD),
high
blood pressure, or
diabetes
- Rule out other causes of your symptoms
- Find any damage to your heart and measure how
well your heart pumps blood
Early diagnosis and treatment can help people with
heart failure live longer, more active lives.
Medical and Family Histories
Your doctor will ask whether you or others in your
family have or have had a disease or condition that can cause heart failure.
Your doctor also will ask about your symptoms. He or
she will want to know which symptoms you've have, when they occur, how long
you've had them, and how severe they are. The answers will help show whether
and how much your symptoms limit your daily routine.
Physical Exam
During the physical exam, your doctor will:
- Listen to your heart for sounds that aren't
normal
- Listen to your lungs for the sounds of extra
fluid buildup
- Look for swelling in your ankles, feet, legs,
abdomen, and the veins in your neck
Diagnostic Tests
No one test shows whether you have heart failure. If
you have signs and symptoms of heart failure, your doctor may order an
EKG
(electrocardiogram), a chest x ray, and a BNP blood test as initial tests.
Initial Tests
EKG. This simple test shows how
fast your heart is beating and whether its rhythm is steady or irregular. An
EKG may show whether you have had a
heart
attack or whether the walls in your heart's pumping chambers are thicker
than normal. Thicker walls can make it harder for your heart to pump blood.
Chest x ray. A chest x ray takes a
picture of your heart and lungs. It can show whether your heart is enlarged,
whether you have fluid in your lungs, or whether you have lung disease.
BNP blood test. This new test
checks the level of a hormone called BNP, which rises during heart failure.
Followup Tests
Your doctor may refer you to a cardiologist if your
initial test results indicate heart failure. A cardiologist is a doctor who
specializes in treating people with heart problems.
The cardiologist will likely order one or more other
tests to confirm the diagnosis.
Echocardiography. Echocardiography
uses sound waves to create a moving picture of your heart. It shows the size
and shape of your heart and how well parts of your heart are working. The test
also can show where blood flows poorly to the heart, where the heart muscle
doesn't contract as it should, and damage to the heart muscle caused by poor
blood flow.
Sometimes this test is done both before and after
your heart is put through physical stress (see stress testing below). Testing
under stress helps show whether there's a lack of blood flow to your heart (a
sign of CAD).
Doppler imaging. A Doppler test
uses sound waves to measure the speed and direction of blood flow. It's often
done with an echocardiogram to give a more complete picture of blood flow to
the heart and lungs.
Doppler is often used to find out whether you have
right-side heart failure (this is when the heart can't fill with enough blood).
Holter monitor. A Holter monitor
is a small box that you carry in a pouch around your neck or clipped to your
belt. It's attached to sticky patches called electrodes that are placed on your
chest. The device records your heart rhythm for a full 24- or 48-hour period,
while you do your normal daily activities.
Nuclear heart scan. A
nuclear
heart scan is a test that shows how well blood is passing through your
heart and how much blood is reaching your heart muscle.
Your doctor will inject a radioactive substance into
your bloodstream, which will make your heart chambers and vessels easy to see.
Then, a special camera is used to show where the substance lights up (in
healthy heart muscle) and where it doesn't (in damaged heart muscle).
Your doctor may want to do this test while your
heart is under physical stress (see stress testing below).
Cardiac catheterization. During
cardiac
catheterization (KATH-e-ter-i-ZA-shun), a long, thin, flexible tube called
a catheter is put into a blood vessel in your arm, groin (upper thigh), or neck
and threaded to your heart. This allows your doctor to study the insides of
your coronary arteries. Coronary arteries carry oxygen-rich blood to your
heart.
During this procedure, your doctor can check the
pressure and blood flow in the heart's chambers, collect blood samples, and use
x rays to look at the coronary arteries.
Coronary angiography.
Coronary
angiography (an-jee-OG-ra-fee) is usually done with cardiac
catheterization. A dye that can be seen on x ray is injected into the blood
through the tip of the catheter. The dye allows your doctor to see the flow of
blood to the heart muscle. This test also shows how well your heart is pumping.
Stress test. Some heart problems
are easier to diagnose when your heart is working harder and beating faster
than when it's at rest. During
stress
testing, you exercise (or are given medicine if you can't exercise) to make
your heart work harder and beat faster. You may walk or run on a treadmill or
pedal a bicycle.
Heart tests, such as nuclear heart scanning and
echocardiography, are done during stress testing.
Cardiac magnetic resonance imaging
(MRI). A
cardiac
MRI scan shows, in detail, the structures and beating of your heart. An MRI
scan can help your doctor see whether parts of your heart are damaged. Doctors
also are using MRI in research studies to find early signs of heart failure,
even before symptoms appear.
Positron emission tomography (PET).
PET scanning shows the level of chemical activity in areas of your heart. This
scan can help your doctor see whether enough blood is flowing to these areas.
It can show blood flow problems that other types of scans may not pick up.
Thyroid function tests. Thyroid
function tests show how well the thyroid is working. They include blood tests,
imaging tests, and tests to stimulate the thyroid. These common tests are key
in checking for heart failure. Having too much or too little thyroid hormone in
the blood can cause heart failure.
How Is Heart Failure Treated?
Early diagnosis and treatment can help people with
heart failure live longer, more active lives. How heart failure is treated will
depend on your type and stage of heart failure (how severe it is).
The goals of treatment for all stages of heart
failure are to:
For people with any stage of heart failure,
treatment will include lifestyle measures, medicines, and ongoing care. People
who have more severe heart failure also may need medical procedures and
surgery.
Lifestyle Measures
You can take simple steps to help yourself feel
better and control heart failure. The sooner you start these measures, the
better off you're likely to be.
Follow a Healthy Eating Plan
A diet low in salt, fat, saturated fat,
trans fat, and cholesterol can help you prevent or control heart
failure. Salt can cause extra fluid to build up in your body, making heart
failure worse. Fat and saturated fat can increase your blood cholesterol
levels. Trans fat raises your LDL ("bad") cholesterol and lowers your
HDL ("good") cholesterol. High blood cholesterol can cause heart disease, which
in turn can cause heart failure.
A balanced diet with varied nutrients can help your
heart work better. Getting enough potassium is key for people with heart
failure. Some heart failure medicines deplete the potassium in your body. This
can put people with heart failure in danger. Lack of potassium can cause very
rapid heart rhythms that lead to sudden death.
Potassium is found in foods like bananas,
strawberries, raisins, beets, and greens. Talk to your health care team about
getting the correct amount of potassium.
If you have heart failure, you shouldn't drink
alcohol. If you have severe heart failure, your doctor may advise you to limit
the amount of fluids that you drink.
Examples of healthy eating plans are the National
Heart, Lung, and Blood Institute's
Therapeutic
Lifestyle Changes (TLC) diet and the
Dietary
Approaches to Stop Hypertension (DASH) eating plan.
The TLC diet is low in saturated fat and
cholesterol to help lower blood cholesterol. The DASH eating plan contains less
salt/sodium, sweets, added sugars, fats, and red meat than the typical American
diet. Fruits, vegetables, fat-free or low-fat diary products, whole grains,
fish, poultry, beans, seeds, and nuts are the focus of the plan.
Adopt Healthy Habits
Taking steps to control risk factors for CAD, high
blood pressure, and diabetes also will help control heart failure.
- Lose weight if you're
overweight
or obese. Work with your health care team to lose weight safely.
- Do physical activity as your doctor directs to
become more fit and stay as active as possible.
- Quit smoking and avoid using illegal drugs. Avoid
exposure to secondhand smoke. Smoking and drugs can worsen heart failure and
harm your health.
- Get enough rest.
Medicines
Your doctor will base your medicine treatment on the
type of heart failure you have, how severe it is, and your response to certain
medicines. The following are the main medicines for treating heart failure.
- Diuretics (water or fluid pills) help reduce
fluid buildup in your lungs and swelling in your feet and ankles.
- ACE inhibitors lower blood pressure and reduce
strain on your heart. They also may reduce the risk of a future
heart
attack.
- Aldosterone antagonists trigger the body to get
rid of salt and water through urine, which lowers the volume of blood that the
heart must pump.
- Angiotensin receptor blockers relax your blood
vessels and lower blood pressure, so the heart doesn't have to work as hard.
- Beta blockers slow your heart rate and lower your
blood pressure to decrease the workload on your heart.
- Isosorbide dinitrate/hydralazine hydrochloride
helps relax your blood vessels, so your heart doesn't work as hard to pump
blood. The Food and Drug Administration approved this medicine for use in
African Americans after studies showed it worked well for this group.
- Digoxin makes the heart beat stronger and pump
more blood.
Many people with severe heart failure must be
treated in the hospital from time to time. In the hospital, you may receive new
or special medicines, but you will keep taking your other medicines too. Some
people with very severe heart failure are given intravenous (IV) medicines,
which are injected into veins in their arms.
Your doctor also will order extra oxygen if you take
medicine but still have trouble breathing. The extra oxygen can be given in the
hospital and at home.
Ongoing Care
It's important to watch for signs that heart failure
is getting worse. Weigh yourself each day. Let your doctor know right away if
you have a sudden weight gain or weight loss. Either one can signal a need to
adjust your treatment. If your doctor advises you to limit your intake of
fluids, carefully watch how much you drink during the day.
It's also important to get medical care for other
related conditions. If you have diabetes and/or high blood pressure, work with
your health care team to control your condition(s). Have your blood sugar level
and blood pressure checked. Your doctor will tell you how often to come in for
tests and how often to take measurements at home.
Medical Procedures and Surgery
As heart failure worsens, lifestyle changes and
medicines may no longer control heart failure symptoms. You may need a medical
procedure or surgery.
If you have heart damage and severe heart failure
symptoms, you may need:
- Cardiac resynchronization therapy. In heart
failure, the right and left sides of the heart may no longer contract at the
same time. This disrupts the heart's pumping. To correct this problem, doctors
may implant a type of
pacemaker
near your heart. This device helps both sides of the heart contract at the same
time, which may decrease heart failure symptoms.
- An
implantable
cardioverter defibrillator (ICD). Some people with heart failure have very
rapid, irregular heartbeats. Without treatment, the problem can cause
sudden
cardiac arrest. Doctors implant ICDs to solve this problem. ICDs are
similar to pacemakers. The device checks your heart rate and corrects heart
rhythms that are too fast.
People who have heart failure symptoms at rest
despite other treatments may need:
- A mechanical heart pump, such as a left
ventricular assist device. This device helps pump blood from the heart to the
rest of the body. People may use pumps until they have surgery or as a
long-term treatment.
- Heart
transplant. When all other treatments fail to control symptoms, some people
who have heart failure receive healthy hearts from deceased donors.
- Experimental treatments. Studies are under way
to see whether
open-heart
surgery or
angioplasty
(a procedure used to unblock heart arteries and improve blood flow) can reduce
heart failure symptoms.
Ongoing Research
Researchers continue to learn more about heart
failure and how to treat it. As a result, treatments are getting better.
People with heart failure often can be treated in a
research study. You get top care from heart failure experts and the chance to
help advance heart failure knowledge and care.
You also may want to take part in a heart failure
registry, which tracks the course of disease and treatment in large numbers of
people. These data help research move forward. You may help yourself and others
by taking part. Talk to your health care team to learn more.
How Can Heart Failure Be Prevented?
You can take steps to prevent heart failure. The
sooner you start, the better your chances to avoid it or to stay healthier
longer.
For People Who Have Healthy Hearts
If you have a healthy heart, you can take action to
prevent heart disease, which helps prevent heart failure. To prevent heart
disease:
- Follow a heart healthy diet that focuses on
fruits, vegetables, whole grains, low-fat diary products, and lean meat. It
also should be low in salt, fat, saturated fat, trans fat, and
cholesterol. Examples of healthy eating plans are the National Heart, Lung, and
Blood Institute's
Therapeutic
Lifestyle Changes (TLC) diet and the
Dietary
Approaches to Stop Hypertension (DASH) eating plan.
- Quit smoking if you smoke. Avoid exposure to
secondhand smoke.
- Lose weight if you're
overweight
or obese.
- Get regular physical activity. Aim for at least
30 minutes on most, and preferably all, days of the week.
- Avoid using illegal drugs.
For People Who Are at High Risk for Heart Failure
Even if you're at high risk for heart failure, you
can take steps to reduce your risks. People at high risk include those who have
high
blood pressure,
coronary
artery disease, or
diabetes, or people who are obese.
- Follow all of the steps listed above.
- Treat and control any conditions that cause heart
failure. Take medicines as your doctor prescribes.
- Avoid drinking alcohol.
- See your doctor for regular followup visits.
For People Who Have Heart Damage but No Signs of
Heart Failure
If you have heart damage but no signs of heart
failure, you can still reduce your risks. In addition to taking the steps
above, take all of the medicines your doctor prescribes to reduce your heart's
workload.
If you have side effects from a medicine, tell your
doctor. You should never stop taking medicine without asking your doctor first.
Living With Heart Failure
Heart failure can't be cured. You will likely have
to take medicine and follow a treatment plan for the rest of your life.
Despite treatment, symptoms may get worse over time.
You may not be able to do many of the things that you did before you had heart
failure. However, if you take all the steps your doctor recommends, you can
stay healthier longer.
Researchers also may find new treatments that can
help you in the future.
Follow Your Treatment Plan
Treatment can relieve your symptoms and make daily
activities easier. It also can reduce the chance that you'll have to go to the
hospital. For these reasons, it's vital that you follow your treatment plan.
- Take all of your medicines as your doctor
prescribes. If you have side effects from a medicine, tell your doctor. You
should never stop taking medicine without asking your doctor first.
- Make all of the lifestyle changes that your
doctor recommends.
- Get advice from your doctor about how active you
can/should be. This includes advice on daily activities, work, leisure time,
sex, and exercise. Your level of activity will depend on the stage of your
heart failure (how severe it is). Studies show that aerobic exercise improves
heart function; other types of exercise don't.
- Keep all of your medical appointments, including
visits to the doctor and appointments to get tests and lab work. Your doctor
needs the results of these tests to adjust your medicine doses and help you
avoid any harmful side effects.
Take Steps To Prevent Heart Failure From Getting
Worse
Certain factors can cause your heart failure to
worsen. These include:
- Forgetting to take your medicines
- Not following your diet (such as eating salty
foods)
- Drinking alcohol
These factors can lead to a hospital stay. If you
have trouble following your diet, talk to your doctor. Your doctor can help
arrange for a dietitian to work with you. Avoid drinking alcohol.
People with heart failure often have other serious
conditions that require ongoing treatment. If you do, you're likely taking
medicines for them as well as for heart failure. Taking more than one medicine
raises the risk of side effects and other problems. Make sure your pharmacist
has a complete list of all of the medicines and over-the-counter products that
you're taking.
Tell your doctor right away about any problems with
your medicines. Also, talk with your doctor before taking any new medicine
another doctor prescribes or any new over-the-counter medicines or herbal
supplements.
Try to avoid respiratory infections like the flu and
pneumonia. Ask your doctor or nurse about getting flu and pneumonia vaccines.
Coping with heart failure and changing your life to
decrease symptoms can be hard. You may feel depressed. If so, talk to your
doctor. He or she may recommend treatment for depression. This treatment can
improve your outlook and help you enjoy life more.
Plan Ahead
Be ready to meet your health needs. Know:
- When to seek help. Talk to your doctor about when
to make an office visit or when to get urgent help.
- Phone numbers for your doctor and hospital.
- Directions to the doctor's office or hospital and
people who can take you there.
- A list of medicines you're taking.
Key Points
- Heart failure is a condition in which your heart
can't pump blood the way it should. In some cases, the heart can't fill with
enough blood. In other cases, the heart can't send blood to the rest of the
body with enough force. Some people have both problems.
- "Heart failure" doesn't mean that your heart has
stopped or is about to stop working. However, it's a serious condition that
requires medical care.
- The leading causes of heart failure are diseases
that damage the heart. These include
coronary
artery disease,
high
blood pressure, and
diabetes. Heart failure develops over time as the pumping
action of the heart grows weaker.
- Heart failure is a common condition. About 5
million people in the United States have heart failure, and it results in about
300,000 deaths each year. Heart failure is more common in people who are 65 or
older, African American, or
overweight
or obese. Men have a higher rate of heart failure than women.
- Common signs and symptoms of heart failure are
shortness of breath or trouble breathing, fatigue (feeling tired), and swelling
in the ankles, feet, legs, abdomen, and, rarely, the veins in the neck. All of
these symptoms are due to fluid buildup in your body.
- Your doctor will diagnose heart failure based on
your medical and family histories, a physical exam, and tests. He or she must
rule out other causes for symptoms and find out whether you have a disease or
condition that's causing heart failure. He or she also will check whether your
heart is damaged and how well it pumps blood.
- Heart failure treatment may include lifestyle
measures, medicines, ongoing care, and using a medical device or having
surgery. The sooner you start treatment, the better off you're likely to be.
- You can take steps to prevent heart failure by
having a healthy lifestyle, preventing and treating conditions that can lead to
heart failure, and taking medicines as your doctor prescribes.
- Heart failure can't be cured. You will likely
need to take medicine and follow a treatment plan for the rest of your life.
Despite treatment, your symptoms may get worse over time. Following your
treatment plan, taking steps to prevent heart failure from getting worse, and
planning ahead can help you stay healthier longer.
- Researchers are finding and testing new
treatments for heart failure. These treatments offer hope for the future. Talk
to your doctor about whether research studies may benefit you.
Links to Other Information About Heart Failure
NHLBI Resources
Non-NHLBI Resources
Clinical Trials
|