|
Ways To Manage Physical Changes
Fatigue
Memory and Concentration Changes
Pain
Nervous System Changes (Neuropathy)
Lymphedema or Swelling
Mouth or Teeth Problems
Changes in Weight and Eating Habits
Trouble Swallowing
Bladder or Bowel Control Problems
Menopause Symptoms
"If I could stop feeling so tired all the time,
I think I'd be fine. I've started getting
used to everything else."
- Rosa
|
Some have described survivorship as being "disease-free, but not free of your
disease." What you experience with your body may be related to the type of
cancer you had and the treatment you received. It's important to remember
that no two people are alike, so you may experience changes that are very
different from someone else's, even if that person had the same type of cancer
and treatment.
You may find that you are still coping with the effects of treatment on your body.
It can take time to get over these effects. You may wonder how your body should
feel during this time and what are signs that cancer is coming back. This section
describes some of the problems that can occur when treatment is over. Some of the
most common problems that people report are:
- Fatigue
- Memory and concentration changes
- Pain
- Nervous system changes (neuropathy)
- Lymphedema, or swelling
- Mouth or teeth problems
- Changes in weight and eating habits
- Trouble swallowing
- Bladder or bowel control problems
- Menopause symptoms
Some cancer survivors report that they still feel tired or worn out. In fact, fatigue
is one of the most common complaints during the first year of recovery.
Rest or sleep does not cure the type of fatigue that you may have. Doctors do not
know its exact causes. The causes of fatigue are different for people who are
receiving treatment than they are for those who have finished.
- Fatigue during treatment can be caused by cancer therapy. Other problems
can also play a part in fatigue, like anemia (having too few red blood cells)
or having a weak immune system. Poor nutrition, not drinking enough
liquids, and depression can also be causes. Pain can make fatigue worse.
-
Researchers are still learning about what may cause fatigue after treatment.
How long will fatigue last? There is no normal pattern. For some, fatigue gets
better over time. Some people, especially those who have had bone marrow
transplants, may still feel energy loss years later.
Some people feel very frustrated when fatigue lasts longer than they think it
should and when it gets in the way of their normal routine. They may also
worry that their friends, family, and coworkers will get upset with them if they
continue to show signs of fatigue.
Getting Help
Talk with your doctor or nurse about what may be causing your fatigue and what
can be done about it. Ask about:
- How any medicines you are taking or other medical problems you have
might affect your energy level
-
How you can control your pain, if pain is a problem for you
-
Exercise programs that might help, such as walking
-
Relaxation exercises
-
Changing your diet or drinking more fluids
-
Medicines or nutritional supplements that can help
-
Specialists who might help you, such as physical therapists, occupational
therapists, nutritionists, or mental health care providers
|
Coping With Fatigue
|
|
Here are some ideas:
- Plan your day. Be active at the time of day when you feel most alert
and energetic.
- Save your energy by changing how you do things.
For example, sit on a stool while you cook or wash dishes.
- Take short naps or rest breaks between activities.
- Try to go to sleep and wake up at the same time every day.
- Do what you enjoy, but do less of it. Focus on old or new
interests that don't tire you out. For example, try to read something
brief or listen to music.
- Let others help you. They might cook a meal, run errands, or do
the laundry. If no one offers, ask for what you need. Friends and family
might be willing to help but may not know what to do.
- Choose how to spend your energy. Try to let go of things that
don't matter as much now.
- Think about joining a support group. Talking about your fatigue
with others who have had the same problem may help you find new
ways to cope.
|
"Not being able to concentrate the way I used to
has been the hardest for me. I'm hoping it doesn't
affect my work."
- Josh
Research shows that one in four people with cancer reports memory and
attention problems after chemotherapy. This is sometimes called "chemobrain."
Many survivors describe this as "brain fog," which can lead to problems paying
attention, finding the right word, or remembering new things.
These effects can begin soon after treatment ends, or they may not appear until
much later. They don't always go away. If a person is older, it can be hard to tell
whether these changes in memory and concentration are a result of treatment or
of the aging process. Either way, some feel they just can't focus as they once did.
Research is starting to explore why some people develop problems with memory
and concentration while others don't. It seems that people who have had
chemotherapy or have had radiation to the head area are at higher risk for these
problems. People who had high doses of chemotherapy may have memory
problems, but even those who had standard doses have reported memory changes.
Getting Help
Your doctor can help you with memory and concentration problems. Talk with
him or her if:
- You are still having memory and thinking problems. You may
want to ask about seeing a specialist (called a neuropsychologist) to help
you with these problems.
- You think a medicine you are taking could be causing or
adding to your problem.
- You think you suffer from depression or anxiety. These problems
can affect attention, concentration, and memory.
- You are going through menopause. Some memory and
concentration problems can be related to menopause.
|
Improving Memory and Concentration
|
|
Cancer survivors have found many ways to help improve their memory
after cancer treatment. See if any of these ideas work for you:
- Jot it down. You can write down each task, how long it will take,
and where you need to go in a notebook or pocket calendar. Plan your
whole day. Keep it simple, and be realistic about how much you can do
in a day.
- Set up reminders. Put small signs around the house to remind you
of things to do, such as taking out the trash or locking the door.
- Group long numbers into chunks. For example, the phone number
812-5846 can be repeated as "eight-twelve, fifty-eight, forty-six."
- Talk yourself through tasks. When doing a task with a number of
steps, such as cooking or working on a computer, whisper each step to
yourself.
- Manage stress. Managing stress better may improve your memory
and attention. And learning how to relax can help you remain calm
even in stressful moments.
- Go over what you plan to say. Before you go to family events or
work functions, go over names, dates, and key points you want to make.
- Repeat what you want to remember. Saying it a couple of times
can help your mind hold on to the information.
|
Some people have a lot of pain after treatment, while others have less. Everyone
is different. Types of pain you may feel after cancer treatment include:
- Pain or numbness in the hands and feet due to injured nerves.
Chemotherapy or surgery can damage nerves, which can cause severe
pain. For more information on nervous system changes, see Nervous System Changes (Neuropathy).
- Painful scars from surgery.
- Pain in a missing limb or breast. While doctors don't know why this
pain occurs, it is real. It's not just "in your mind." This is sometimes called
phantom pain.
Getting Help
If you find that you still have pain after treatment ends, your doctor can help
find the source of your pain and get relief. You do not have to be in pain. And
wanting to control pain is not a sign of weakness. It's a way to help you feel
better and stay active. Pain may be caused by treatment or other health issues,
such as arthritis.
With your help, your doctor can assess how severe your pain is and may
recommend one or more of the following approaches:
- Pain-relief medicines. In most cases, doctors will try the mildest
medicines first. Then they will work up to stronger ones if you need them.
The key to getting relief is to take all medicines just as your doctor
prescribes. To keep pain under control, do not skip doses or wait until you
hurt to take these medicines.
|
You may be afraid that if you use these medicines you'll become addicted, but this
rarely happens if you take the correct dose and see your doctor regularly.
|
- Antidepressant medicines. Some of these are prescribed to reduce pain
or numbness from injured nerves.
- Physical therapy. Going to a physical therapist may help relieve your
pain. The therapist may use heat, cold, massage, pressure, and/or exercise
to help you feel better.
- Braces. These limit movement of a painful limb or joint.
- Acupuncture. This is a proven method that uses needles at pressure points
to reduce pain.
- Hypnosis, meditation, or yoga. Any of these may help your pain. A
trained specialist can teach you these approaches.
- Relaxation skills. Many people with cancer have found that practicing
deep relaxation helps relieve their pain or reduce their stress.
- Nerve blocks or surgery. If you don't get relief from the other
approaches in this section, you may want to ask your doctor about these.
Nerve blocks or surgery often help if you have persistent, limiting pain,
but they may put you at risk for other problems. They may also require
you to stay in the hospital.
|
Talking With Your Doctor About Pain
|
|
There are different ways you can describe your pain to your doctor:
- Use numbers. Talk about how strong the pain feels on a scale of 0 to
10, with 0 being no pain and 10 being the worst pain you could have.
- Describe what the pain feels like. Is it sharp, dull, throbbing, steady?
- Point out the exact places it hurts, either on your body or on a
drawing. Note whether the pain stays in one place or whether it moves
outward from the spot.
- Explain when you feel pain. Note when it starts, how long it lasts,
if it gets better or worse at certain times of the day or night, and if
anything you do makes it better or worse.
- Describe how your pain affects your daily life. Does it stop you
from working? Doing household chores? Seeing friends and family?
Going out and having fun?
- Make a list of all the medicines you are taking (for any
reason). If you are taking any for pain relief, how much do they help?
- Talk about any side effects you have from your pain control
medicine, such as constipation or other changes in bowel habits, or
feeling groggy or "out of it." Many of these problems can be helped.
- Keep a record of your pain. Jotting down notes about your pain can
help you track changes over time. It can also show how you respond to
any pain control medicine or other treatment you receive.
|
|
Make sure your insurance covers the pain relief approaches your doctor recommends.
|
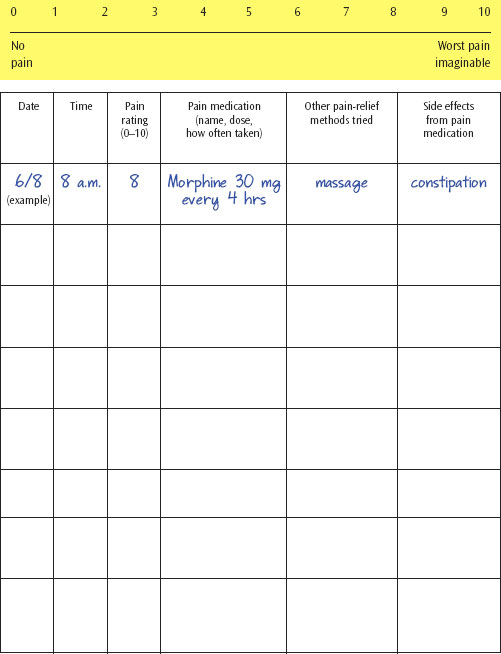
Pain Diary
Use this pain diary and pain rating scale to record your pain.
(You may want to photocopy this sheet before writing on it.)
Sometimes cancer treatment can cause damage to your nervous system. This is
called neuropathy (new-RAH-path-ee), or problems with nerve function.
Sometimes these symptoms can be made worse by other conditions, such as
diabetes, kidney failure, alcoholism, and malnutrition. Most people first notice
symptoms in their hands or feet, usually starting with their fingertips and toes.
Sometimes, the tingling and pain move up the fingers to the hands or from the
toes to the feet.
Common symptoms include tingling, burning, weakness, or numbness in your
hands or feet; sudden, sharp, stabbing, or electric shock pain sensations; loss of
sensation of touch; loss of balance or difficulty walking; clumsiness; trouble
picking up objects or buttoning clothes; hearing loss; jaw pain; constipation; and
being more - or less - sensitive to heat and cold.
Symptoms can start when you begin chemotherapy or after treatment. If they do,
tell your health care team right away. Symptoms can improve over time, but it may
take up to a year or more.
Getting Help
- Treatments include medications, topical creams, and pain patches.
- Other approaches include acupuncture, physical therapy, and exercise.
|
Managing Nervous System Changes
|
- Be careful when handling knives, scissors, and other sharp objects.
- Avoid falling. Walk slowly, hold onto handrails, and put no-slip bath
mats in your tub or shower. Remove area rugs or cords you could trip over.
Steady yourself when you walk by using a cane or other device.
- Wear tennis shoes or other footwear with rubber soles.
- Use a thermometer and gloves instead of your bare hand.
These can help you avoid being burned when checking water temperature.
If possible, lower the temperature setting on your hot water heater.
- Allow yourself time to rest.
|
Lymphedema (LIMF-eh-DEE-ma) is a swelling of a part of the body caused by the buildup of lymph
fluids. It often happens in the arm, leg, face, or neck. It can be caused by cancer
or its treatment. There are many different types of lymphedema. Some types
happen right after surgery, are mild, and don't last long. Other types can occur
months or years after cancer treatment and can be quite painful. These types can
also develop after an insect bite, minor injury, or burn.
People who are at risk for lymphedema are those who have had:
- Breast cancer. If you had radiation therapy, or had your underarm
lymph nodes removed, or had radiation in the underarm area after your
lymph nodes were removed
- Melanoma of the arms or legs. If you had lymph nodes removed
and/or had radiation therapy
- Prostate cancer. If you had surgery or radiation therapy to the
whole pelvis
- Cancer of the female or male reproductive organs. If you had
surgery to remove lymph nodes or had radiation therapy
- Other cancers that have spread to the lower abdominal area.
The pressure from the growing tumor can make it hard for your body to
drain fluid.
Getting Help
Your doctor or nurse may be able to help you find ways to prevent and relieve
lymphedema. Ask about:
- Skin care. It's important to keep your skin clean. You should also use
lotion to keep it moist.
- Exercise. Find out about exercises to help the body drain lymph fluid
and what types of exercise you should not do.
- Ways to treat lymphedema. Your doctor may suggest:
- Keeping the arm or leg raised above your chest for periods of time
- Having special types of massage that can help by moving the lymph
fluid from where it has settled
- Wearing special elastic sleeves and clothing that can help lymph
fluid drain
- Losing weight
- Finding sources of emotional support to help you cope
- Avoiding procedures done in the area with lymphedema, such as
shots or blood tests
|
Preventing or Relieving Lymphedema
|
|
Other cancer survivors have found these tips helpful:
- Watch for signs of swelling or infection (redness, pain, heat,
fever). Tell your doctor or nurse if your arm or leg is painful or swollen.
- Keep your arm or leg free of cuts, insect bites, and sunburn.
Try not to have shots or blood tests done in that area.
- Eat a well-balanced, protein-rich, low-salt diet.
- Keep regular follow-up appointments with your doctor.
- Wear loose-fitting clothing on your arm or leg.
- Protect the area. Try not to use that arm or leg to figure out how
hot or cold something is, such as bath water or cooked food. You may be
less able to feel hot and cold now.
|
Many people who have been treated for cancer develop problems with their
mouth or teeth. Some problems go away after treatment. Others last a long time,
while some may never go away. Some problems may develop months or years
after your treatment has ended.
Radiation or surgery to the head and neck can cause problems with your teeth
and gums; the soft, moist lining of your mouth; glands that make saliva (spit);
and jawbones. If you were treated with certain types of chemotherapy, you may
also have these problems. This can cause:
- Dry mouth
- Cavities and other kinds of tooth problems
- Loss of or change in sense of taste
- Painful mouth and gums
- Infections in your mouth
- Jaw stiffness or jawbone changes
Who Has These Problems?
- Almost all people who have had radiation therapy to the head and neck
- Most people who have had bone marrow transplants
- About two out of every five people treated with chemotherapy
Getting Help
If you find that problems persist after cancer treatment ends, talk with your
doctor about possible causes and ways to control mouth pain.
Try to see your dentist soon after you are done with treatment. Ask how often
you should have checkups and ways to take care of your mouth and teeth.
|
Preventing or Relieving Mouth or Teeth Problems
|
- Keep your mouth moist.
- Drink a lot of water.
- Suck on ice chips.
- Chew sugarless gum or suck on sugar-free hard candy.
- Use a saliva substitute to help moisten your mouth.
- Keep your mouth clean.
- Brush your teeth, gums, and tongue with an extra-soft toothbrush
after every meal and at bedtime. If it hurts, soften the bristles in
warm water.
- Ask your dentist for tooth sponges, such as Toothettes® or Dentips®,
that you can use in place of a toothbrush.
- Use a mild fluoride toothpaste (like children's toothpaste) and a
mouthwash without alcohol.
- Floss your teeth gently every day. If your gums bleed or hurt, stay
away from the areas that are bleeding or sore, but keep flossing your
other teeth.
- Rinse your mouth several times a day with a solution of 1/4 teaspoon
baking soda and 1/8 teaspoon salt in 1 cup of warm water. Follow with
a plain water rinse.
- If you have dentures, clean, brush, and rinse them after meals. Have
your dentist check them to make sure they still fit you well.
- If your mouth is sore, remember to stay away from:
- Sharp, crunchy foods, like chips, that can scrape or cut your mouth
- Foods that are hot, spicy, or high in acid, like citrus fruits and juices,
which can irritate your mouth
- Sugary foods, like candy or soda, that can cause cavities
- Toothpicks (they can cut your mouth)
- All tobacco products
- Alcoholic drinks
|
Some survivors who have had certain kinds of chemotherapy or medicines have
problems with weight gain. Sometimes the added pounds stay on even when
treatment ends. Breast cancer survivors who have had certain types of
chemotherapy gain weight in a different way - they may lose muscle and gain
fat tissue.
Unfortunately, the usual ways people try to lose weight may not work for them.
Try to be patient with yourself. Look for the positive things that you can control,
such as eating a healthy diet. Try to focus on the fact that treatment is over, and
you are trying to get stronger with time.
Some cancer survivors have the opposite problem: they have no desire to eat,
and they lose weight. Some men say that weight loss or loss of muscle tone is a
bigger concern for them than weight gain. It makes them feel less strong and like
less of a man.
Managing a Healthy Weight
For weight issues, ask your doctor or nurse about:
- Doing strength-building exercises, if you have lost muscle or gained
fat tissue
- Talking to a dietitian or nutritionist who can help you plan a healthy diet
that won't add extra pounds
|
Regaining a Lost Appetite
|
|
Here are some tips that have helped others improve their appetites:
- Start with small meals. Five small meals a day may be easier to
manage than three larger ones.
- Focus on your favorite foods. If the thought of eating still lacks
appeal, try the foods you really liked before treatment to jump-start your
appetite. Try adding some fresh fruit, juice, or other flavoring to improve
the taste.
- Stay active. A short walk before a meal can help you feel hungry.
|
Some people who have had radiation therapy or chemotherapy may find it hard
to eat because they have trouble swallowing. People who have had radiation
therapy to the head, neck, breast, or chest or those who have had surgery
involving the larynx may also have this problem.
Getting Help
- Eat soft, bland foods moistened with sauces or gravies. Puddings, ice cream,
soups, applesauce, and bananas and other soft fruits are nourishing and
usually easy to swallow.
- Use a blender to process solid foods.
- Ask for advice from your health care team, including your doctor, nurse,
nutritionist, and/or speech pathologist.
- Tilt your head back or move it forward while you are eating.
- Have a sip of water every few minutes to help you swallow and talk more
easily. Carry a water bottle with you so you always have some handy.
Bladder and bowel problems are among the most upsetting issues people face
after cancer treatment. People often feel ashamed or fearful to go out in public.
"Going back to work was the hardest thing," one prostate cancer survivor noted.
This loss of control can happen after treatment for bladder, prostate, colon,
rectal, ovarian, or other cancers. Your surgery may have left you with no bladder
or bowel control at all. Or perhaps you still have some control, but you make
lots of sudden trips to the bathroom. The opposite problem can happen when a
medicine you are taking for pain causes constipation.
Getting Help
It is very important to tell your doctor about any changes in your bladder or
bowel habits. Ask your doctor or nurse about:
- Problems with constipation
- Kegel exercises (see Changes in Sex Life on muscle weakness)
- Medicines that may help
- Help in coping with ostomies. If you have an ostomy, an opening from
inside the body to the outside to pass urine or waste material, there are
services and support groups to help you cope with changes (see Services to Think About).
After chemotherapy, some women stop getting their periods every month - or stop
getting them altogether. Some cancer treatments (and the medicines tamoxifen
and raloxifene) can cause changes in women's bodies and reduce the amount of
hormones they make. These changes can cause your periods to stop, as well as
cause other symptoms of menopause (also called "the change" or "change of life").
Over time, some women will start getting their periods again (this is more likely
for younger women), but others will not. Even though your doctor may have
discussed early menopause with you, give yourself permission to mourn the loss
of your fertility.
Some common signs of menopause are:
- Irregular periods. One of the first signs is a change in your periods.
They may become less regular. They could be lighter. Some women have
short times of heavy bleeding. Sometimes, they stop all of a sudden.
- Hot flashes. Hot flashes are often worse at night and can affect sleep or
cause mood changes.
- Problems with your vagina or bladder. Tissues in these areas
become drier and thinner. You may be more likely to get vaginal
infections. As you get older, you may also have problems holding your
urine or urinary tract problems.
- Lack of interest in having sex. These changes may make it hard for
you to become sexually aroused.
- Fatigue and sleep problems. You may feel tired or have trouble getting
to sleep, getting up early, or getting back to sleep after waking up in the
middle of the night.
- Memory and other problems, such as depression, mood swings,
and irritability. Some of these, especially memory problems, may be
related to growing older. There may be a connection between changes in
your hormone levels and your emotions.
- Other changes in your body. You may notice your waist getting bigger,
less muscle and more fat around your body, or thinning and loss of
elasticity of your skin.
|
Ask your doctor if you still need to use birth control, even if you are not getting
your period.
|
Getting Help
See a gynecologist every year. Ask about:
- Medicines, supplements, or other approaches that can help you manage
menopause symptoms
- Tests you should have (such as a bone density test to see if you are at risk
for osteoporosis)
- Ways you can reduce your chance of getting:
- Osteoporosis. Menopause can put you at risk for losing bone tissue,
which can weaken your bones and make them easier to break.
- Heart disease. Menopause can also lead to higher cholesterol, which
can increase your risk of diseases that affect your heart and blood vessels.
|
Relieving Hot Flashes
|
|
Here are some tips that have helped others deal with hot flashes:
- Quit smoking.
- Drink plenty of water.
- Through exercise and diet, try to maintain a healthy weight.
Exercise most days of the week, doing both weight-bearing and muscle-strengthening
activities. Eat wisely. A balanced diet will provide most of
the nutrients and calories your body needs to stay healthy.
- If you are having hot flashes, try to write down when they happen
and what may cause them. This may help you find out what to avoid.
You may also want to:
- Sleep in a cool room to avoid being awakened by hot flashes.
- Dress in layers that you can take off if you get warm.
- Use cotton sheets, and wear clothing that lets your skin "breathe."
- Try having a cold drink or turning on a fan at the beginning of a
hot flash.
- Try not to eat a lot of spicy foods.
- Limit the alcohol and caffeine you drink.
|
Back to Top
< Previous Section | Next Section > |