 |
|
 |

Allogeneic Stem-Cell Transplant Survivors Face Long-Term Challenges
People who undergo allogeneic hematopoietic stem-cell transplantation 1 (HCT) and survive for at least 2 years remain at increased risk of premature death even 15 years after treatment, reports a new study published online August 1 in Blood. This group of survivors also faces long-term challenges affecting their overall health and well-being, including difficulty maintaining employment, as well as finding and retaining health and life insurance.
Advances in stem-cell transplantation "have made it a curative therapeutic option," explains Dr. Smita Bhatia, professor of population sciences at City of Hope Comprehensive Cancer Center and lead author of the study. "We need to focus on the survivors. Half [of the cohort we studied] has survived longer than nine and a half years, and one thing that we have shown quite definitively is that these survivors continue to face challenges."
Read more 2 


Guest Update by Dr. Robert Croyle
The Imperative of Improving Colorectal Cancer Screening Rates
 A study published last October in Cancer modeled how different scenarios - each of which took into account changes in screening, risk factors, and optimal use of chemotherapy - would influence mortality rates from colorectal cancer, the second leading cause of cancer death. In every scenario, mortality was decreased by varying degrees over the next two decades, but in each case the most influential factor was improved screening rates.
A study published last October in Cancer modeled how different scenarios - each of which took into account changes in screening, risk factors, and optimal use of chemotherapy - would influence mortality rates from colorectal cancer, the second leading cause of cancer death. In every scenario, mortality was decreased by varying degrees over the next two decades, but in each case the most influential factor was improved screening rates.
It's a troubling fact, however, that colorectal cancer screening rates continue to lag well behind those for other cancers. This is discouraging given that, when caught early, colorectal cancer is highly curable.
The reasons behind this shortfall are complex, but there is widespread agreement that if significant improvements in colorectal cancer screening are to be realized, the primary care setting will be the most crucial contributor. Read more 3 
 |
The NCI Cancer Bulletin is produced by the National Cancer Institute (NCI). NCI, which was established in 1937, leads the national effort to eliminate the suffering and death due to cancer. Through basic, clinical, and population-based biomedical research and training, NCI conducts and supports research that will lead to a future in which we can identify the environmental and genetic causes of cancer, prevent cancer before it starts, identify cancers that do develop at the earliest stage, eliminate cancers through innovative treatment interventions, and biologically control those cancers that we cannot eliminate so they become manageable, chronic diseases.

For more information on cancer, call 1-800-4-CANCER or visit http://www.cancer.gov.

NCI Cancer Bulletin staff can be reached at ncicancerbulletin@mail.nih.gov. |
|
 |
 |

Allogeneic Stem-Cell Transplant Survivors Face Long-Term Challenges
People who undergo allogeneic hematopoietic stem-cell transplantation 1 (HCT) and survive for at least 2 years remain at increased risk of premature death even 15 years after treatment, reports a new study published online August 1 in Blood. This group of survivors also faces long-term challenges affecting their overall health and well-being, including difficulty maintaining employment, as well as finding and retaining health and life insurance.
Advances in stem-cell transplantation "have made it a curative therapeutic option," explains Dr. Smita Bhatia, professor of population sciences at City of Hope Comprehensive Cancer Center and lead author of the study. "We need to focus on the survivors. Half [of the cohort we studied] has survived longer than nine and a half years, and one thing that we have shown quite definitively is that these survivors continue to face challenges."
These results come from long-term follow-up data from the Bone Marrow Transplant Survivor Study (BMTSS), which began in 2000 and comprises a cohort of 1,479 patients who underwent allogeneic HCT for cancers of the blood or for bone-marrow dysfunction at City of Hope or the University of Minnesota between 1974 and 1998.
Out of all patients who survived at least 2 years after transplantation, 21.6 percent had died by June 30, 2003. The probability of surviving was 86.6 percent at 5 years, 80.4 percent at 10 years, and 76.3 percent at 15 years from HCT. "Overall, premature death occurred 10 times more often than expected" compared to the general population, explain the authors. Treatment-related morbidities and chronic graft-versus-host disease accounted for 25 percent and 22 percent of the deaths, respectively.
Relative mortality compared with the general population was highest 2 to 5 years after HCT, but remained twice as high even 15 years after transplantation. Survivors had specific risks of mortality related to the effects of treatment on vital organ systems, including a 15.1 percent greater risk of death due to pulmonary dysfunction and a 2.3 percent greater risk of death due to cardiac complications.
To gather a clearer picture of the challenges to functional well-being faced by survivors, the investigators collected survey data from 547 BMTSS participants and 319 nearest-age siblings. Compared with the siblings, survivors were 14 times more likely to report a health problem preventing them from holding a job, 7 times more likely to report difficulty obtaining or retaining health insurance, and 10 times more likely to report difficulty obtaining or retaining life insurance. Survivors were also significantly less likely to be married compared with healthy siblings. "They're facing challenges re-integrating back into society," comments Dr. Bhatia.
"This population needs very specialized follow-up to look out for late effects or complications," she continued. "We either need to develop really good communications between the cancer-care and transplant teams and patients’ regular physicians, or we need to have a mechanism available at the transplanting centers to follow transplant patients for life."
Dr. Julia Rowland, director of the NCI Office of Cancer Survivorship 4, agrees with these conclusions. "This report argues strongly for the need, which is being supported by the advocacy community 5, for survivors to receive a treatment summary at the end of their therapy and a care plan going forward," she said. "These documents would detail the type of cancer the survivor had, the treatments received, and potential problems for which she or he might be at increased risk as a result, and, importantly, outline recommended follow-up care. Together, they would serve as a guide for survivors and their health care providers in planning for future cancer surveillance and health care needs.
"A number of the complications identified in this study, both physical and psychosocial, potentially could be mitigated with early interventions. Thus, systematic follow-up, with timely identification and treatment of these complications, could enable us to further reduce the late morbidity and mortality for these survivors," Rowland concluded.
By Sharon Reynolds
|
 |
 |

Guest Update by Dr. Robert Croyle
The Imperative of Improving Colorectal Cancer Screening Rates
 A study published last October in Cancer modeled how different scenarios - each of which took into account changes in screening, risk factors, and optimal use of chemotherapy - would influence mortality rates from colorectal cancer, the second leading cause of cancer death. In every scenario, mortality was decreased by varying degrees over the next two decades, but in each case the most influential factor was improved screening rates.
A study published last October in Cancer modeled how different scenarios - each of which took into account changes in screening, risk factors, and optimal use of chemotherapy - would influence mortality rates from colorectal cancer, the second leading cause of cancer death. In every scenario, mortality was decreased by varying degrees over the next two decades, but in each case the most influential factor was improved screening rates.
It's a troubling fact, however, that colorectal cancer screening rates continue to lag well behind those for other cancers. This is discouraging given that, when caught early, colorectal cancer is highly curable.
The reasons behind this shortfall are complex, but there is widespread agreement that if significant improvements in colorectal cancer screening are to be realized, the primary care setting will be the most crucial contributor.
Indeed, the colorectal cancer screening research portfolio supported by NCI's Division of Cancer Control and Population Sciences 6 (DCCPS) includes many studies set in community and primary care settings, including those that focus on minority, low-resource, and underserved populations.
Since 2001, researchers from DCCPS and the Agency for Healthcare Research and Quality 7 (AHRQ) have been collaborating to develop research to improve colorectal cancer screening in primary care practice. These researchers - led by Dr. Carrie Klabunde from DCCPS' Applied Research Program 8 - have published a paper in the August Journal of General Internal Medicine (JGIM) that reviews the published literature for innovative strategies to improve colorectal cancer screening rates and, as importantly, identifies some of the knowledge gaps that should be considered high priorities for future research.
This review is particularly compelling because it uses recent recommendations from the Society for General Internal Medicine and American Academy of Family Physicians for a new primary care practice model as its frame. This influential model is built on six core elements: a team approach to care delivery, advanced information systems, patient-centered care, improved efficiency and quality of services, enhanced practice finances, and training opportunities.
Developing and reviewing strategies for screening improvements based on this new model will ensure their relevance to primary care practice. And, most of the strategies under investigation work well with this new model because they primarily target systems of care instead of the individual physician.
In the area of team delivery of care, for example, the JGIM review highlights studies that have shown how giving medical personnel other than the physician important responsibilities related to screening - including ordering tests and conducting telephone counseling - greatly increased fecal occult blood test rates. These results are consistent with the findings of other studies of preventive services and strongly support a multidisciplinary team approach in the primary care setting.
Use of electronic health records (EHRs) is also a subject of investigation. Studies have shown, for example, that these advanced information system tools allow medical practices to better track their patients' adherence to recommended screenings and automate activities like reminder calls. The JGIM review, however, underscored the sluggish adoption of EHRs and other advanced IT systems in primary care, and stressed that more research is needed to identify and help practices overcome the obstacles to adoption.
Nongovernmental organizations, such as the American Cancer Society, have played a key role in raising public awareness about the benefits of early detection. And we are confident that NCI- and AHRQ-funded research on colorectal cancer screening will generate useful interventions that will lead to more people receiving screening for this disease. The JGIM paper highlights innovative strategies as well as questions that must be answered to realize progress toward improving colorectal cancer screening rates - progress that could save many lives.
|
 |
 |
HPV Vaccine Not Effective for Treating Pre-Existing Infections
A vaccine developed to prevent infection with human papillomaviruses (HPV), the cause of cervical cancer, was found to be ineffective for treating women with pre-existing HPV infections, according to a study published in the August 15 Journal of the American Medical Association.
The study, a community-based, randomized trial 9 of 2,189 women in Costa Rica, was conducted by NCI's Division of Cancer Epidemiology and Genetics 10 (DCEG) and Costa Rican investigators. The researchers found no significant difference in how quickly an HPV infection was cleared among those who received the HPV vaccine compared with the control group who received vaccinations for hepatitis A. At the 6-month follow-up visit, rates of viral clearance were 33.4 percent for women who received vaccines against HPV types 16 and 18 compared with a 31.6 percent rate among the control group. At the 12-month visit, rates of clearance in the HPV vaccine group were 48.8 percent versus 49.8 percent for the controls.
"The main finding of the study was to demonstrate that among women who are already infected, the HPV vaccine does not help accelerate the rate of viral clearance," commented Dr. Allan Hildesheim with DCEG. "Therefore, women who are infected with HPV should not take the vaccine to treat their infections or associated lesions." The study reinforces the importance of targeting HPV vaccination towards adolescent girls before they begin sexual activity "because that would maximize the benefit provided by vaccination," he added.
The study is part of a larger community-based clinical trial of 7,466 Costa Rican women 11. The larger study will address broad issues about the vaccine including efficacy, duration of protection, and global impact of vaccination on HPV and HPV-related disease. Among other questions, "the study will address whether vaccination is important for women who have previously been infected and have cleared the infection by themselves," said Dr. Hildesheim.
Drug Combination Shows Benefit in Relapsed/Refractory Multiple Myeloma
Interim results from a phase III clinical trial suggest a new combination treatment should be another standard of care for patients with relapsed or refractory multiple myeloma, according to the trial's leaders.
In the most recent survival analysis from the 646-patient trial, released early online on August 6 in the Journal of Clinical Oncology, the combination of pegylated liposomal doxorubicin 12 (Doxil) and bortezomib 13 (Velcade) improved the median time to disease progression compared with bortezomib alone (9.3 months vs. 6.5 months) and yielded a superior 15-month overall survival rate (76 percent of patients in the combination group were alive at 15 months compared with 65 percent in the bortezomib-only group).
The results come 2 years after a phase III trial showed that 14 bortezomib alone was superior to dexamethasone, another drug commonly used to treat all stages of multiple myeloma, and 1 year after a trial demonstrated that the combination of lenalidomide 15 (Revlimid) and dexamethasone was superior 16 to dexamethasone alone in patients with refractory or relapsed disease.
The bortezomib/Doxil combination also increased the duration of response, reported the study's principal investigator, Dr. Robert Z. Orlowski from the University of Texas M.D. Anderson Cancer Center, and colleagues. However, the combination's benefits came at the expense of an increased risk of adverse events, including high-grade hematologic (e.g., neutropenia) and gastrointestinal (e.g., diarrhea, nausea) toxicities.
Based on the results of this trial, also known as the DOXIL-MMY-3001 study 17, the U.S. Food and Drug Administration recently approved the use of this combination for treating patients with multiple myeloma who have not previously received bortezomib and have received at least one prior therapy.
Irinotecan Not Effective in Adjuvant Therapy for Colon Cancer
Final results from a Cancer and Leukemia Group B 18 (CALGB) trial show that irinotecan 19 should not be added to 5-fluorouracil (5-FU) and leucovorin in the adjuvant treatment of stage III colon cancer. In the CALGB 89803 20 trial, led by Dr. Leonard B. Saltz and colleagues at Memorial Sloan-Kettering Cancer Center, no survival benefit was seen in the adjuvant setting. These results appear in the August 10 Journal of Clinical Oncology.
"These results were unexpected," writes Dr. Neal Meropol of the Fox Chase Cancer Center in Philadelphia in a related editorial. "After all, CPT 11 [irinotecan] had previously shown clear activity in patients with metastatic cancer - the accepted proving ground for subsequent adjuvant therapies."
In previous trials, Dr. Saltz and others had found that adding irinotecan to 5-FU and leucovorin provided a modest but statistically significant improvement in survival compared to treatment with 5-FU and leucovorin alone in patients with metastatic colon cancer. Based on these findings, it was anticipated that the three-drug combination would also be effective when given after surgery to patients with less advanced disease.
"The report by Saltz et al. sends a strong message," said Meropol. "Randomized trials are necessary to prove the obvious, [because] history tells us that the obvious is often disproved."
Saltz and colleagues agreed. "The results of our trial demonstrate the dangers of jumping to conclusions before completion of the formal clinical trial assessment."
In addition, combining irinotecan with 5-FU and leucovorin significantly increased treatment toxicity, including greater reductions in white blood cell counts and increases in infection, vomiting, and fatigue. More than 10 percent (65) of the 635 patients assigned to the irinotecan-containing arm had their treatment stopped because of an adverse event. Another 82 patients receiving the three-drug combination withdrew from the trial, more than twice the number of patients who withdrew from the 5-FU plus leucovorin arm. Within 60 days of entering the study, 14 patients receiving irinotecan died, compared to 5 in the 5-FU and leucovorin arm.
|
 |
 |
Following are newly released NCI research funding opportunities:
Genome-Wide Association Studies in the Genes, Environment, and Health Initiative - Study Investigators
Announcement Number: RFA-HG-07-012
Letter of Intent Receipt Date: September 18, 2007
Application Receipt Date: October 18, 2007
This is a renewal of RFA-HG-06-033 and will use the U01 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3757. Inquiries: Dr. Emily L. Harris - emily.harris@nih.gov
Clinical Research Education and Career Development in Minority Institutions
Announcement Number: RFA-RR-07-005
Letter of Intent Receipt Date: September 24, 2007
Application Receipt Date: October 24, 2007
This is a renewal of RFA-RR-06-003 and will use the R25 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3759. Inquiries: Dr. H. Nelson Aguila - aguilah@mail.nih.gov
Epidemiologic Investigation of Putative Causal Genetic Variants - Study Investigators
Announcement Number: RFA-HG-07-014
Letter of Intent Receipt Date: October 19, 2007
Application Receipt Date: November 19, 2007
This funding opportunity will use the U01 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3758. Inquiries: Dr. Erin M. Ramos - ramoser@mail.nih.gov
Data Ontologies for Biomedical Research
Announcement Number: PAR-07-425
Letter of Intent Receipt Dates: December 18, 2007; August 18, 2008; December 22, 2008; and August 21, 2009
Application Receipt Dates: January 18, 2008; September 18, 2008; January 21, 2009; and September 21, 2009
This funding opportunity will use the R01 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3760. Inquiries: Dr. Jennifer Couch - couchj@mail.nih.gov
Sharing Data and Tools: Federation Using the Biomedical Informatics Research Network and caBIG Infrastructures
Announcement Number: PAR-07-426
Letter of Intent Receipt Dates: December 18, 2007; August 18, 2008; December 22, 2008; and August 21, 2009
Application Receipt Dates: January 18, 2008; September 18, 2008; January 21, 2009; and September 21, 2009
This funding opportunity will use the R01 award mechanism. For more information, see http://cri.nci.nih.gov/4abst.cfm?initiativeparfa_id=3761. Inquiries: Dr. Jennifer Couch - couchj@mail.nih.gov
|
 |
 |

Testing Carbohydrates as Cancer Biomarkers
 |
 |
Featured Meetings and Events |
 |
| A calendar of scientific meetings and events sponsored by the National Institutes of Health (NIH) is available at http://calendar.nih.gov. |
|
NCI has launched a new initiative to determine whether carbohydrates can be used as biological markers for detecting cancer and assessing disease risk. The $15.6 million, 5-year initiative 21 will complement efforts to identify gene and protein biomarkers by focusing on an important, if understudied, class of molecules.
Like genes and proteins, complex carbohydrates - also known as glycans - may be altered as cancer develops. The goal of the new initiative is to identify panels of glycan-based biomarkers associated with early-stage cancers and validate the panels in clinical samples.
"Glycans represent one of the richest sources of potential cancer biomarkers," says Dr. Karl Krueger of NCI's Division of Cancer Prevention 22 (DCP), who heads the project, called the Alliance of Glycobiologists for Detection of Cancer and Cancer Risk.
Glycans are sugars that are linked together, often forming complex branched-chain structures, and are bound to proteins and lipids, modifying the behavior of these molecules. Glycans have dominated the surfaces of cells for billions of years and are widely thought to mediate many biological processes.
One of the most promising cancer biomarkers in development today is a "glycoprotein" known as GP73. This marker for liver cancer is expected to undergo validation testing through NCI's Early Detection Research Network 23 (EDRN) in the coming months.
EDRN is providing Alliance researchers with expertise on the critical process of validation, where many promising potential biomarkers have failed.
The trans-NIH Alliance includes the Consortium for Functional Glycomics 24, funded by the National Institute of General Medical Sciences (NIGMS), and several Glycomics and Glycotechnology Resource Centers 25 supported by the National Center for Research Resources (NCRR).
Glycans are structurally more complex than DNA or proteins, and this has slowed efforts to study the molecules on a large scale. But recent advances in technologies, such as the development of glycan arrays, have made the initiative feasible.
"The core technologies are in place and this means that researchers can focus on discovering biomarkers rather than building infrastructure," says Dr. Sudhir Srivastava, head of NCI's Cancer Biomarkers Research Group 26, which is sponsoring the initiative.
The initiative is a critical piece of NCI's efforts in biomarker development, adds Dr. Srivastava. "Traditional methods of analyzing DNA and proteins cannot detect cancer-related changes involving glycans," he notes.
Information about glycans could improve the utility of protein-based biomarkers in use today, including prostate-specific antigen for prostate cancer and CA-125 for ovarian cancer. Both proteins have glycan components, and analyzing their molecular features together may yield useful information for physicians and patients, the researchers say.
Alliance members came to NCI for a kick-off meeting last week. It was the first time that glycobiologists had come together in one room with the goal of applying the field's new technologies and insights to the challenge of detecting cancer biomarkers.
If the initiative succeeds, several participants said, interest in glycobiology will grow and carbohydrates just might emerge from the shadow of genes and proteins.
By Edward R. Winstead |
 |
 |
A Conversation with...Dr. LaSalle D. Leffall, Jr.
 The President's Cancer Panel 27, a three-person advisory committee appointed by the President, oversees the National Cancer Program and reports directly to the President any delays or blockages in its rapid execution. Each year, the Panel holds a series of meetings and writes a report to the President on a chosen topic of concern in the cancer community. This year's report, Promoting Healthy Lifestyles: Policy, Program, and Personal Recommendations for Reducing Cancer Risk, examines the effects of obesity, diet and nutrition, physical activity, tobacco use, and tobacco smoke exposure on cancer risk. Dr. LaSalle D. Leffall, Jr., Charles R. Drew Professor of Surgery at Howard University College of Medicine, has served as chair of the Panel since 2002 and was recently reappointed for a third term. The President's Cancer Panel 27, a three-person advisory committee appointed by the President, oversees the National Cancer Program and reports directly to the President any delays or blockages in its rapid execution. Each year, the Panel holds a series of meetings and writes a report to the President on a chosen topic of concern in the cancer community. This year's report, Promoting Healthy Lifestyles: Policy, Program, and Personal Recommendations for Reducing Cancer Risk, examines the effects of obesity, diet and nutrition, physical activity, tobacco use, and tobacco smoke exposure on cancer risk. Dr. LaSalle D. Leffall, Jr., Charles R. Drew Professor of Surgery at Howard University College of Medicine, has served as chair of the Panel since 2002 and was recently reappointed for a third term.
What did the Panel learn from its 2006/2007 series of meetings?
We invited 45 representatives from government agencies, medicine, academia, industry, and the advocacy community to present expert testimony on obesity, diet, physical activity, and tobacco. Much of this testimony focused on recent research linking obesity resulting from unhealthy eating and physical inactivity to increased risk of several cancers, including breast, prostate, colon, and liver cancer. We also learned that many entities not traditionally considered part of the National Cancer Program - educators; employers; city planners; the food, beverage, and tobacco industries; and the media - contribute to the national cancer burden and will need to play a role in the promotion and adoption of healthy living.
From experts in the tobacco field, we learned of mixed progress. For example, the number of Americans living in smoke-free municipalities is rapidly increasing, but at the same time, most state tobacco control programs are significantly underfunded. Speakers also emphasized the need to protect youth and other populations of special concern, such as racial and ethnic minority groups, the poor, and persons with mental illness, from the aggressive advertising and marketing campaigns of tobacco companies.
The Panel chose to focus on obesity and tobacco. Why did the Panel choose these two areas to examine?
We know that there are many other lifestyle factors that affect cancer risk, but we decided to focus specifically on obesity and tobacco because an estimated one-third of preventable cancer deaths are related to diet and another one-third are related to tobacco. This means that more than two-thirds of cancer deaths could be prevented through changes in lifestyle. Alarming obesity trends and stalled declines in smoking rates indicate that America is in need of a significant culture change.
What can governmental and nongovernmental organizations do to help individuals and families live healthier lifestyles?
We encourage policymakers at all levels of government to pass legislation and implement policies that help Americans adopt healthier lifestyles. The Panel believes that Congress should grant the FDA authority to regulate tobacco products and marketing, as well as provide subsidies for production of fruits and vegetables that would make healthy foods more available and affordable. State and local governments must increase funding for tobacco prevention programs and pass ordinances to make all workplaces and public spaces 100 percent smoke-free. Schools should reinstate physical education classes and offer more healthy food options for students. Medicare and Medicaid, as well as private health insurance companies, should provide coverage for nutrition counseling and smoking cessation interventions. Primary care providers need to counsel patients about maintaining a healthy weight and offer smoking cessation services. Individuals and families must also take personal responsibility for their own health by eating healthy foods, exercising, and not smoking.
|
 |
 |

Making Sense of Breast Cancer's Decline
 |
 |
What Happened in 2003? |
 |
Between 2002 and 2003, the incidence of breast cancer declined nearly 7 percent in the United States and remained low through 2004. This sharp decrease was reported 28 last December, and since then researchers have been trying to explain the good news.
Although there is no consensus and no proof of causation, the role of hormone therapy is attracting a lot of attention. The August 2 issue of the New England Journal of Medicine included seven letters 29 to the editor regarding an analysis 30 of the 2003 decline led by Drs. Berry and Ravdin that appeared in the journal last May. Some of the letters challenge the report's conclusion that the bulk of the decline is attributable to the sharp drop in hormone use, while others provide support for the theory.
More support comes from a prospective study of screening and hormone use in more than 600,000 women from 1997 through 2003. A decline in mammography rates is unlikely to explain the recent decline in U.S. breast cancers while a drop in hormone use is a "more likely contributor," researchers in the Breast Cancer Surveillance Consortium 31 reported online in JNCI August 14.
Further insights may be provided by the Cancer Intervention and Surveillance Modeling Network 32, which is modeling the impact of HRT on breast cancer tumor progression and how risk changes when a woman stops using HRT. |
 |
|
A new study of women in a large U.S. health plan suggests that the use of hormone therapy played a key role in both the rise and decline of breast cancer rates in that population since the early 1980s.
The study describes changes in mammography screening, hormone therapy, and breast cancer incidence among women in the Kaiser Permanente Northwest health plan between 1980 and 2006.
The results link both mammography screening and hormone therapy to changes in breast cancer rates. But screening rates remained virtually constant from 1991 through 2006, leading the researchers to suggest that hormone therapy was responsible for the rise and decline of breast cancer rates since the early 1990s.
"The trends in hormone use go a long way toward explaining the fluctuations in breast cancer rates that researchers have been talking about for a long time," says Dr. Andrew Glass of the Kaiser Permanente Center for Health Research. He co-led the study with Drs. Robert Hoover and James Lacey of NCI's Division of Cancer Epidemiology and Genetics 10 (DCEG).
The rates of women getting mammograms did drop slightly from 2000
to 2001 but rebounded in 2005 and 2006, according to findings in the August 1 Journal of the National Cancer Institute (JNCI).
Although the results are from a single population, the breast cancer rates among the Kaiser participants are nearly identical to statistics for the U.S. population.
"This study gives us one of the most comprehensive and up-to-date pictures of what's happening with breast cancer in the United States," says Dr. Lacey.
In the Kaiser population, breast cancer rates rose 26 percent from the early 1980s to early 1990s, paralleling increases in both mammography screening and hormone use. Rates then continued to rise but at a slower rate for another decade. This second rise parallels an increase in hormone use among the population at a time when mammography rates were stable.
After the health risks of taking estrogen-plus-progestin were revealed by the Women's Health Initiative study 33 in July 2002, many Kaiser members, along with millions of other women, abandoned hormones. A sharp drop in breast cancer incidence among Kaiser members after 2003 paralleled a 75-percent drop in hormone therapy use in this population.
"Hormone therapy use was declining gradually in the period before the WHI results were announced," says Dr. Lacey. "People have focused on the dramatic 2003 drop in use, but some of the dynamics that led to the decline were in place earlier."
The researchers' observations are consistent with those from other studies, including some published and some still in press, note Drs. Donald Berry and Peter Ravdin of the University of Texas M.D. Anderson Cancer Center in the accompanying JNCI editorial.
"Hormone use remains an important public health issue," says Dr. Glass. "Millions of women are still taking hormones, and despite the research, some physicians believe these hormones are safe and effective and pose no harm to women."
The current study looked at time trends in practices and disease rates across the Kaiser population as a whole. Dr. Glass and his colleagues are developing plans to use the Kaiser database to link pharmacy, screening, and disease records for individual women. The results could potentially clarify whether women who stopped hormone therapy were less likely to get screened and less likely to be diagnosed with cancer.
The current Kaiser study, which is a follow-up to a 1990 study by Drs. Glass and Hoover, has produced clues to a complicated puzzle at a time when they are needed.
"What we have here is a good example of a natural experiment occurring over time," says Dr. Glass. "You can see the play of the different forces as they take hold."
By Edward R. Winstead
|
 |
 |

Radiation Therapies to Treat Brain Metastases
Name of the Trial
Phase III Randomized Study of Stereotactic Radiosurgery with Versus without Whole-Brain Radiotherapy in Patients with Cerebral Metastases (NCCTG-N0574). See the protocol summary at http://www.cancer.gov/clinicaltrials/NCCTG-N0574.
 Principal Investigators
Principal Investigators
Drs. Paul Brown, Kurt Jaeckle, Richard Deming, Elana Farace, and Bruce Pollock, NCCTG; Drs. Anthony Asher and Fred Barker, ACOSOG; Dr. Anthony Asher, RTOG
Why This Trial Is Important
The spread of cancer to the brain (brain metastases) is common in many types of adult cancer. For patients with brain metastases that can be treated, life may be prolonged significantly.
Whole-brain radiotherapy and stereotactic radiosurgery are methods that have proven useful in treating brain metastases. In whole-brain radiotherapy, radiation is delivered to the entire brain in incremental doses over the course of a few weeks. In stereotactic radiosurgery, radiation is delivered in a higher single dose directly to the tumor, minimizing the exposure of normal brain cells to harmful radiation.
In this trial, doctors are comparing stereotactic radiosurgery alone with stereotactic radiosurgery followed by whole-brain radiotherapy. They want to determine whether adding whole-brain radiotherapy provides any benefit in terms of preventing additional metastases and how whole-brain radiotherapy affects patient quality of life and cognition.
"Upfront whole-brain radiotherapy is a proven method of preventing brain metastases, but its benefits may come at the cost of reduced cognitive abilities and quality of life," said Dr. Brown. "So the role of whole-brain radiotherapy in this setting remains controversial. With this trial, we hope to define its use in the treatment of brain metastases following radiosurgery.
"One recent development that we're excited about is a trial amendment that allows the use of pinless head systems to deliver the radiosurgery, which will open the study up to many more treatment centers."
Who Can Join This Trial
Researchers will enroll 528 patients age 18 and older with one to three brain metastases from cancer elsewhere in the body. See the list of eligibility criteria at http://cancer.gov/clinicaltrials/NCCTG-N0574.
Study Sites and Contact Information
Study sites in the United States are recruiting patients for this trial. See the list of study contacts at http://cancer.gov/clinicaltrials/NCCTG-N0574 or call NCI's Cancer Information Service at 1-800-4-CANCER (1-800-422-6237) for more information. The toll-free call is confidential.
An archive of "Featured Clinical Trial" columns is available at http://cancer.gov/clinicaltrials/ft-all-featured-trials. |
 |
 |
If Memory Serves...
Several months before the National Cancer Institute Act was passed by Congress and signed by President Roosevelt, Fortune magazine had published an article, "Cancer: the Great Darkness," that pointed out the small amount of money that was being spent for cancer research. (Read more 34)
For more information about the birth of NCI, go to http://www.cancer.gov/
aboutnci/ncia.
Workshop on Phase 0 Trials Slated for September
On September 5, NCI's Division of Cancer Treatment and Diagnosis 35 will sponsor a workshop on "Phase 0 Trials in Oncologic Drug Development" in the Natcher Conference Center on the NIH campus in Bethesda, MD. The goal of the workshop is to define the Phase 0 effort and its potential value, lay out what is needed to perform phase 0 trials, propose ways to evaluate the Phase 0 effort, and determine future research directions for the next 2 to 3 years. Registration and other information can be found at http://www.blsmeetings.net/phase0workshop/.
NCI Director to Open Understanding NCI Teleconference Series
NCI Director Dr. John E. Niederhuber will present an "Update for the Advocacy Community" on September 12 from 1:00-2:00 p.m., EDT, to open the fall "Understanding NCI" teleconference series. Doug Ulman, chair of the NCI Director's Consumer Liaison Group 36, will address the role advocates play at NCI.
NCI's Office of Liaison Activities 37 (OLA) sponsors the teleconference series, which is intended to inform the advocacy community and the general public about NCI research and scientific initiatives, as well as feature an advocate's perspective on the topic. Callers are encouraged to participate in a discussion with Dr. Niederhuber during the question and answer session.
The teleconference can be accessed toll free within the U.S. at 800-857-6584; the passcode is NCI. Toll-free playback will be available through October 12 at 866-443-8027.
For more information on "Understanding NCI," visit http://ola.cancer.gov/activities/teleconferences or contact OLA at 301-594-3194 or liaison@od.nci.nih.gov.
Breast Cancer Guidelines Now Available in Spanish
The Breast Health Global Initiative's Guidelines for International Breast Health and Cancer Control are now available in Spanish. The guidelines were published in English in 2006 and address resources for early detection and access to care, diagnosis and pathology, treatment and allocation of resources, and health systems and public policy to reduce the burden of breast cancer in low- and middle-income countries (LMCs).
The Spanish-language guidelines are intended to help policymakers and health care providers in Spanish-speaking LMCs improve breast cancer outcomes through evidence-based, economically feasible, and culturally appropriate practices. Russian, Chinese, and Arabic versions of the guidelines are expected soon. The guidelines can be found at http://www.paho.org/English/DD/PIN/pr070727.htm.
|
|
 |
 |

NCI Support Helps Researchers Recover from Hurricane Katrina
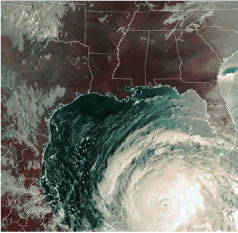 Two years ago, when Hurricane Katrina slammed into the Gulf Coast, the whole world saw the devastation to New Orleans and the surrounding region - the submerged streets, the flooded houses, the gaping levees. Less obvious, however, was the destruction of laboratories where hundreds of researchers were carrying out investigations into cancer and other diseases.
Two years ago, when Hurricane Katrina slammed into the Gulf Coast, the whole world saw the devastation to New Orleans and the surrounding region - the submerged streets, the flooded houses, the gaping levees. Less obvious, however, was the destruction of laboratories where hundreds of researchers were carrying out investigations into cancer and other diseases.
"Right after Hurricane Katrina, NCI organized a rapid response 38 to try to place dislocated investigators and provide disaster relief supplements to allow investigators to rebuild their labs as quickly as possible," says Stephen White of NCI's Division of Cancer Biology 39 and the Hurricane Katrina Relief 40 coordinator for the Institute. "This was complicated by damaged communications lines and the displacement of many researchers and their laboratory employees. But, within a couple of weeks, NCI program directors had managed to locate and contact nearly all of our grantees and offer help and support."
Some researchers were hit harder than others, depending on their location. Some institutions lost electricity and suffered structural damage; the contents of freezers and incubators were rendered unusable. Other labs were completely flooded, resulting in the loss of equipment, cell lines, tissue samples, and data. In some cases, investigators were not able to enter their labs for 3 to 6 months because of mold and other contamination left by the storm.
NCI initially asked grantees to submit brief requests for relief funds as soon as they were able to determine the extent of losses and estimate immediate needs. Relief funding supported the replacement of supplies, reagents, chemicals, assay kits, lab ware, cell lines, animals, small equipment replacement and repair, computers and software, contracts for samples and databases, and patient enrollment costs.
NCI also established a policy on how to respond to requests and allocate resources. An award of $1 million was made to the Louisiana Cancer Research Consortium and distributed equally between the Tulane University and the LSU Cancer Centers to support the replacement of lost equipment. Investigators holding grants with multiple years remaining were given initial supplements to recover immediate losses to their labs and the opportunity to request project extensions at the end of their project period, if needed.
"Within 6 months after the hurricane, we had heard from and responded to nearly all of our affected investigators," continues Mr. White. "In FY06 we made 29 relief supplements to active grants totaling about $4 million. For FY06 and FY07 combined, NCI has provided 37 relief supplements totaling $4.95 million."
NCI provided relief funds to grantees at Tulane University, LSU Health Science Center, University of South Alabama, Loyola University New Orleans, and Ochsner Clinic Foundation, and awarded a supplement to a contract with the Louisiana Tumor Registry.
Several grantees moved to new institutions in other states. NCI expedited transfers to these institutions and ensured that relief funds were distributed as quickly as possible.
"It's impossible to calculate the total damage resulting from Katrina," says Mr. White. "I'd say that many investigators lost at least a full year of research. The loss of basic and clinical data was phenomenal, but most of the investigators were able to resume their work either in New Orleans or in another city. I'm glad that NCI Director Dr. John Niederhuber, the Executive Committee, and other NCI staff were able to help them to do that and continue to support the recovery effort."
By Barbara Cire |
 |
|
Table of Links
| 1 | http://www.cancer.gov/Templates/db_alpha.aspx?CdrID=270732 |
| 2 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_082107/page2 |
| 3 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_082107/page3 |
| 4 | http://dccps.nci.nih.gov/ocs |
| 5 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_110805/page2 |
| 6 | http://dccps.nci.nih.gov |
| 7 | http://www.ahrq.gov |
| 8 | http://appliedresearch.cancer.gov |
| 9 | http://www.cancer.gov/clinicaltrials/NCI-04-C-N191 |
| 10 | http://dceg.cancer.gov |
| 11 | http://dceg.cancer.gov/hreb/research/cervical-hpv |
| 12 | http://www.cancer.gov/cancertopics/druginfo/doxorubicin-hydrochloride-liposome |
| 13 | http://www.cancer.gov/cancertopics/druginfo/bortezomib |
| 14 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_062805/page5#b |
| 15 | http://www.cancer.gov/cancertopics/druginfo/lenalidomide |
| 16 | http://www.cancer.gov/clinicaltrials/results/lenalidomide0606 |
| 17 | http://www.cancer.gov/search/ViewClinicalTrials.aspx?cdrid=420968&version=H
ealthProfessional&protocolsearchid=3538044 |
| 18 | http://www.calgb.org |
| 19 | http://www.cancer.gov/cancertopics/druginfo/IrinotecanHydrochloride |
| 20 | http://www.cancer.gov/clinicaltrials/CLB-89803 |
| 21 | http://prevention.cancer.gov/programs-resources/groups/cb/programs/glycome |
| 22 | http://prevention.cancer.gov |
| 23 | http://edrn.nci.nih.gov |
| 24 | http://www.functionalglycomics.org/static/index.shtml |
| 25 | http://www.ncrr.nih.gov/biomedical_technology/biomedical_technology_research_re
sources/technology_for_systems_biology/glycomics.asp |
| 26 | http://prevention.cancer.gov/programs-resources/groups/cb |
| 27 | http://deainfo.nci.nih.gov/advisory/pcp/pcp.htm |
| 28 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_010907/page6 |
| 29 | http://content.nejm.org/cgi/content/full/357/5/509 |
| 30 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_050107/page2 |
| 31 | http://breastscreening.cancer.gov |
| 32 | http://cisnet.cancer.gov |
| 33 | http://www.nhlbi.nih.gov/whi/estro_pro.htm |
| 34 | http://www.cancer.gov/aboutnci/if-memory-serves |
| 35 | http://dctd.cancer.gov |
| 36 | http://dclg.cancer.gov |
| 37 | http://ola.cancer.gov |
| 38 | http://www.cancer.gov/ncicancerbulletin/NCI_Cancer_Bulletin_090605/page2 |
| 39 | http://dcb.nci.nih.gov |
| 40 | http://www.cancer.gov/hurricane-response-efforts |
|
 |