CBER Vision Newsletter
Special Commemorative Issue
July 2002

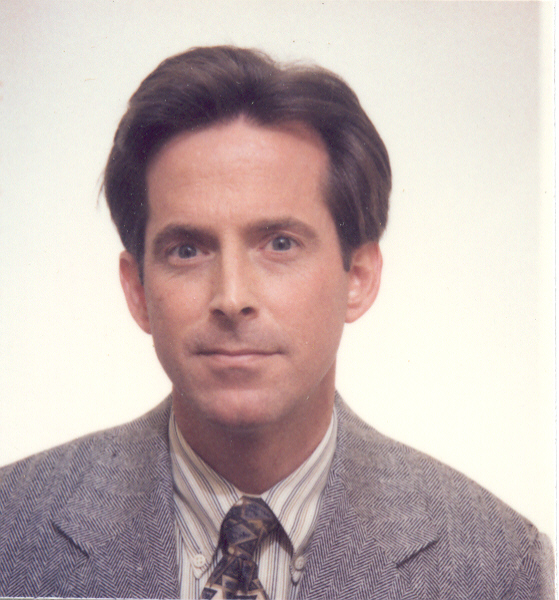
A Message from the Center Director

The Center for Biologics Evaluation and Research (CBER) is witnessing an event of great historic significance, both for our Center and FDA, and for the general public. On July 1, 2002, CBER commemorates passage of the 1902 Biologics Control Act (the Act) and 100 years of biologics regulation. The Act gave what is now known as CBER the authority to regulate biological products, and the responsibility to ensure their safety for the American public. Since passage of the Act, CBER has established a proud record of regulatory stewardship and research accomplishments. CBER's tradition of integrating strong science with innovative regulation has enhanced its ability to protect the public health, and has led to safer and more effective biological products.
Several activities and events have been planned to help us commemorate passage of the Act, and to honor our rich history of research, regulation and public service. By now, all of you should have received a Centennial mug and other commemorative items, such as pens and bookmarks. You may have watched our commemorative videotape, which captures the beginning of biologics regulation in 1901, with "Jim the horse," and ends with current discoveries and challenges for CBER. Presently, we are preparing a Centennial book that will walk us through 100 years of accomplishments in biomedical research and the regulation of biological products. Each of you will receive a copy of the Centennial book which will be used for various outreach activities to tell this important story. In the meantime, please check CBER's web site for an abbreviated on-line version of the book. An upcoming FDA Consumer also will publish an article about the history of CBER.
I am delighted to tell you that, as part of our commemorative activities this summer, the Smithsonian National Museum of American History will exhibit key artifacts from CBER's history. FDA historian John P. Swann, PhD, and others have worked hard to make this happen. I urge you to visit the Museum and have a look at these objects from our past.
Also, in recognition of our legacy of strong scientific research, on September 23-24, we will hold a scientific symposium at Natcher Auditorium on the NIH Campus. Details are included in this isssue of CBER Vision. I encourage all CBER staff to attend this important event.
Today, I invite you to read this Special Commemorative Edition of CBER Vision, which highlights some key research contributions made by CBER scientists over the last 100 years and, I believe, illustrates how science and innovative regulation go hand in hand. You may wish to share this issue with your family and friends. As you read the following pages, imagine yourself back in time, working in one of CBER's predecessor agencies alongside some of the most highly-respected scientists of the day. Maybe you have just a microscope, some culture plates, flasks and beakers, and a few chemical reagents, trying to understand the biological basis for disease and immunity. Perhaps you are working on research toward a vaccine for the numerous infectious diseases that were rampant at the time, or working to make blood and blood derivatives clean and safe from blood-borne pathogens. Imagine the pace of scientific research and regulation back then, and how work was accomplished with whatever scientific, technological, financial and other means were available. Despite limitations, much was accomplished. In some areas breakthroughs occurred; in others, the groundwork was laid for future discoveries. Think about where we were then, and where we are now-how our knowledge has grown, how our technological capabilities have expanded, and how our investment in biomedical research and review over the years has led to stunning discoveries and the availability of new medicines. We can all take much pride in working for such an organization as CBER.
I am very proud to be a part of CBER's legacy and invite you to join me on this historic journey into the past. And I look forward to facing future challenges and experiencing exciting research and regulatory opportunities together, as we build upon 100 years of regulating biological products and protecting the public health.
Kathryn C. Zoon, PhD

Message From The FDA Historian
The emergence of biological treatments in the late nineteenth century finally provided cures for diphtheria and eventually other serious diseases that had long plagued humanity. However, since the treatments consisted of processing the by-products of pathogenic organisms and then injecting them directly into the body, the potential for disaster was considerable. And unfortunately, it was realized in St. Louis in 1901, when thirteen children died after receiving diphtheria antitoxin that had been accidentally contaminated with tetanus. Around the same time, nine children in Camden, New Jersey, died from tainted smallpox vaccine.
The risks were laid bare before the legislative branch by District of Columbia Health Officer W. C. Woodward, who informed the House of Representatives why it was so important to secure pure biological treatments: they were introduced directly into the circulation; once administered they were beyond recall; and if the first dose turned out to be worthless, the loss of time could easily cost the life of the patient. "The manner in which these substances are produced and marketed," Woodward warned his audience, "renders it impossible to exercise efficient control over them by any system of inspection which takes cognizance only of the finished product. Efforts to insure their purity must be directed to the establishments where such products are manufactured."
Introduced in the House on April 5, 1902, the Biologics Control Act was passed by Congress with little debate, less than thirteen weeks later on July 1, 1902. By comparison, the 1906 Food and Drugs Act took 25 years after the first bill was introduced, though the latter certainly covered considerably more hotly-contested territory. But perhaps the most fascinating element of the 1902 law, especially considering the evolution and expansion of biological therapeutics, is that it has remained more or less intact over the past century. This law, the first of its kind to regulate the manufacture of therapeutic products since the short-lived 1813 Vaccine Act, charged the federal government to marshal the necessary science to establish standards for and oversight of biologics production.
This marvelous act will be recognized through several important educational venues over the coming months, including a well-researched monograph, a video that takes advantage of the rich visual legacy left by CBER and its predecessors, a symposium on biologics regulation, an article in FDA Consumer and a case exhibit at the Smithsonian Institution's National Museum of American History. CBER is to be commended for conceiving and developing this broad program to educate the public, and to remind FDAers of why we're here, and why the public health is better protected because of the 1902 Biologics Control Act.
John P. Swann, Ph. D.
FDA Historian

THE EARLY YEARS OF BIOLOGICS DEVELOPMENT AND REGULATION
The Public Health Service Hygienic Laboratory
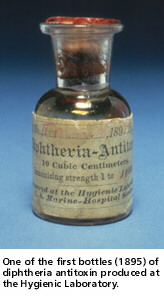
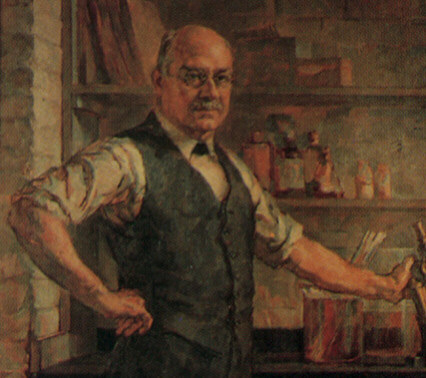 The Marine Health Service (MHS), the original public health agency, was established in 1798 to provide hospital care for merchant seamen. It also protected port cities against diseases such as smallpox, cholera and yellow fever. Joseph Kinyoun was a young MHS medical officer who toured the research centers of Europe to learn the latest techniques for controlling infectious diseases. Determined to apply his new-found knowledge to improving public health in the United States, he established one of the country's first bacteriological laboratories in 1887 in the MHS Hospital on Staten Island, New York. This one-room "Laboratory of Hygiene," with Kinyoun as director, was the beginning of medical laboratory research in the U.S. Public Health Service. In 1891, the Laboratory of Hygiene was moved to Washington, D.C. and renamed the "Hygienic Laboratory." Soon after, Kinyoun again visited Europe and, at the Pasteur Institute in Paris, learned the procedure for preparing diphtheria antitoxin. On returning to the United States, he prepared an antitoxin serum, both to be used by the MHS and for demonstration to representatives of local and state health boards. In a report to the U.S. Surgeon General in 1895, Kinyoun noted that all serum intended for sale should be made and tested by competent and disinterested persons, making an early plea for the establishment of a regulatory service.
The Marine Health Service (MHS), the original public health agency, was established in 1798 to provide hospital care for merchant seamen. It also protected port cities against diseases such as smallpox, cholera and yellow fever. Joseph Kinyoun was a young MHS medical officer who toured the research centers of Europe to learn the latest techniques for controlling infectious diseases. Determined to apply his new-found knowledge to improving public health in the United States, he established one of the country's first bacteriological laboratories in 1887 in the MHS Hospital on Staten Island, New York. This one-room "Laboratory of Hygiene," with Kinyoun as director, was the beginning of medical laboratory research in the U.S. Public Health Service. In 1891, the Laboratory of Hygiene was moved to Washington, D.C. and renamed the "Hygienic Laboratory." Soon after, Kinyoun again visited Europe and, at the Pasteur Institute in Paris, learned the procedure for preparing diphtheria antitoxin. On returning to the United States, he prepared an antitoxin serum, both to be used by the MHS and for demonstration to representatives of local and state health boards. In a report to the U.S. Surgeon General in 1895, Kinyoun noted that all serum intended for sale should be made and tested by competent and disinterested persons, making an early plea for the establishment of a regulatory service.
Beginning in 1899 under a new director Milton Rosenau, the Hygienic Laboratory expanded into a research organization with divisions of chemistry, bacteriology and pathology, zoology and pharmacology. Recognizing its importance, Congress authorized $35,000 in 1901 for construction of a new building, in which the Laboratory could investigate "infectious and contagious diseases and matters pertaining to the public health." The Hygienic Laboratory ultimately evolved into the National Institutes of Health.

FROM THE LABORATORY OF HYGIENE TO CBER
The regulation of biologics and the research necessary to support such regulation was delegated to the U.S. Treasury Department's Hygienic Laboratory of the Public Health and Marine Hospital Service, under the provisions of the Biologics Control Act of 1902. As the Hygienic Laboratory evolved into the CBER of today, its name also evolved to reflect changing responsibilities.
| Year |
Existing Organization |
| 1887 |
Laboratory of Hygiene of the Marine Health Service (MHS) |
| 1891 |
Laboratory of Hygiene renamed Hygienic Laboratory, still of the MHS |
| 1902 |
Hygienic Laboratory of the Public Health and Marine Hospital Service (PH-MHS) |
| 1930 |
Hygienic Laboratory renamed National Institute of Health |
| 1937 |
Division of Biologics Control (DBC) formed within National Institute of Health (NIH) |
| 1944 |
DBC renamed Laboratory of Biologics Control (LBC) |
| 1948 |
LBC incorporated into National Microbiological Institute (NMI), NIH |
| 1955 |
LBC becomes Division of Biologics Standards (DBS), an independent entity within NIH; NMI renamed the National Institute of Allergy and Infectious Diseases |
| 1972 |
DBS transferred from NIH to FDA; becomes Bureau of Biologics (BoB) |
| 1982 |
BoB merged with Bureau of Drugs to form National Center for Drugs and Biologics (NCDB) |
| 1983 |
Biologics component of NCDB renamed Office of Biologics Research and Review (OBRR) within Center for Drugs and Biologics (CDB) |
| 1988 |
CDB separated into two Centers; Center for Biologics Evaluation and Research (CBER) (formerly OBRR) and Center for Drug Evaluation and Research (CDER) |

CBER LEADERSHIP
Between 1887 and today, biologics regulation was led by the following directors:
Joseph J. Kinyoun, 1887-1899
Milton J. Rosenau, 1899-1909
John F. Anderson, 1909-1915
George W. McCoy, 1915-1937
Walter T. Harrison, 1937-1940
Milton V. Veldee, 1940-1949
William G. Workman, 1949-1955
Roderick Murray, 1955-1972
Harry M. Meyer, Jr., 1972-1987
Paul D. Parkman, 1987-1991
Gerald V. Quinnan, Jr., 1991-1992 (Acting)
Kathryn C. Zoon, 1992-present

HOW IT ALL BEGAN
The St. Louis Tetanus Epidemic
 Diphtheria antitoxin was a formidable new weapon in the fight against diphtheria-a dangerous infectious disease. But without proper standards to ensure its potency and purity, the antitoxin could be harmful instead of beneficial. Medical workers and the public expressed concern about the poor supervision of antitoxin production and the lack of inspection and testing of the final product. Even though many believed that federal oversight was necessary, no action was taken until a tragedy occurred. In 1901, when a serious diphtheria epidemic swept St. Louis, Missouri, victims of the disease were given antitoxin serum prepared from the blood of horses. In late October, 5-year-old Veronica Neill was admitted to the city hospital and received two shots of diphtheria antitoxin. Several days later, on October 26, she died from tetanus, a different infectious disease. Her doctor notified the St. Louis Health Commissioner that her death likely was caused by tetanus-contaminated antitoxin prepared by the city's Health Department; distribution of the antitoxin was stopped immediately. An investigation uncovered that a horse named Jim, which had provided diphtheria antitoxin for 3 years, had contracted tetanus and had been killed. The contaminated serum from this horse should have been destroyed, but was not. Instead, it was accidentally bottled and issued to doctors to use in treating diphtheria patients. Thirteen children died from tetanus as a result of receiving this serum. Although the St. Louis disaster was the worst, it was not the only such incident. Also in the fall of 1901, nine children in Camden, New Jersey, died from tetanus as a result of receiving contaminated smallpox vaccine.
Diphtheria antitoxin was a formidable new weapon in the fight against diphtheria-a dangerous infectious disease. But without proper standards to ensure its potency and purity, the antitoxin could be harmful instead of beneficial. Medical workers and the public expressed concern about the poor supervision of antitoxin production and the lack of inspection and testing of the final product. Even though many believed that federal oversight was necessary, no action was taken until a tragedy occurred. In 1901, when a serious diphtheria epidemic swept St. Louis, Missouri, victims of the disease were given antitoxin serum prepared from the blood of horses. In late October, 5-year-old Veronica Neill was admitted to the city hospital and received two shots of diphtheria antitoxin. Several days later, on October 26, she died from tetanus, a different infectious disease. Her doctor notified the St. Louis Health Commissioner that her death likely was caused by tetanus-contaminated antitoxin prepared by the city's Health Department; distribution of the antitoxin was stopped immediately. An investigation uncovered that a horse named Jim, which had provided diphtheria antitoxin for 3 years, had contracted tetanus and had been killed. The contaminated serum from this horse should have been destroyed, but was not. Instead, it was accidentally bottled and issued to doctors to use in treating diphtheria patients. Thirteen children died from tetanus as a result of receiving this serum. Although the St. Louis disaster was the worst, it was not the only such incident. Also in the fall of 1901, nine children in Camden, New Jersey, died from tetanus as a result of receiving contaminated smallpox vaccine.

CONGRESS TAKES ACTION
The Biologics Control Act (1902)
As a result of the St. Louis tetanus outbreak and similar but smaller occurrences of contaminated smallpox vaccine and diphtheria antitoxin, Congress passed the Biologics Control Act on July 1, 1902, only a few months after it was proposed-with virtually no debate or opposition. This Act authorized the Hygienic Laboratory of the Public Health and Marine Hospital Service to issue regulations that governed all aspects of commercial production of vaccines, serums, toxins, and antitoxins and similar products with the objective of ensuring their safety, purity, and potency. The Laboratory issued its first series of regulations in 1903 and additional regulations in 1909 and thereafter, to tighten control over biologics production. Further, in 1934, the Hygienic Laboratory-renamed the National Institute of Health in 1930 by the Ransdell Act-issued a regulation stating that licenses to manufacture new biologics would not be granted without evidence that the products were effective. Overall, the basic provisions of the 1902 Act served the nation well throughout the 20th century.
Implementing the Biologics Control Act
Between 1903 and 1907, the Hygienic Laboratory established standards and issued licenses to pharmaceutical firms for making smallpox and rabies vaccines, diphtheria and tetanus antitoxins, and various antibacterial antiserums. After 1907, many firms also started producing antibacterial vaccines. Beginning in 1917, the Laboratory issued licenses for making toxin products that provided immunity, including: diphtheria toxin mixed with antitoxin [1917]; scarlet fever toxin [1925]; diphtheria toxoid [1926]; tetanus toxoid [1933]; additional antitoxins such as botulinum [1921]; scarlet fever streptococcus [1925]; gonococcus [1927]; perfringens and other gas gangrene-causing bacteria [1931-1939]; and human bacterial and viral antisera for pertussis, poliomyelitis and mumps [1939-1941].
Throughout these early years, as is still true today, the 1902 Act stimulated scientific research by the Hygienic Laboratory to improve existing biologics and to find better ways of producing them, to develop standards for new products and to find immunizing agents for all infectious diseases. Laboratory staff made numerous significant contributions that advanced the state of the science. For instance, staff established the standards for botulinus antitoxins and for gas gangrene antitoxins, developed a practical method for preparing serums to diagnose various types of pneumonia, and developed an improved meningitis serum potency test, as well as a serum specific for different types of meningitis bacteria.

 MARGARET PITTMAN
MARGARET PITTMAN
"A WOMAN SCIENTIST AHEAD OF HER TIME"
Margaret Pittman was considered a "world-renowned expert on the subject of pertussis," and "a woman scientist ahead of her time" according to Linda Smallwood, Associate Director for Policy in CBER's Office of Blood Research and Review.
Pioneering Work on Haemophilus influenzae
Haemophilus influenzae bacteria cause infections in humans ranging from asymptomatic respiratory infections to serious diseases such as meningitis. Children are particularly susceptible to this pathogen. In the early 1930s, Margaret Pittman-who retired from the Division of Biologics Standards in 1971 after 35 years of making significant scientific contributions-was doing postgraduate work at the Rockefeller Institute (RI) for Medical Research. While at the RI, she conducted pioneering research on the microbiology and immunology of infections caused by H. influenzae. She found that these bacteria existed in two forms-encapsulated (with a special coating) and unencapsulated. The unencapsulated bacteria, which generally caused either no illness at all or relatively mild respiratory infections and mucosal infections (such as sinusitis), frequently were found in the upper respiratory tract of adults. Pittman discovered six different varieties of the encapsulated H. influenzae organism and observed that only the type b encapsulated variety seemed to cause serious diseases in children. Pittman's work formed the basis for development of an antiserum for invasive H. influenzae type b disease. The antiserum was the first effective therapy for this potentially fatal infection. The 1985 licensing of a polysaccharide vaccine for H. influenzae type b for use in preschool-aged children was a long-term outcome of Pittman's early research on this pathogen. Research by John Robbins and colleagues, conducted at the Bureau of Biologics in the 1980s, led to development and licensing in 1987 of a polysaccharide-protein conjugate vaccine for H. influenzae type b that provided stronger protection than the simpler polysaccharide vaccine. In 1996, Robbins received the Albert Lasker Award for Clinical Medical Research for his work on the conjugate vaccine.

From left, Top row: "Hut" Hudson; Russell P. Miller; Edward Garlock; Aneas P. Collins; Ben T. Sockrider; Thomas F. Probey
From left, Second row: Glen Hefner; L.J. Bender; Sadie A. Carlin; Dr. Sarah E. Stewart; Marguerite Lyons; Gilbert E. Beard; Robert Forkish.
From left, Bottom row: Dr. Karl Habel; Dr. Margaret Pittman; Dr. William G. Workman; Dr. W. T. Harrison; Dr. Sara E. Branham; Dr. V. J. Dorsett; Dr. Bernice Eddy.
Testing the Potency of Pertussis Vaccine
Pertussis, also known as "whooping cough," is a potentially deadly respiratory infection that most commonly affects children. The illness can last for weeks and is characterized by a severe cough; some infected children are left with permanent neurological damage, and some die. Although scientists had been trying to develop a pertussis vaccine since the early 1900s, the difficulty in assessing its potency was a major stumbling block. Scientists had not been able to develop a potency test for pertussis vaccine, because they were unable to establish pertussis infection in a laboratory animal. In 1944, Margaret Pittman found that she could infect mice with pertussis by injecting pertussis bacteria into the mouse brain. She then used this knowledge to test the potency of a pertussis vaccine. Dr. Pittman developed a vaccine potency standard based on a "50 percent dose"-that is, the dose of vaccine that would result in the survival of 50 percent of mice infected with a certain number of pertussis bacteria. On January 1, 1949, manufacturers began using this "mouse protection test" for determining pertussis vaccine potency. Further, to make vaccine preparation easier, Pittman prepared an opacity standard for pertussis vaccine that could be used to estimate the number of bacteria in a vaccine, instead of laboriously counting the bacteria under a microscope.
Pyrogenicity Testing for Blood Products
In the early 1940s, the use of intravenous therapy using blood and blood products increased significantly because of the many wounded soldiers who needed treatment during World War II. Occasionally, pyrogenicity (fever reactions) occurred after this therapy. To investigate pyrogenicity in blood products, Margaret Pittman and Thomas Probey, at the Division of Biologics Control, studied the pyrogenicity of 28 types of bacteria isolated from blood plasma by using a rabbit pyrogen test. Pittman and Probey found that all of the bacteria were capable of producing fever but, because the effects of various types of bacteria differed widely, simply measuring the number of bacteria in plasma could not predict the pyrogenicity of the plasma. Based on these and other findings, Pittman and Probey collaborated with manufacturers to help define production techniques that resulted in pyrogen-free blood products.

World War II and the Postwar Period
Standards for Essential Blood Products
During World War II, the Division of Biologics Control established standards for manufacturing plasma and albumin, and supervised their production in commercial establishments. The Division issued licenses for several blood fractionation products, including albumin, globulins useful for blood grouping, immune globulins (called gamma globulin at the time), fibrin foam and thrombin (clotting agents used to control bleeding during surgery), and fibrin film (used in surgery as a substitute for the outermost membrane covering the brain).
Elimination of Jaundice Virus From Blood Plasma
During World War II, the demand for human blood plasma for America's military personnel was huge. The Division of Biologics Control (DBC) had responsibility for setting up safety standards and overseeing the manufacture of blood products by commercial laboratories. Blood plasma, blood serum and serum albumin were among these products. Although blood products without doubt saved many lives, they were found to have potential hazards. In 1942, 28,000 military personnel injected with a yellow fever vaccine prepared with human blood serum developed jaundice. One hundred people died. There was a strong possibility that some unknown factor in human blood was causing the disease. Thus, in the middle of wartime production of blood plasma on a massive scale, the DBC was faced with the urgent need to find a way to guarantee its safety.
By conducting careful research, three DBC scientists - John Oliphant, Alexander Gilliam and Carl Larson - showed that people who were inoculated with blood serum from jaundice-infected patients also developed jaundice, but that the disease was not spread by personal contact. The cause of the jaundice appeared to be an unidentified virus. The yellow fever vaccine likely had been contaminated by the blood serum of donors who either had unrecognized disease or were simply carriers of the virus. Because blood plasma from individual donors was generally "pooled," one donor infected with the virus could contaminate an entire batch of plasma or serum. The DBC scientists found that the jaundice-causing virus was heat resistant; also, it was too small to be removed from blood products by using filters. Next, Oliphant, working with biophysicist Alexander Hollaender, conducted research in which ultraviolet radiation appeared to kill the virus in blood serum and plasma. In April 1949, regulations were issued by the Laboratory of Biologics Control (LBC) requiring that human blood plasma and serum be irradiated. Studies conducted by Oliphant and Roderick Murray in the LBC in the early 1950s, however, showed that some jaundice, renamed hepatitis, cases were still being transmitted through transfusions. In later years, researchers identified both hepatitis B virus and hepatitis C virus as possible contaminants in blood products. Today, all blood products are tested for hepatitis B and C to prevent contaminated blood from being used for transfusions or for the manufacture of blood products.
Improving Existing Biologics
During the war years, all U.S. military personnel received shots for tetanus, typhoid fever and smallpox. Also, tremendous quantities of vaccines for typhus, yellow fever, cholera, diphtheria and plague, as well as antitoxins and serums for various other diseases, had to be manufactured to immunize those who served in areas where these diseases occur. The Division of Biologics Control had to be certain that the requirements for each product helped ensure that it would be safe, pure and effective against the disease. In some cases, this meant improving existing products by refining standards, developing better potency tests or finding new ways to purify a product. For instance, in 1941, the Division licensed a new vaccine for typhus-a disease caused by a kind of bacteria called rickettsia. The vaccine was given to U.S. military personnel in southern Europe and North Africa. Typhus had caused devastating epidemics in World War I, but only 64 cases occurred among U.S. military personnel in World War II.
Early Research on Influenza Vaccine
The influenza (flu) epidemic of 1918-19 caused an estimated 20 million deaths worldwide. There was little progress, however, in flu research until a flu virus called Type A was finally isolated in England in 1933 and in the United States in 1934. This advance came from the use of embryonated chicken eggs for recovering the virus-a new breakthrough that allowed the preparation of vaccines. The most common varieties of flu are caused by the Type A flu virus. Researchers discovered a second kind of flu virus, Type B, in the 1940 flu epidemic. Flu vaccines made in the late 1930s and early 1940s were not always effective, because no accurate test was available to measure their potency. Even though flu vaccine was not yet licensed for marketing, commercial laboratories produced large amounts of flu vaccine for the U.S. Army during World War II. Because this vaccine was of variable quality, Bernice Eddy, a scientist at the Division of Biologics Control, concentrated on developing the first reliable potency test for flu vaccine, so that manufacturers could make a uniform product with the desired effectiveness. The vaccine produced during World War II was effective against both Type A and Type B influenza viruses. The flu vaccine was licensed in 1945 and, after World War II, it was also used for civilians. Producing effective flu vaccine is complicated because the Type A virus has a number of subtypes and, as new subtypes appear and circulate in the human population, vaccine formulations must be changed to protect people against the new subtypes. Today's flu vaccines are 70 to 90 percent effective in reducing a person's chances of getting the flu.

A DEFINING EVENT
The War on Polio and The Cutter Incident
 U.S. President Franklin D. Roosevelt, who suffered the paralytic effects of poliomyelitis, also called polio or infantile paralysis, initiated a "War on Polio" during his administration. Concerted efforts were directed toward finding a vaccine for this incurable, infectious disease. Polio virus was successfully grown in tissue cell culture in 1949, and live polio virus vaccine produced from virus grown by this method was successfully tested in humans in 1950. Jonas Salk began his polio vaccine research in 1951. By 1954, a large field trial of vaccine developed by Salk, using inactivated (killed) poliovirus, was conducted in American children. Trial data showed the vaccine to be both safe and effective. On April 12, 1955, the Laboratory of Biologics Control issued licenses for commercial manufacture of polio vaccine to six companies that had already been producing vaccine for the field trials. Written protocols for vaccine production and safety testing, submitted to the Laboratory of Biologics Control by the companies, were the only legal requirement for licensing. Over the next two weeks, approximately 40 batches of manufactured vaccine were released by the government for distribution. Unexpectedly, on April 25, polio was reported in a vaccine recipient. One day later, five more cases were reported. All cases had received vaccine produced by Cutter Laboratories. On April 27, the Laboratory of Biologics Control requested that Cutter Laboratories recall all vaccine and the company did so immediately. On May 7, the Surgeon General recommended that all polio vaccinations be suspended pending inspection of each manufacturing facility and thorough review of the procedures for testing vaccine safety. The investigation found that live polio virus had survived in two batches of Cutter vaccine. In fact, Cutter Laboratories had discarded a number of other vaccine batches because live virus was present, but there was no requirement for them to report such problems. Overall, 260 cases of polio were attributed to Cutter vaccine; these included 94 vaccinees and 166 close contacts of vaccinees, with 192 cases being paralytic. Reappraisal of virus inactivation and safety testing procedures led to improved production techniques, and development of more sensitive and better-controlled testing methods to ensure consistently safe vaccine. Large-scale polio vaccinations resumed in the fall of 1955.
U.S. President Franklin D. Roosevelt, who suffered the paralytic effects of poliomyelitis, also called polio or infantile paralysis, initiated a "War on Polio" during his administration. Concerted efforts were directed toward finding a vaccine for this incurable, infectious disease. Polio virus was successfully grown in tissue cell culture in 1949, and live polio virus vaccine produced from virus grown by this method was successfully tested in humans in 1950. Jonas Salk began his polio vaccine research in 1951. By 1954, a large field trial of vaccine developed by Salk, using inactivated (killed) poliovirus, was conducted in American children. Trial data showed the vaccine to be both safe and effective. On April 12, 1955, the Laboratory of Biologics Control issued licenses for commercial manufacture of polio vaccine to six companies that had already been producing vaccine for the field trials. Written protocols for vaccine production and safety testing, submitted to the Laboratory of Biologics Control by the companies, were the only legal requirement for licensing. Over the next two weeks, approximately 40 batches of manufactured vaccine were released by the government for distribution. Unexpectedly, on April 25, polio was reported in a vaccine recipient. One day later, five more cases were reported. All cases had received vaccine produced by Cutter Laboratories. On April 27, the Laboratory of Biologics Control requested that Cutter Laboratories recall all vaccine and the company did so immediately. On May 7, the Surgeon General recommended that all polio vaccinations be suspended pending inspection of each manufacturing facility and thorough review of the procedures for testing vaccine safety. The investigation found that live polio virus had survived in two batches of Cutter vaccine. In fact, Cutter Laboratories had discarded a number of other vaccine batches because live virus was present, but there was no requirement for them to report such problems. Overall, 260 cases of polio were attributed to Cutter vaccine; these included 94 vaccinees and 166 close contacts of vaccinees, with 192 cases being paralytic. Reappraisal of virus inactivation and safety testing procedures led to improved production techniques, and development of more sensitive and better-controlled testing methods to ensure consistently safe vaccine. Large-scale polio vaccinations resumed in the fall of 1955.
The Cutter Incident was a defining moment in the history of vaccine manufacturing and government oversight of vaccines. It occurred because the rigorous safety precautions that were used in the field trials-which included repeating all vaccine safety tests in three different laboratories and confirming all manufacturers' ability to prepare consistently safe vaccine-were not required for the production of commercially-produced licensed vaccine. In addition, the protocols provided by the manufacturers did not provide enough information for safety evaluation.
In 1955, as a result of the Cutter Incident, the Laboratory of Biologics Control was raised to division status within NIH, to strengthen and expand its biologics control function. It became the Division of Biologics Standards, an independent entity composed of seven laboratories. The Division continued to oversee the control and release of biologics until 1972, when, in reaction to its not having instituted an effectiveness review equivalent to that performed for drugs, it was moved from NIH to FDA and renamed the Bureau of Biologics. The merger with FDA was logical, because a "biological product" under the 1944 PHS Act also falls within the jurisdiction of the 1938 FD&C Act. The appropriate provisions of both Acts were skillfully used to regulate biologics.

GROUNDBREAKING WORK
Protection Against Rubella
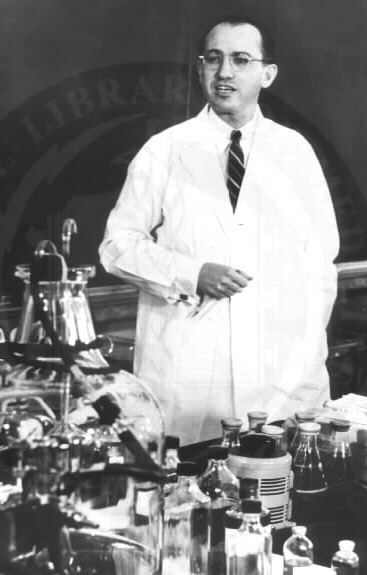
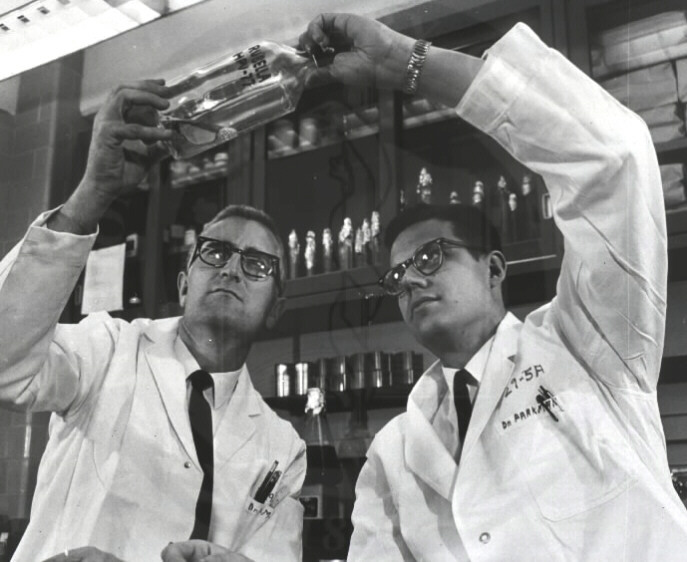 Rubella (German measles) is a usually mild viral disease that most often affects children and young adults, but it is a very dangerous disease for pregnant women, particularly during the first 3 months of pregnancy. The virus can be transmitted to the unborn child, resulting in abnormalities such as cataracts, deafness, heart defects and mental retardation. A global epidemic of rubella that started in Europe in 1962 spread to the United States in 1964, causing an estimated 12.5 million cases in this country and birth defects in about 20,000 children. The need for a rubella vaccine was clear and many in the scientific community were working on the problem. In 1963, Roderick Murray, MD, the founding Director of the Division of Biologics Standards (DBS) hired Paul Parkman, MD, who had discovered rubella virus while working at the Walter Reed Army Institute of Research, to start a rubella program. Dr. Parkman teamed with Harry Meyer, Jr., MD, already at DBS. By 1966, they were able to report that they had developed the first effective experimental vaccine for rubella. They had weakened the rubella virus by subjecting it to 77 passages in primary African green monkey kidney cell cultures over 2 years and then tested its effectiveness in rhesus monkeys. When the monkeys were inoculated with the weakened, live virus, none of them developed rubella or transmitted the disease to monkeys that had not been inoculated, and they were solidly protected against infection with the wild virus. Based on these results, Parkman and Meyer prepared a weakened, live vaccine for human testing and inoculated 34 children. None of the children developed rubella, nor did they transmit the virus to any of their 30 playmates who had not been inoculated. Parkman and Meyer made the weakened virus-the first successful experimental rubella vaccine-available to other scientists interested in rubella research. Based on their success, the first rubella vaccines were licensed in 1969. These vaccines, and the current vaccine that was approved a decade later, have been strikingly successful in controlling rubella. By 1988, there were only 225 reported cases of rubella in the United States.
Rubella (German measles) is a usually mild viral disease that most often affects children and young adults, but it is a very dangerous disease for pregnant women, particularly during the first 3 months of pregnancy. The virus can be transmitted to the unborn child, resulting in abnormalities such as cataracts, deafness, heart defects and mental retardation. A global epidemic of rubella that started in Europe in 1962 spread to the United States in 1964, causing an estimated 12.5 million cases in this country and birth defects in about 20,000 children. The need for a rubella vaccine was clear and many in the scientific community were working on the problem. In 1963, Roderick Murray, MD, the founding Director of the Division of Biologics Standards (DBS) hired Paul Parkman, MD, who had discovered rubella virus while working at the Walter Reed Army Institute of Research, to start a rubella program. Dr. Parkman teamed with Harry Meyer, Jr., MD, already at DBS. By 1966, they were able to report that they had developed the first effective experimental vaccine for rubella. They had weakened the rubella virus by subjecting it to 77 passages in primary African green monkey kidney cell cultures over 2 years and then tested its effectiveness in rhesus monkeys. When the monkeys were inoculated with the weakened, live virus, none of them developed rubella or transmitted the disease to monkeys that had not been inoculated, and they were solidly protected against infection with the wild virus. Based on these results, Parkman and Meyer prepared a weakened, live vaccine for human testing and inoculated 34 children. None of the children developed rubella, nor did they transmit the virus to any of their 30 playmates who had not been inoculated. Parkman and Meyer made the weakened virus-the first successful experimental rubella vaccine-available to other scientists interested in rubella research. Based on their success, the first rubella vaccines were licensed in 1969. These vaccines, and the current vaccine that was approved a decade later, have been strikingly successful in controlling rubella. By 1988, there were only 225 reported cases of rubella in the United States.
Ensuring Effectiveness of Allergenic Products
Allergenic products include allergen patch tests-diagnostic tests applied to the surface of the skin; and allergenic extracts-injectable products, made from natural substances, used to diagnose and treat allergic diseases such as "hay fever," food allergy and bee venom allergy. Very important research on allergenic products, particularly allergenic extracts, began in the 1970s in the Bureau of Biologics. As explained by Harold Baer, former Chief of the Laboratory of Allergenic Products, "Although there were hundreds of allergenic products, and they were injected probably into more people than any other product licensed by FDA, these were the only products for which there were no standards." To address this issue, Bureau scientists developed laboratory techniques for measuring the activity of allergenic extracts, linked these results to effectiveness of the extracts in humans, and established standards for the extracts that had to be met by manufacturers. A scientific review of the hundreds of allergenic extracts that were being marketed in the United States in the 1980s found that about 240 products had no allergenic activity. These ineffective products were gradually removed from the market over the course of a decade. Currently, there are 19 standardized allergenic extracts available for use.

CBER SCIENCE SYMPOSIUM
"SCIENCE AND THE REGULATION OF BIOLOGICS:
FROM A RICH HISTORY TO A CHALLENGING FUTURE"
SEPTEMBER 23, 2002
| 8:30 - 8:45 |
Introduction and Welcome |
Dr. Kathryn Zoon |
| 8:45 - 9:15 |
Harry Meyer, Jr., MD Lecture |
Dr. Paul Parkman |
| 9:15 - 9:40 |
CBER Centennial Video |
|
| 9:40 - 9:50 |
Remarks |
Dr. Lester Crawford (Invited) |
| 9:50 - 10:00 |
Remarks |
Secretary Tommy Thompson (Invited) |
| 10:00 - 10:20 |
Break |
|
| 10:20 - 10:50 |
International Biologics Issues |
Dr. Johannes Lower |
| 10:50 - 12:30 |
Issues in Blood Research |
Dr. Jay Epstein |
| |
"Raise the Standards" |
Dr. David Aronson |
| |
Topic to be Determined |
Dr. John Petricciani |
| |
"TSEs: BSE, CJD, vCDJ and the Blood Supply" |
Dr. David Asher |
| 12:30 - 1:45 |
Lunch |
|
| 1:45 -2:15 |
Remarks |
Dr. Ruth Kirschstein |
| 2:15 - 3:20 |
Issues in Vaccines Research |
Dr. Karen Midthun |
| |
History of Interaction between Industry and FDA |
Dr. Maurice Hilleman |
| |
Topic to be determined |
Dr. John Robbins |
| 3:20 - 3:40 |
Break |
|
| 3:40 - 4:10 |
"Methods for Development of Vaccine Characterization" |
Dr. Konstantin Chumakov |
| 4:15 |
Adjourn |
|
SEPTEMBER 24, 2002
| 8:30 - 8:45 |
Open and Welcome |
Dr. Kathryn Zoon |
| 8:45 - 9:15 |
New Efforts in Counter Bioterrorism |
Dr. Anthony Fauci |
| 9:15 - 10:20 |
Issues in Therapeutics Research |
Dr. Jay Siegel |
| |
"Past, Present and Future Perspectives on Immunology and Immune Therapies" |
Dr. Thomas Waldmann |
| |
Topic to be Determined |
Dr. French Anderson |
| 10:20 - 10:40 |
Break |
|
| 10:40 - 11:10 |
NCI Perspectives on Translational Medicine and New Technologies |
Dr. Carl Barrett |
| 11:10 - 11:40 |
Issues in Therapeutics Research/
Future Technology |
Dr. Emmanuel Petricoin/
Dr. Lance Liotta |
| 11:40 - 12:00 |
Future Challenges in Biologics |
Dr. Kathryn Zoon |
| Adjourn |
|

CBER's Recent Past and the Future
In the early 1980's, Human Immune Deficiency Virus (HIV) appeared and was found in the blood of infected people; thus, threatening the nation's blood supply. Transfusions became suspect. Improved screening tests for donated blood became necessary, and both CBER and the industry responded to the challenge. The first test kit to detect HIV in donated blood was licensed in 1985. Inspections of blood banks were increased to ensure compliance with strict screening and processing procedures.
Also in the 1980's, the human genome was being deciphered. The double helix is the DNA molecule in a human cell that contains genetic information. Understanding DNA allows researchers to manipulate genes to potentially cure inherited diseases. The discovery of recombinant DNA methods led the way to the development of biotechnology, and the approval of the first recombinant DNA vaccine, Hepatitis B (Recombinant), licensed in 1986.
The 1990's were witness to licensure of numerous biologics to treat infectious diseases, cancer and other serious illnesses. Additionally, the deciphering of the human genome was completed. Work continues in the areas of gene therapy, altering the genetic makeup of a cell by isolating a gene, and xenotransplantation, the transplantation of animal cells, tissue or organs into a human.
Today, the genomics revolution has scarcely begun. The study of gene structures is leading to potentially effective treatments for a variety of serious diseases and conditions including cancer, diabetes and heart disease. While the genome represents the information archive of the cell, it is the proteins that do all the work. They carry out cell function, underpin disease processes and ultimately dictate cellular growth and death. The main tool being used to study gene structure and proteins is microarray equipment which is capable of analyzing thousands of genes simultaneously. The focus is to develop genomic and proteomic tools to help in science-based decision making for product development. The joint CBER/NIH Proteomics Program offers molecular imaging of cells and blood, providing early diagnosis of disease and early warning of drug toxicity. Vaccines are being developed and modified as new discoveries reveal more about the human immune system. New allergenic products provide relief for those who suffer from allergies.
Infectious diseases, new and old, create an urgent demand for the hastened availability of new drugs. CBER's major challenge of the 21st century lies with the ability to expedite approval of biological products for use by the public while, at the same time, maintaining high levels of safety and quality. CBER's careful risk management of approved products in the market plays a crucial role in protecting the public health.
This is an exciting time in history where we are witness to the great biotechnology revolution. New biological therapies give credence to the expectation of longer and healthier lives. In the forefront of this revolution, CBER remains committed to the quest for better and safer products for a healthier tomorrow for all Americans and peoples throughout the world.

Test Yourself!
Now that you have read about CBER's history and some key accomplishments, take this short quiz and test your memory. All of the answers except one can be found within this issue of CBER Vision. Answers can be found at the bottom of this page.
- What was the name of the first U.S. government agency to regulate biological products?
- Hygienic Laboratory of the Public Health and Marine Hospital Service (PH-MHS)
- Laboratory of Hygiene of the Marine Health Service (MHS)
- National Institutes of Health
- National Fish and Wildlife Service
- What was the impetus for passage of the Biologics Control Act of 1902?
- outbreak of polio in a Lake Michigan summer camp
- deaths from hepatitis after plasma transfusions in Korean War
- deaths in St. Louis from tetanus contamination of diphtheria antitoxin
- outbreak of Salmonella poisoning at Popeye's in Palo Alto
- Who were the CBER scientists who developed the rubella vaccine?
- Sabin and Salk
- Parkman and Meyer
- Pittman and Probey
- Strunk and White
- CBER scientists conducted important research on post-transfusion jaundice caused by:
- Hepatitis A
- Hepatitis B
- Hantavirus
- Rickettsia tsu tsu gamushi
- What was the "Cutter Incident?"
- cases of polio contracted from live polio vaccine
- cases of influenza contracted from live flu vaccine
- cases of rubella from live rubella vaccine
- a shipwreck off Sea Island, Georgia
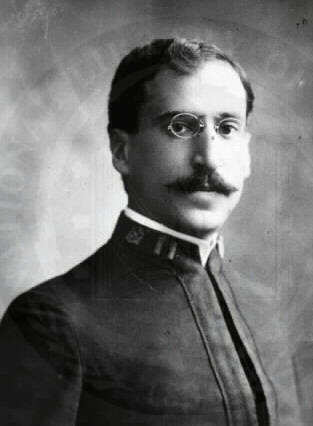
- Who is this person? Hint: Presently, he works in CBER's Office of Blood Research and Review.

- Jay Epstein
- Mark Elengold
- John Finlayson
- Karl Landsteiner

CBER Vision
Published quarterly by the Center for Biologics Evaluation and Research (CBER), Office of Communication, Training and Manufacturers Assistance (OCTMA), Division of Manufacturers Assistance and Training (DMAT) for CBER employees.
CBER Vision Office
Rockwall 1, Room 609
Phone: 301-827-2000 Fax: 301-827-3843
Director, DMAT
Gail Sherman (Sherman@cber.fda.gov)
Co-Editors
Seamus O'Boyle (Oboyle@cber.fda.gov)
Laura Woolf (Woolf@cber.fda.gov)

Quiz Answers:
1. a, 2. c, 3. b, 4. b, 5. a, 6. c.
|