News
Breaking BubR1 Mimics Genetic Shuffle Seen in Cancer Cells, Offers Opportunity to "Force Cancer's Hand"
PHILADELPHIA (Nov. 17, 2008) — A study of how one protein enzyme, BubR1, helps make sure chromosomes are equally distributed during mitosis might explain how the process of cell division goes so awry in cancer, according to researchers from Fox Chase Cancer Center. Their findings might offer a better understanding of the processes behind cancer-cell survival and drug-resistance.
In an article published online today in the Journal of Cell Biology, the Fox Chase researchers demonstrate that the BubR1 protein contains four separate functional areas that take part in cell division. Mutations in these areas, the researchers say, lead to a genetic rearrangement similar to a process that allows cancer cells to evade destruction by medical treatment. Inhibiting BubR1 could be a strategy that enhances the killing power of current therapeutics, co-author Tim J. Yen, PhD, believes.
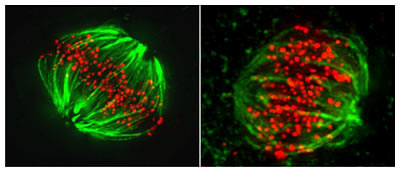
Left: Normal metaphase, kinetochores (red dots) attach to chromosomes (not visible), which are then pulled apart by microtubules (green lines). Right: A mutation in BubR1 causes kinetochores to create aberrant attachments to chromosomes, leading to improper segregation.
"Improper chromosomal segregation is a hallmark of cancer – it scrambles chromosomes and shuffles the genetic deck in a way that helps some cancer cells to evade destruction," says Yen, a senior member of the Fox Chase scientific staff. "This shuffling can, in effect, push a cancer cell to evolve in a way that allows it to survive drug or radiation therapy."
According to Yen, cancer cells survive by playing a risky evolutionary gamble. Improper chromosomal segregation allows cancer cells to shuffle their genetic deck to select for traits that allow them to survive and continue to grow. The downside of this strategy is that some daughter cells are dealt bad hands and die. As long as the genetic alterations are made on a relatively small scale, Yen says, cells within the tumor will continually evolve so that they can readily adapt to drugs.
"But here is an opportunity to force cancer's hand, as it were, by causing more damaging changes on a much larger scale than cancer cells can handle," Yen says. "Given that BubR1 is responsible for properly dealing from the genetic deck, its inhibition would result in catastrophic genetic changes that are incompatible with cancer-cell life."
The BubR1 enzyme has multiple roles as part of the cellular machinery that physically moves each of the 23 pairs of human chromosome into each new daughter cell. The protein also plays a part in regulating the so-called mitotic checkpoints, which serve as quality control for cell division. If the machinery does not function properly or the checkpoints are ignored, some daughter cells get more than their accustomed share of DNA, which can offer them a competitive advantage, Yen says.
Yen and Haomin Huang, PhD, a postdoctoral fellow in Yen's laboratory and lead author of the paper, determined that the structure of the BubR1 protein undergoes four chemical modifications that may be important for turning the activity of this enzyme off or on. By mutating BubR1 at positions within the protein that become chemically modified, the researchers were able to determine some of the protein's roles in the process of chromosome segregation during mitosis.
One position in particular, labeled S670, was found to be essential in preventing division errors. It serves as a means of connecting chromosomes to the microtubule proteins that pull them into the daughter cells. When the researchers prevented S670 from being properly modified, cell-culture studies showed that the chromosomes failed to be distributed equally between the daughter cells during division.
"Our studies show that of all the proteins and protein complexes associated with cell division, the phosphorylation status of BubR1 is a determining factor in cell-cycle control," Yen says. "Exploiting BubR1's crucial functions may help to increase the efficiency of cancer drugs that disrupt DNA replication, like gemcitabine, or drugs that prevent cell division, like paclitaxel."
Joining Yen and his Fox Chase colleagues in this study were researchers from GlaxoSmithKline and Avram Hershko, PhD, of the Technion-Israel Institute of Technology in Haifa, Israel. Hershko, a longtime visiting scientist at Fox Chase, joined the Yen laboratory while on sabbatical. Hershko and an Israeli colleague received the 2004 Nobel Prize in chemistry along with former Fox Chase researcher Irwin Rose, PhD, for their discovery of ubiquitin-mediated protein degradation at Fox Chase.
Grants from the Leukemia and Lymphoma Society, National Institutes of Health and the Commonwealth of Pennsylvania funded this study.
Fox Chase Cancer Center is one of the leading freestanding cancer research and treatments centers in the United States. Founded in 1904 in Philadelphia as the nation's first cancer hospital, Fox Chase became one of the first institutions to be designated a National Cancer Institute Comprehensive Cancer Center in 1974. Today, Fox Chase conducts a broad array of nationally competitive basic, translational, and clinical research, with special programs in cancer prevention, detection, treatment, and community outreach. For more information, call 1-888-FOX-CHASE or 1-888-369-2427. Other 2008 releases
Media inquiries only, please contact Gregory Lester at 215-728-2753.
 Print this Page
Print this Page
 E-mail This Page
E-mail This Page

