About This Booklet
The Cervix
Cancer Cells
Risk Factors
Symptoms
Detection and Diagnosis
Staging
Treatment
Second Opinion
Nutrition and Physical Activity
Follow-up Care
Sources of Support
Taking Part in Cancer Research
National Cancer Institute Information Resources
National Cancer Institute Publications
About This Booklet
This National Cancer Institute (NCI) booklet (NIH Publication No. 08-2407) is
about cervical cancer.* The disease begins on the
surface of the cervix. If not treated, the cancer invades
more deeply into the cervix. This is called invasive cervical cancer. Every year in the United States, about
11,000 women learn they have invasive cervical
cancer. Most of these women are younger than 55.
This booklet is only about invasive cervical
cancer. It's not about precancer, abnormal cells
found only on the surface of the cervix, or other
cervical changes. These cell changes are treated
differently from invasive cervical cancer.
Instead of this booklet, women with abnormal
cervical cells only on the surface may want to
read the NCI booklet Understanding Cervical
Changes: A Health Guide for Women 1. It tells
about abnormal cells and describes treatments.
Also, the NCI offers the following materials
about the Pap test and abnormal test results:
|
This booklet tells about diagnosis, staging,
treatment, and follow-up care. Learning about medical
care for invasive cervical cancer can help you take an
active part in making choices about your care.
This booklet has lists of questions that you may
want to ask your doctor. Many people find it helpful to
take a list of questions to a doctor visit. To help
remember what your doctor says, you can take notes or
ask whether you may use a tape recorder. You may also
want to have a family member or friend go with you
when you talk with the doctor - to take notes, ask
questions, or just listen.
For the latest information about cervical cancer,
please visit our Web site at
http://www.cancer.gov/cancertopics/types/cervical. Or, contact our Cancer
Information Service. We can answer your questions
about cancer. We can also send you NCI booklets
and fact sheets. Call 1-800-4-CANCER
(1-800-422-6237) or instant message us through the
LiveHelp 4 service at http://www.cancer.gov/help.
*Words in italics are in the Dictionary 5. The Dictionary
explains these terms. It also shows how to pronounce them.
The Cervix
The cervix is part of a woman's reproductive system.
It's in the pelvis. The cervix is the lower, narrow part
of the uterus (womb).
The cervix is a passageway:
- The cervix connects the uterus to the vagina. During
a menstrual period, blood flows from the uterus
through the cervix into the vagina. The vagina leads
to the outside of the body.
- The cervix makes mucus. During sex, mucus helps
sperm move from the vagina through the cervix into
the uterus.
- During pregnancy, the cervix is tightly closed to
help keep the baby inside the uterus. During
childbirth, the cervix opens to allow the baby to pass
through the vagina.
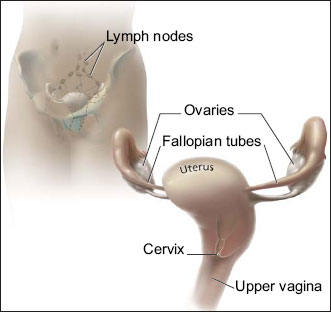 This picture shows the cervix and nearby organs.
This picture shows the cervix and nearby organs.
|
Cancer Cells
Cancer begins in cells, the building blocks that make
up tissues. Tissues make up the organs of the body.
Normal cells grow and divide to form new cells as
the body needs them. When normal cells grow old or
get damaged, they die, and new cells take their place.
Sometimes, this process goes wrong. New cells
form when the body does not need them, and old or
damaged cells do not die as they should. The buildup
of extra cells often forms a mass of tissue called a
growth or tumor.
Growths on the cervix can be benign or malignant.
Benign growths are not cancer. They are not as harmful
as malignant growths (cancer).
- Benign growths (polyps, cysts, or genital warts):
- are rarely a threat to life
- don't invade the tissues around them
- Malignant growths (cervical cancer):
- may sometimes be a threat to life
- can invade nearby tissues and organs
- can spread to other parts of the body
Cervical cancer begins in cells on the surface of the
cervix. Over time, the cervical cancer can invade more
deeply into the cervix and nearby tissues. The cancer
cells can spread by breaking away from the original
(primary) tumor. They enter blood vessels or lymph
vessels, which branch into all the tissues of the body.
The cancer cells may attach to other tissues and grow
to form new tumors that may damage those tissues.
The spread of cancer is called metastasis. See the
Staging 6 section for information about
cervical cancer that has spread.
Risk Factors
When you get a diagnosis of cancer, it's natural to
wonder what may have caused the disease. Doctors
cannot always explain why one woman develops
cervical cancer and another does not. However, we do
know that a woman with certain risk factors may be
more likely than others to develop cervical cancer. A
risk factor is something that may increase the chance
of developing a disease.
Studies have found a number of factors that may
increase the risk of cervical cancer. For example,
infection with HPV (human papillomavirus) is the
main cause of cervical cancer. HPV infection and other
risk factors may act together to increase the risk even
more:
- HPV infection: HPV is a group of viruses that can
infect the cervix. An HPV infection that doesn't go
away can cause cervical cancer in some women.
HPV is the cause of nearly all cervical cancers.
HPV infections are very common. These viruses are
passed from person to person through sexual
contact. Most adults have been infected with HPV at
some time in their lives, but most infections clear up
on their own.
Some types of HPV can cause changes to cells in
the cervix. If these changes are found early, cervical
cancer can be prevented by removing or killing the
changed cells before they can become cancer cells.
The NCI fact sheet Human Papillomaviruses and
Cancer: Questions and Answers 7 has more
information.
A vaccine for females ages 9 to 26 protects against
two types of HPV infection that cause cervical
cancer. The NCI fact sheet
Human Papillomavirus (HPV) Vaccines: Questions and Answers 8
has more
information.
-
Lack of regular Pap tests: Cervical cancer is more
common among women who don't have regular Pap
tests. The Pap test helps doctors find abnormal cells.
Removing or killing the abnormal cells usually
prevents cervical cancer.
- Smoking: Among women who are infected with
HPV, smoking cigarettes slightly increases the risk
of cervical cancer.
- Weakened immune system (the body's natural
defense system): Infection with HIV (the virus that
causes AIDS) or taking drugs that suppress the
immune system increases the risk of cervical cancer.
- Sexual history: Women who have had many sexual
partners have a higher risk of developing cervical
cancer. Also, a woman who has had sex with a man
who has had many sexual partners may be at higher
risk of developing cervical cancer. In both cases, the
risk of developing cervical cancer is higher because
these women have a higher risk of HPV infection.
- Using birth control pills for a long time: Using
birth control pills for a long time (5 or more years)
may slightly increase the risk of cervical cancer
among women with HPV infection. However, the
risk decreases quickly when women stop using birth
control pills.
- Having many children: Studies suggest that giving
birth to many children (5 or more) may slightly
increase the risk of cervical cancer among women
with HPV infection.
- DES (diethylstilbestrol): DES may increase the risk
of a rare form of cervical cancer in daughters
exposed to this drug before birth. DES was given to
some pregnant women in the United States between
about 1940 and 1971. (It is no longer given to
pregnant women.)
Having an HPV infection or other risk factors does
not mean that a woman will develop cervical cancer.
Most women who have risk factors for cervical cancer
never develop it.
Symptoms
Early cervical cancers usually don't cause
symptoms. When the cancer grows larger, women may
notice one or more of these symptoms:
- Abnormal vaginal bleeding
- Bleeding that occurs between regular menstrual
periods
- Bleeding after sexual intercourse, douching, or a
pelvic exam
- Menstrual periods that last longer and are heavier
than before
- Bleeding after going through menopause
- Increased vaginal discharge
- Pelvic pain
- Pain during sex
Infections or other health problems may also cause
these symptoms. Only a doctor can tell for sure. A
woman with any of these symptoms should tell her
doctor so that problems can be diagnosed and treated
as early as possible.
Detection and Diagnosis
Doctors recommend that women help reduce their
risk of cervical cancer by having regular Pap tests. A
Pap test (sometimes called Pap smear or cervical
smear) is a simple test used to look at cervical cells.
Pap tests can find cervical cancer or abnormal cells that
can lead to cervical cancer.
Finding and treating abnormal cells can prevent
most cervical cancer. Also, the Pap test can help find
cancer early, when treatment is more likely to be
effective.
For most women, the Pap test is not painful. It's
done in a doctor's office or clinic during a pelvic exam.
The doctor or nurse scrapes a sample of cells from the
cervix. A lab checks the cells under a microscope for
cell changes. Most often, abnormal cells found by a
Pap test are not cancerous. The same sample of cells
may be tested for HPV infection.
If you have abnormal Pap or HPV test results, your
doctor will suggest other tests to make a diagnosis:
- Colposcopy: The doctor uses a colposcope to look at
the cervix. The colposcope combines a bright light
with a magnifying lens to make tissue easier to see.
It is not inserted into the vagina. A colposcopy is
usually done in the doctor's office or clinic.
- Biopsy: Most women have tissue removed in the
doctor's office with local anesthesia. A pathologist
checks the tissue under a microscope for abnormal
cells.
- Punch biopsy: The doctor uses a sharp tool to
pinch off small samples of cervical tissue.
- LEEP: The doctor uses an electric wire loop to
slice off a thin, round piece of cervical tissue.
- Endocervical curettage: The doctor uses a curette
(a small, spoon-shaped instrument) to scrape a
small sample of tissue from the cervix. Some
doctors may use a thin, soft brush instead of a
curette.
- Conization: The doctor removes a cone-shaped
sample of tissue. A conization, or cone biopsy,
lets the pathologist see if abnormal cells are in the
tissue beneath the surface of the cervix. The
doctor may do this test in the hospital under
general anesthesia.
Removing tissue from the cervix may cause some
bleeding or other discharge. The area usually heals
quickly. Some women also feel some pain similar to
menstrual cramps. Your doctor can suggest medicine
that will help relieve your pain.
For more information about tests, cell changes, and
treatment for these changes, you may want to read
Understanding Cervical Changes 1. The NCI fact sheet
The Pap Test: Questions and Answers 3 tells how often
women should have Pap tests and how to prepare for
them.
|
You may want to ask the doctor these
questions before having a biopsy:
- Which biopsy method do you recommend?
- How will tissue be removed?
- Will I have to go to the hospital?
- How long will it take? Will I be awake? Will it
hurt?
- Are there any risks? What are the chances of
infection or bleeding after the test?
- For how many days afterward should I avoid
using tampons, douching, or having sex?
- Can the test affect my ability to get pregnant
and have children?
- How soon will I know the results? Who will
explain them to me?
- If I do have cancer, who will talk to me about
the next steps? When?
|
Staging
If the biopsy shows that you have cancer, your
doctor needs to learn the extent (stage) of the disease to
help you choose the best treatment. Staging is a careful
attempt to find out whether the tumor has invaded
nearby tissues, whether the cancer has spread and, if
so, to what parts of the body. Cervical cancer spreads
most often to nearby tissues in the pelvis, lymph nodes,
or the lungs. It may also spread to the liver or bones.
When cancer spreads from its original place to
another part of the body, the new tumor has the same
kind of cancer cells and the same name as the original
tumor. For example, if cervical cancer spreads to the
lungs, the cancer cells in the lungs are actually cervical
cancer cells. The disease is metastatic cervical cancer,
not lung cancer. For that reason, it's treated as cervical
cancer, not lung cancer. Doctors call the new tumor
"distant" or metastatic disease.
Your doctor will do a pelvic exam, feel for swollen
lymph nodes, and may remove additional tissue. To
learn the extent of disease, the doctor may order some
of the following tests:
- Chest x-rays: X-rays often can show whether cancer
has spread to the lungs.
- CT scan: An x-ray machine linked to a computer
takes a series of detailed pictures of your organs. A
tumor in the liver, lungs, or elsewhere in the body
can show up on the CT scan. You may receive
contrast material by injection in your arm or hand,
by mouth, or by enema. The contrast material makes
abnormal areas easier to see.
- MRI: A powerful magnet linked to a computer is
used to make detailed pictures of your pelvis and
abdomen. The doctor can view these pictures on a
monitor and can print them on film. An MRI can
show whether cancer has spread. Sometimes
contrast material makes abnormal areas show up
more clearly on the picture.
- PET scan: You receive an injection of a small
amount of radioactive sugar. A machine makes
computerized pictures of the sugar being used by
cells in your body. Cancer cells use sugar faster than
normal cells, and areas with cancer look brighter on
the pictures.
The stage is based on where cancer is found. These
are the stages of invasive cervical cancer:
- Stage I: The tumor has invaded the cervix beneath
the top layer of cells. Cancer cells are found only in
the cervix.
- Stage II: The tumor extends to the upper part of the
vagina. It may extend beyond the cervix into nearby
tissues toward the pelvic wall (the lining of the part
of the body between the hips). The tumor does not
invade the lower third of the vagina or the pelvic
wall.
- Stage III: The tumor extends to the lower part of
the vagina. It may also have invaded the pelvic wall.
If the tumor blocks the flow of urine, one or both
kidneys may not be working well.
- Stage IV: The tumor invades the bladder or rectum.
Or the cancer has spread to other parts of the body.
- Recurrent cancer: The cancer was treated, but has
returned after a period of time during which it could
not be detected. The cancer may show up again in
the cervix or in other parts of the body.
Treatment
Women with cervical cancer have many treatment
options. The options are surgery, radiation therapy,
chemotherapy, or a combination of methods.
The choice of treatment depends mainly on the size
of the tumor and whether the cancer has spread. The
treatment choice may also depend on whether you
would like to become pregnant someday.
Your doctor can describe your treatment choices, the
expected results of each, and the possible side effects.
You and your doctor can work together to develop a
treatment plan that meets your medical and personal
needs.
Your doctor may refer you to a specialist, or you
may ask for a referral. You may want to see a
gynecologic oncologist, a surgeon who specializes in
treating female cancers. Other specialists who treat
cervical cancer include
gynecologists, medical oncologists, and
radiation oncologists. Your health care
team may also include an oncology nurse and a
registered dietitian.
Before treatment starts, ask your health care team
about possible side effects and how treatment may
change your normal activities. Because cancer
treatments often damage healthy cells and tissues, side
effects are common. Side effects may not be the same
for each person, and they may change from one
treatment session to the next.
At any stage of the disease, supportive care is
available to relieve the side effects of treatment, to
control pain and other symptoms, and to help you cope
with the feelings that a diagnosis of cancer can bring.
You can get information about coping on NCI's Web
site at http://www.cancer.gov/cancertopics/coping
and from NCI's Cancer Information Service
at 1-800-4-CANCER or
LiveHelp 4
(http://www.cancer.gov/help).
You may want to talk to your doctor about taking
part in a clinical trial, a research study of new
treatment methods. See the section on
Taking Part in
Cancer Research 9.
|
You may want to ask the doctor these
questions before treatment begins:
- What is the stage of my disease? Has the
cancer spread? If so, where?
- May I have a copy of the report from the
pathologist?
- What are my treatment choices? Which do you
recommend for me? Will I have more than one
kind of treatment?
- What are the expected benefits of each kind of
treatment?
- What are the risks and possible side effects of
each treatment? What can we do to control the
side effects?
- What can I do to prepare for treatment?
- Will I have to stay in the hospital? If so, for
how long?
- What is the treatment likely to cost? Will my
insurance cover the cost?
- How will treatment affect my normal
activities?
- What can I do to take care of myself during
treatment?
- What is my chance of a full recovery?
- How often will I need checkups after
treatment?
- Would a clinical trial (research study) be right
for me?
|
Surgery is an option for women with Stage I or II
cervical cancer. The surgeon removes tissue that may
contain cancer cells:
- Radical trachelectomy: The surgeon removes the
cervix, part of the vagina, and the lymph nodes in
the pelvis. This option is for a small number of
women with small tumors who want to try to get
pregnant later on.
- Total hysterectomy: The surgeon removes the cervix
and uterus.
- Radical hysterectomy: The surgeon removes the
cervix, some tissue around the cervix, the uterus,
and part of the vagina.
With either total or radical hysterectomy, the
surgeon may remove other tissues:
- Fallopian tubes and ovaries: The surgeon may
remove both fallopian tubes and ovaries. This
surgery is called a salpingo-oophorectomy.
- Lymph nodes: The surgeon may remove the lymph
nodes near the tumor to see if they contain cancer. If
cancer cells have reached the lymph nodes, it means
the disease may have spread to other parts of the
body.
The time it takes to heal after surgery is different for
each woman. You may have pain or discomfort for the
first few days. Medicine can help control your pain.
Before surgery, you should discuss the plan for pain
relief with your doctor or nurse. After surgery, your
doctor can adjust the plan if you need more pain
control.
After a radical trachelectomy, some women have
bladder problems for a few days. The hospital stay
usually is about 2 to 5 days.
After a hysterectomy, the length of the hospital stay
may vary from several days to a week. It is common to
feel tired or weak for a while. You may have problems
with nausea and vomiting, and you may have bladder
and bowel problems. The doctor may restrict your diet
to liquids at first, with a gradual return to solid food.
Most women return to their normal activities within 4
to 8 weeks after surgery.
After a hysterectomy, women no longer have
menstrual periods. They cannot become pregnant.
When the ovaries are removed, menopause occurs at
once. Hot flashes and other symptoms of menopause
caused by surgery may be more severe than those
caused by natural menopause. You may wish to discuss
this with your doctor before surgery. Some drugs have
been shown to help with these symptoms, and they
may be more effective if started before surgery.
For some women, a hysterectomy can affect sexual
intimacy. You may have feelings of loss that make
intimacy difficult. Sharing these feelings with your
partner may be helpful. Sometimes couples talk with a
counselor to help them express their concerns.
|
You may want to ask the doctor these
questions before having surgery:
- Do you recommend surgery for me? If so,
which kind? Will my ovaries be removed? Do
I need to have lymph nodes removed?
- What is the goal of surgery?
- What are the risks of surgery?
- How will I feel after surgery? If I have pain,
how will it be controlled?
- How long will I have to be in the hospital?
- Will I have any lasting side effects? If I don't
have a hysterectomy, will I be able to get
pregnant and have children? If I get pregnant
later on, is there a bigger chance that I could
have a miscarriage?
- When will I be able to resume normal
activities?
- How will the surgery affect my sex life?
|
Radiation therapy (also called radiotherapy) is an
option for women with any stage of cervical cancer.
Women with early stage cervical cancer may choose
radiation therapy instead of surgery. It also may be
used after surgery to destroy any cancer cells that
remain in the area. Women with cancer that extends
beyond the cervix may have radiation therapy and
chemotherapy
Radiation therapy uses high-energy rays to kill
cancer cells. It affects cells only in the treated area.
Doctors use two types of radiation therapy to treat
cervical cancer. Some women receive both types:
- External radiation therapy: A large machine directs
radiation at your pelvis or other tissues where the
cancer has spread. The treatment usually is given in
a hospital or clinic. You may receive external
radiation 5 days a week for several weeks. Each
treatment takes only a few minutes.
- Internal radiation therapy: A thin tube is placed
inside the vagina. A radioactive substance is loaded
into the tube. You may need to stay in the hospital
while the radioactive source is in place (up to 3
days). Or the treatment session may last a few
minutes, and you can go home afterward. Once the
radioactive substance is removed, no radioactivity is
left in your body. Internal radiation may be repeated
two or more times over several weeks.
Side effects depend mainly on how much radiation
is given and which part of your body is treated.
Radiation to the abdomen and pelvis may cause
nausea, vomiting, diarrhea, or urinary problems. You
may lose hair in your genital area. Also, your skin in
the treated area may become red, dry, and tender.
You may have dryness, itching, or burning in your
vagina. Your doctor may advise you to wait to have sex
until a few weeks after radiation treatment ends.
You are likely to become tired during radiation
therapy, especially in the later weeks of treatment.
Resting is important, but doctors usually advise
patients to try to stay as active as they can.
Although the side effects of radiation therapy can be
upsetting, they can usually be treated or controlled.
Talk with your doctor or nurse about ways to relieve
discomfort.
It may also help to know that most side effects go
away when treatment ends. However, you may wish to
discuss with your doctor the possible long-term effects
of radiation therapy. For example, the radiation may
make the vagina narrower. A narrow vagina can make
sex or follow-up exams difficult. There are ways to
prevent this problem. If it does occur, however, your
health care team can tell you about ways to expand the
vagina.
Another long-term effect is that radiation aimed at
the pelvic area can harm the ovaries. Menstrual periods
usually stop, and women may have hot flashes and
vaginal dryness. Menstrual periods are more likely to
return for younger women. Women who may want to
get pregnant after radiation therapy should ask their
health care team about ways to preserve their eggs
before treatment starts.
You may find it helpful to read the NCI booklet
Radiation Therapy and You 10.
|
You may want to ask the doctor these
questions before having radiation therapy:
- What is the goal of this treatment?
- How will the radiation be given?
- Will I need to stay in the hospital? If so, for
how long?
- When will the treatments begin? How often
will I have them? When will they end?
- How will I feel during treatment? Are there
side effects?
- How will we know if the radiation therapy is
working?
- Will I be able to continue my normal activities
during treatment?
- How will radiation therapy affect my sex life?
- Are there lasting side effects?
- Will I be able to get pregnant and have
children after my treatment is over?
|
For the treatment of cervical cancer, chemotherapy
is usually combined with radiation therapy. For cancer
that has spread to distant organs, chemotherapy alone
may be used.
Chemotherapy uses drugs to kill cancer cells. The
drugs for cervical cancer are usually given through a
vein (intravenous). You may receive chemotherapy in a
clinic, at the doctor's office, or at home. Some women
need to stay in the hospital during treatment.
The side effects depend mainly on which drugs are
given and how much. Chemotherapy kills fast-growing
cancer cells, but the drugs can also harm normal cells
that divide rapidly:
- Blood cells: When chemotherapy lowers the levels
of healthy blood cells, you're more likely to get
infections, bruise or bleed easily, and feel very weak
and tired. Your health care team will check for low
levels of blood cells. If your levels are low, your
health care team may stop the chemotherapy for a
while or reduce the dose of drug. There are also
medicines that can help your body make new blood
cells.
- Cells in hair roots: Chemotherapy may cause hair
loss. If you lose your hair, it will grow back, but it
may change in color and texture.
- Cells that line the digestive tract: Chemotherapy
can cause a poor appetite, nausea and vomiting,
diarrhea, or mouth and lip sores. Your health care
team can give you medicines and suggest other
ways to help with these problems.
Other side effects include skin rash, tingling or
numbness in your hands and feet, hearing problems,
loss of balance, joint pain, or swollen legs and feet.
Your health care team can suggest ways to control
many of these problems. Most go away when treatment
ends.
You may wish to read the NCI booklet
Chemotherapy and You 11.
|
You may want to ask the doctor these
questions before having chemotherapy:
- Why do I need this treatment?
- Which drug or drugs will I have?
- How do the drugs work?
- What are the expected benefits of the
treatment?
- What are the risks and possible side effects of
treatment? What can we do about them?
- When will treatment start? When will it end?
- How will treatment affect my normal
activities?
|
Second Opinion
Before starting treatment, you might want a second
opinion about your diagnosis and treatment plan. Some
people worry that the doctor will be offended if they
ask for a second opinion. Usually the opposite is true.
Most doctors welcome a second opinion. And many
health insurance companies will pay for a second
opinion if you or your doctor requests it.
If you get a second opinion, the doctor may agree
with your first doctor's diagnosis and treatment plan.
Or the second doctor may suggest another approach.
Either way, you have more information and perhaps a
greater sense of control. You can feel more confident
about the decisions you make, knowing that you've
looked at your options.
It may take some time and effort to gather your
medical records and see another doctor. In most cases,
it's not a problem to take several weeks to get a second
opinion. The delay in starting treatment usually will not
make treatment less effective. To make sure, you
should discuss this delay with your doctor.
There are many ways to find a doctor for a second
opinion. You can ask your doctor, a local or state
medical society, a nearby hospital, or a medical school
for names of specialists. NCI's Cancer Information
Service at 1-800-4-CANCER can tell you about
nearby treatment centers. Other sources can be found in
NCI's fact sheet How To Find a Doctor or Treatment
Facility If You Have Cancer 12.
Nutrition and Physical Activity
It's important for you to take care of yourself by
eating well and staying as active as you can.
You need the right amount of calories to maintain a
good weight. You also need enough protein to keep up
your strength. Eating well may help you feel better and
have more energy.
However, you may not feel like eating during or
soon after treatment. You may be uncomfortable or
tired. You may find that foods don't taste as good as
they used to. In addition, the side effects of treatment
(such as poor appetite, nausea, vomiting, or mouth
sores) can make it hard to eat well. Your doctor, a
registered dietitian, or another health care provider can
suggest ways to cope with these problems. Also, the
NCI booklet Eating Hints for Cancer Patients 13 has
many useful ideas and recipes.
Research shows that people with cancer feel better
when they stay active. Walking, yoga, swimming, and
other activities can keep you strong and increase your
energy. Exercise may reduce nausea and pain and make
treatment easier to handle. It also can help relieve
stress. Whatever physical activity you choose, be sure
to talk to your doctor before you start. Also, if your
activity causes you pain or other problems, be sure to
let your doctor or nurse know about it.
Follow-up Care
You'll need regular checkups after treatment for
cervical cancer. Checkups help ensure that any changes
in your health are noted and treated if needed. If you
have any health problems between checkups, you
should contact your doctor.
Your doctor will check for the return of cancer. Even
when the cancer seems to have been completely
removed or destroyed, the disease sometimes returns
because undetected cancer cells remained somewhere
in the body after treatment. Checkups may include a
physical exam, Pap tests, and chest x-rays.
The NCI has publications to help answer questions
about follow-up care and other concerns. You may find
it helpful to read the NCI booklet Facing Forward:
Life After Cancer Treatment 14. You may also want to
read the NCI fact sheet Follow-up Care After Cancer
Treatment: Questions and Answers 15.
|
You may want to ask your doctor these
questions after you have finished treatment:
- How often will I need checkups?
- How often will I need a Pap test?
- What other follow-up tests do you suggest for
me?
- Between checkups, what health problems or
symptoms should I tell you about?
|
Sources of Support
Learning you have cervical cancer can change your
life and the lives of those close to you. These changes
can be hard to handle. It's normal for you, your family,
and your friends to have many different and sometimes
confusing feelings.
Concerns about treatments and managing side
effects, hospital stays, and medical bills are common.
You may also worry about caring for your family,
keeping your job, or continuing daily activities.
Here's where you can go for support:
- Doctors, nurses, and other members of your health
care team can answer questions about treatment,
working, or other activities.
- Social workers, counselors, or members of the
clergy can be helpful if you want to talk about your
feelings or concerns. Often, social workers can
suggest resources for financial aid, transportation,
home care, or emotional support.
- Support groups also can help. In these groups,
patients or their family members meet with other
patients or their families to share what they have
learned about coping with the disease and the effects
of treatment. Groups may offer support in person,
over the telephone, or on the Internet. You may want
to talk with a member of your health care team
about finding a support group.
- Information specialists at 1-800-4-CANCER and
at
LiveHelp 4 (http://www.cancer.gov/help) can help
you locate programs, services, and publications.
They can send you a list of organizations that offer
services to people with cancer.
- Your doctor or a sex counselor may be helpful if
you and your partner are concerned about the effects
of cervical cancer on your sexual relationship. You
and your partner may find it helps to discuss your
concerns.
For tips on coping, you may want to read the NCI
booklet Taking Time: Support for People With Cancer 16.
Taking Part in Cancer Research
Doctors all over the country are conducting many
types of clinical trials (research studies in which people
volunteer to take part). They are studying new ways to
treat cervical cancer. Some are also studying therapies
that may improve the quality of life for women during
or after cancer treatment.
Clinical trials are designed to answer important
questions and to find out whether new approaches are
safe and effective. Research already has led to
advances in the prevention, diagnosis, and treatment of
cervical cancer. Doctors continue to search for new and
better ways to treat cervical cancer. They are testing
new treatments, including new drugs, combinations,
and schedules. Some trials are combining
chemotherapy, surgery, and radiation therapy.
Doctors also are studying surgery to remove sentinel
lymph nodes. A sentinel lymph node is the first lymph
node to which the cancer is likely to spread. Today,
surgeons often have to remove many lymph nodes and
check each of them for cancer. But if the research
shows that it's possible to identify the sentinel lymph
node (the lymph node most likely to have cancer),
doctors may be able to avoid more surgery to remove
other lymph nodes.
Even if the people in a trial don't benefit directly,
they may still make an important contribution by
helping doctors learn more about cervical cancer and
how to control it. Although clinical trials may pose
some risks, researchers do all they can to protect their
patients.
If you are interested in taking part in a clinical trial,
talk with your doctor. You may want to read the NCI
booklet Taking Part in Cancer Treatment Research
Studies 17. It describes how treatment studies are carried
out and explains their possible benefits and risks.
NCI's Web site includes a section on clinical trials
at http://www.cancer.gov/clinicaltrials. It has
general information about clinical trials as well as
detailed information about specific ongoing studies of
cervical cancer. NCI's Information Specialists at
1-800-4-CANCER or at
LiveHelp 4 at
http://www.cancer.gov/help can answer questions and
provide information about clinical trials.
National Cancer Institute Information Resources
You may want more information for yourself, your
family, and your doctor. The following NCI services
are available to help you.
NCI's Cancer Information Service (CIS) provides
accurate, up-to-date information about cancer to
patients and their families, health professionals, and the
general public. Information specialists translate the
latest scientific information into plain language, and
they will respond in English or Spanish, as well as
through TRS providers for the hearing or speech
impaired. Calls to the CIS are confidential and free.
|
Telephone:
|
1-800-4-CANCER (1-800-422-6237)
|
NCI's Web site provides information from numerous
NCI sources. It offers current information about cancer
prevention, screening, diagnosis, treatment, genetics,
supportive care, and ongoing clinical trials. It has
information about NCI's research programs, funding
opportunities, and cancer statistics.
If you're unable to find what you need on the Web
site, contact NCI staff. Use the online contact form at
http://www.cancer.gov/contact
or send an email to
cancergovstaff@mail.nih.gov.
Also, information specialists provide live,
online assistance through
LiveHelp 4 at
http://www.cancer.gov/help.
National Cancer Institute Publications
NCI provides publications about cancer, including
the booklets and fact sheets mentioned in this booklet.
Many are available in both English and Spanish.
You may order these publications by telephone, on
the Internet, or by mail. You may also read them online
and print your own copy.
- By telephone: People in the United States and its
territories may order these and other NCI
publications by calling the NCI's Cancer
Information Service at 1-800-4-CANCER.
- On the Internet: Many NCI publications may be
viewed, downloaded, and ordered from
http://www.cancer.gov/publications on the
Internet. People in the United States and its
territories may use this Web site to order printed
copies. This Web site also explains how people
outside the United States can mail or fax their
requests for NCI booklets.
- By mail: NCI publications may be ordered by
writing to the address below:
Publications Ordering Service
National Cancer Institute
P.O. Box 24128
Baltimore, MD 21227
|