 | ||||||||
 |  |  |  |  | ||||
 | |||
| Setup Instructions |
| Office
of Rural Health Policy FY 2005 Annual Report
Table of Contents Vision, Mission and Strategic Goals
Vision, Mission and Strategic Goals ORHP Vision Mission Goals Goal 1: Improve the health and wellness of people living in rural communities and in the U.S.-Mexico border region Goal 2: Improve the financial viability of small rural hospitals, rural health clinics, and other rural providers Goal 3: Sustain and improve access to outpatient, inpatient, pharmaceutical and emergency room care for rural communities and along the U.S.-Mexico border The Office of Rural Health Policy (ORHP) coordinates rural health policy issues within the U.S. Department of Health and Human Services. In FY 2005, ORHP administered 13 grant programs with a focus on capacity building at the community and State levels. While located within the Health Resources and Services Administration, the office has a department-wide responsibility to analyze the impact of departmental policy on rural communities. ORHP is both a policy and programmatic resource for rural communities. The office's policy role is created by Section 711 of the Social Security Act, which charges the office with advising the Secretary on rural health issues. In that role, the office examines issues such as the effects of Medicare and Medicaid on rural citizens' access to health care, specifically on the viability of rural hospitals and the availability of rural physicians. The office's programs also provide funding at both the community and State levels to support improved rural health care delivery. Through its community-based programs, the office supports projects that improve access to health care services, encourage network development among rural health care providers, enhance delivery of emergency medical services and place and train people in the use of automatic external defibrillators. In addition, the office assumes responsibility for managing HRSA's border health activities. Much of the 2,100-mile U.S.-Mexico border is rural and the urban regions face health care delivery challenges similar to rural areas, such as limited health workforce capacity and a fragile infrastructure. Authorizing Legislation for ORHP Activities: Rural Access to Emergency Devices Grant Program Public Access to Defibrillation Demonstration
Projects Rural EMS Training and Equipment Assistance
Program Rural Health Research Centers Program Policy Oriented Rural Health Services Research
Program Frontier Extended Stay Clinics Demonstration Medicare Rural Hospital Flexibility Grant Program Small Rural Hospital Improvement Grant Program Rural Health Outreach Grant Program Delta States Rural Development Network Grant
Program Network Development Grant Program State Offices of Rural Health Grant Program Network Development Planning Grant Program
Labor-Health
and Human Services-Education and Related Agencies
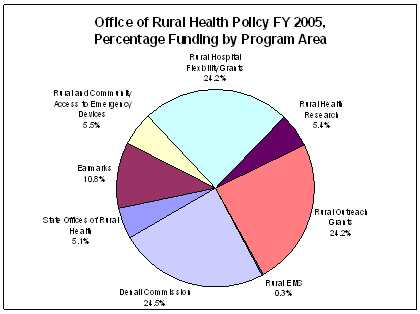
Chart 1. Chart 2 - Total number of ORHP grants and amounts by State, in FY 2005.
REGULATIONS AND KEY POLICY ISSUES: The specific Medicare regulations that come through ORHP for review vary somewhat from year to year, however the major Medicare payment system regulations generally come through for review during both the proposed rule-making and final rule-making cycles. Recently, regulations relating the Medicare Advantage, Medicare Drug Benefit and various quality reporting programs also have been received in the office and reviewed for comment. Medicaid and SCHIP are State-based programs and much of the discretion for these programs is left to the States. However, ORHP does participate in the departmental review of Medicaid and SCHIP waiver proposals to assure that the interests of rural Medicaid beneficiaries are considered. Our role in workforce policy encompasses a wide variety of issues including Graduate Medical Education, J1-Visa Waivers, the National Health Service Corps and Title VII programs that provide support to rural providers. Quality issues are relatively new to the office, as they are to Federal programs in general, but review and input into quality measurement and reporting programs has become a regular and important activity. Key Policy Accomplishments The creation of the Medicare Advantage Regional Preferred Provider Organizations by the Medicare Modernization Act (MMA) was intended to give a beneficiary living in a rural area the advantage of having a choice of methods through which he or she can receive Medicare benefits. As such, we felt it was important to assure that the regulations for the new program allowed this goal to be met. Through the comment process, we worked with the Centers for Medicare and Medicaid Service (CMS) to revise some proposed restrictions on "essential hospitals," assure that rural providers without access to the Internet could receive important documents from Medicare Advantage Plans, and revise language concerning cost-based providers. During the establishment of the Medicare Prescription Drug Benefit, ORHP provided multiple comments to CMS regarding how their proposed regulations might better account for the needs of rural providers and beneficiaries. We were successful in obtaining a change in the network access standards that allows for certain closed-access pharmacies, including those operated by Rural Health Clinics, to count toward meeting the required access standards in areas that lack a sufficient number of open-access pharmacies. ORHP often identifies issues of particular concern to rural providers during its review of the Medicare payment system regulations. We had many concerns about a proposal in the FY 2006 IPPS regulations to restrict the circumstances under which Critical Access Hospitals (CAH) could relocate their facilities and retain their CAH designation. We submitted multiple comments explaining our concerns and the potential affects that the proposed policy might have on rural communities. CMS ultimately revised the regulations and we supported its final policy. During the FY 2006 IPPS regulations process, we also worked closely with CMS to revise several definitions of rural used for both CAHs and other rural hospitals. These revised definitions will assure that hospitals in areas considered rural under several different definitions will continue to be considered rural for purposes of Medicare payment. The CY 2006 Outpatient Prospective Payment System (OPPS) regulations offered us the opportunity to provide assistance to CMS in developing a payment add-on for certain rural hospitals. We worked with CMS to review data and payment policies that ultimately resulted in a payment add-on for a subset of rural hospitals that were determined to have the most need. SPECIAL PROJECTS AND PARTNERSHIPS: One of the unique aspects of the Office of Rural Health Policy is its entrepreneurial nature. Since its inception, the office has put an emphasis on working with key partners and organizations to develop projects to address long-standing rural health problems. The office uses a portion of its funding in the Policy/Research line to support these activities. The emphasis of these special projects is either to highlight an issue or work with key rural partners to develop services or resources that fill an identified need. Some of these "special projects" are focused on the needs of all rural communities, such as the need for general information on rural health. Others may focus only on a specific issue such as the recruitment and retention of health workforce or the role of economic development in health care. Still other activities focus on a particular type of health care providers. In each case, however, the projects and initiatives supported by the office meet an identified rural health care need. The Rural Assistance Center (RAC) is one of the best examples of this investment. In its authorizing statute, the office was charged by Congress with establishing and maintaining "a clearinghouse for collecting and disseminating information on rural health care issues, including rural mental health, rural infant mortality prevention, rural occupational safety and preventive health promotion, research findings relating to rural health care and innovative approaches to the delivery of health care in rural areas.1 The need for such a resource was further heightened by the findings of "One Department Serving Rural America," a report by the Rural Task Force of the U.S. Department of Health and Human Services to the Secretary.2 This report identified the need for a single coordinated point of contact on rural issues for all the HHS programs that affect rural communities. The RAC was established in December 2002 as a rural health and human services "information portal." RAC helps rural communities and other rural stakeholders access the full range of available programs, funding and research that can enable them to provide quality health and human services to rural residents. Services provided include RAC's Web site (www.raconline.org), electronic mailing lists, and customized assistance. The site has had 586,589 hits since inception and has an average turnaround time of less than 24 hours for individual requests. In FY 2005, the RAC continued to expand the level and breadth of information and services for rural residents. In addition, the project also added new sites and information resources related to border health issues and health disparities in the Delta region of the country. Another long-standing effort of the office examines the important link between economic development and health care in rural communities. The health sector is often one of the top employers in a rural economy, a role and relationship that often is not fully understood. The Center for Rural Health Works (RHWks) is an ongoing program that works to strengthen local systems of health. As the national focal point, it provides technical assistance, tools and training to help States measure the economic impact of the health-care sector on local, regional and State economies. It also develops feasibility studies for new health care services. During FY 2005, Center for RHWks activities included conducting two regional workshops, responding to more than 300 requests for technical assistance, developing models for measuring the economic impact of a CAH and a FQHC on local communities and sharing the results of their studies/activities at 16 regional and national conferences. The National Association of Counties (NACo)
has established a partnership with Center for Rural Health Works
to help county elected officials take the lead in conducting a comprehensive
community engagement process for health and economic development.
The purpose of this project is to help communities recognize that
improving their health care system has a direct and positive impact
on local economic growth. This is a new initiative for FY 2005.
During this first year of the program, the NACo Project produced
three county-level reports on economic impact, community need, health
services directory and data/information. The reports were provided
to each county and placed on the NACo website. NACo also disseminated
information about this project through workshops at its Western
Regional and Annual Conferences and through articles in NACo's publication
"County News." With FY 2005 funds, REMSTTAC was able to conduct a wide range of activities. The center provided technical assistance to rural communities relating to EMS and trauma systems. It also represented and provided a rural voice for EMS and trauma in various meetings sponsored by national associations, State governments and Federal agencies. Funding supported the development and dissemination of the "Rural EMS Agenda" for the future. REMSTTAC sponsored a Town Hall Meeting in Park City, Utah. In addition, it began the development of written products that will assist EMS and trauma rural providers. Provider-Focused Technical Assistance ORHP works to develop and provide technical assistance and information sharing for rural health care providers to strengthen and expand their ability to provide quality health care. ORHP's provider-focused TA and information sharing efforts in 2005 involved Rural Health Clinic TA Conference Calls, 340B TA for Rural Hospitals, the Delta Rural Hospital Performance Improvement Project and the Alaska Rural Hospital Performance Improvement Project. New in FY 2005, Rural Health Center TA Conference Calls focused on providing Rural Health Clinics (RHCs) with four national technical assistance conference calls each year. These calls were the only federally funded technical assistance provided specifically to RHCs. The topics were determined about one month before each call by an advisory group comprised of experts in the area of RHCs. FY 2005 funds supported the cost of phone lines, speakers and administration of four to six hour-long calls. The topics covered included billing and coding, shortage designation application, health information technology and cost reporting, among others. The calls attracted an average of 175 participants each. As a result of a change in the law in 2003, more than 250 rural hospitals may now qualify to participate in the 340b Discount Drug purchasing program. To assist these facilities in signing up for the program, the ORHP provided supplemental funding to the HRSA Pharmacy Services Support Center (PSSC) in FY 2005 to assist rural hospitals in understanding and applying for participation in the 340b discount drug purchasing program. The PSSC is a resource established in 2002 to assist HRSA grantees and eligible health care sites to optimize the value of the 340B Program and provide clinically and cost effective pharmacy services that improve medication use and advance patient care. The PSSC operates under a contract between the American Pharmacists Association (APhA) and the Office of Pharmacy Affairs (OPA), in the HRSA Healthcare Systems Bureau. To date, 140 rural hospitals are taking part in the 340b program as a result of this assistance. The Delta Rural Hospital Performance Improvement Project (RHPI) is designed to increase access to quality health care services in the Mississippi Delta by improving the financial, operational and clinical performance of its small rural hospitals. On-site technical assistance is available to 122 hospitals in eight States. This project is also developing and implementing a performance improvement strategy based on the Balanced Scorecard (BSC) technology. In 2005, the Delta RHPI Project carried out a range of activities. It delivered TA to 17 unique hospitals, including 11 Performance Improvement Assessments (PIAs), 10 Targeted Consultations and Balance Scorecard (BSC) consultations in three hospitals. Additionally the project made tools available through the project Web site, conducted sustainability meetings in four States, surveyed all assisted hospitals regarding project success and made numerous presentations about this project. The project has conducted both process and outcomes evaluations. The Alaska Rural Hospital Performance Improvement Project, new in FY 2005, provided on-site technical assistance to hospitals in Alaska that request assistance. The TA was targeted at helping these hospitals improve their financial, clinical and operational performance. FY 2005 money funded three on-site TA visits to Alaska hospitals, as well as follow-up services to provide assistance during the implementation of recommendations made during the site visits. There is an established link between the benefits of health information technology (HIT) adoption and quality improvement. There also is an emerging need for support for rural providers to make informed decisions about their HIT futures, as well as processes and business tools to help them make decisions. Therefore, in an effort to work toward rural equity of HIT adoption, ORHP will hold a national rural HIT meeting, Health Information Technology: A Provider's Roadmap to Quality, in September 2006. This meeting will provide an opportunity for rural providers to learn about the basic components of HIT, focus on the initial steps of strategic planning for HIT investments and share best practices and lessons learned about HIT implementation. The meeting will bring together 300 rural providers to discuss strategic planning for HIT investments. In planning for the 2006 meeting, the HIT External Planning Team, made up of a group of 13 rural HIT experts, met in Washington, D.C., on Nov. 7-8, 2005. In other efforts to further the adoption and implementation of HIT by rural providers, ORHP provided funding to the Technical Assistance and Services Center to develop key expertise, partnerships and tools for critical access hospitals (CAHs) to consider as they look to invest in HIT. This is an ongoing project. With 2005 funding, the Technical Assistance and Services Center for the Rural Hospital Flexibility program (TASC) will deliver tools and a customized portal. The tools will identify key areas of expertise needed to assist CAHs in their clinical, financial, leadership and staffing domains, most likely in the form of a primer on HIT. The portal will be a customized space for knowledge sharing, access and workspace on the AHRQ HIT portal site for the CAHs and other rural health care providers. Health Care Workforce The National Rural Recruitment and Retention Network (3RNet) works to increase the number of providers practicing in rural America. The project consists of 43 State-based, not-for-profit organizations that encourage and assist physicians and other health professionals in locating practices in underserved rural communities. Members include State Offices of Rural Health, Primary Care Offices, Primary Care Associations and Area Health Education Centers and other not-for-profit entities. During FY 2005, 3RNet helped States improve their retention and recruitment (R&R) activities especially for primary care physicians, RNs, dentists, pharmacists and mental health professionals. Members placed 715 medical professionals in 622 communities and 568 of those were in HPSAs and MUAs. 3RNet also maintained a toll-free phone line to assist providers interested in serving rural America. The Network continues conducting workshops, training, and presentations for those interested in recruiting and keeping providers in rural communities. In addition, 3RNet is working with HRSA programs to promote effective R&R into areas served by these programs. A new project, J1 Visa Report WWAMI (Washington, Wyoming, Alaska, Montana and Idaho) focuses on analyzing data to determine the contribution of J1-visa waiver physicians to the rural physician workforce. There have been multiple changes to the various programs that approve these waivers. These changes have influenced those applying for waivers in certain programs. This has led to confusion over the actual aggregate numbers of physicians applying for waivers in exchange for agreeing to practice in rural areas. This project seeks to analyze existing data sources to better understand the supply of J1-visa waiver physicians and determine placement trends. With FY 2005 funding, the University of Washington Rural Health Research Center, which has a heavy focus on rural workforce issues, will analyze various data sets to determine where J1 visa waiver physicians are practicing in rural communities. The ORHP funds a number of projects in its efforts to influence rural health policy to make quality, affordable health care accessible in rural areas. One of these endeavors, the ongoing Policy Analysis Cooperative Agreement, supports the performance of research and analysis on key policy issues affecting rural communities. The 2005 funding supported several activities. This includes working with rural community colleges on health workforce issues. The cooperative agreement also supports ongoing work of the Rural Policy Research Institute (RUPRI) Rural Health Panel. The RUPRI Rural Health Panel provides science-based, objective policy analysis to Federal policy makers. Panel members come from a variety of academic disciplines and create documents that reflect the consensus judgment of all panelists. The grant also provides staff support to the Rural Hospitals Issues Group, a panel of small rural hospital administrators and rural hospital finance experts from across the country to discuss issues such as the MMA, Medicare Advantage, and other policy issues affecting small rural hospitals. A new project, the CAH/Hospice Financial Report, was created to analyze and predict the financial impact that providing general inpatient and respite hospice services will have on Critical Access Hospitals (CAHs). FY 2005 funds supported the development and analysis of a financial model that depicts the likely financial impact of the provision of hospice services on CAHs with various cost structures. Funding for the National Conference of State Legislatures (NCSL) supports an existing cooperative agreement through the Bureau of Primary Health Care which provides funding support to the NCSL for an annual meeting focusing on a key rural health issue of interest to rural State legislators. With 2005 funds, NCSL convened a day-long conference to examine the relationship between health care and economic development in rural areas, and identify strategies and resources available to help rural communities thrive. Best Practices and Emerging Issues in Rural Health The ORHP also funds public health efforts and a program of all-inclusive care for the elderly as part of its work on communicating best practices and addressing emerging issues in rural health. This ongoing Public Health funding supports an existing cooperative agreement with the National Association of County and City Health Officials (NACCHO) through the Bureau of Primary Health Care which provides technical assistance to community and migrant health centers. The Office of Rural Health Policy supplements this cooperative agreement to ensure that key rural issues are addressed in the public health arena and information on rural activities is communicated. Fiscal year 2005 funds supported several activities including: the creation and maintenance of a rural listserv; an issue brief on workforce development; rural sessions at the NACCHO Annual Conference; six scholarships for rural Local Public Health Agencies (LPHAs) to attend the NACCHO Annual Conference; two skills building scholarships for rural LPHAs to attend a social marketing public health conference; the creation of an internal NACCHO Rural Health workgroup and updates on rural health resources and issues in the NACCHO Exchange and the Public Health Dispatch. The purpose of the Program of All-inclusive Care for the Elderly (PACE) model, a Medicare demonstration project, is to expand community-based long-term care options for seniors through comprehensive coordination of preventive, primary, acute, and long-term care services. It is a unique capitated managed care benefit for the frail elderly provided by a not-for-profit or public entity that features a comprehensive medical and social service delivery system. There is little or no penetration of this model into rural areas. What is not known is how many rural providers are interested in the PACE model and how viable this model might be for meeting the needs of frail elderly in rural communities. FY 2005 funds supported a range of activities related to PACE. The project offered consultation with potential providers and a two-day meeting for all PACE Providers to determine progress in the development of rural PACE sites. Discussion between ORHP and the National PACE Association (NPA) has begun on evaluation component. In addition, NPA provided technical assistance to providers on ways to receive start-up PACE site funding. The ORHP created a new project in FY 2005 to address women's health issues. The mission of the Bright Futures for Women's Health and Wellness Initiative is to plan, develop, implement and evaluate a variety of culturally competent consumer, provider, and community-based products to increase awareness and use of preventive health services for all women across their lifespan. The objectives of this project are to aid rural women and adolescent girls in the following ways: 1) providing information to rural women on recommended preventive health services so that they seek care based on their individual needs and share in the decision-making about their health services and 2) providing tools for rural practitioners to use in making all health care visits an opportunity to offer preventive care. FY 2005 funding used to modify an existing set of physical activity and healthy eating tools for consumers and health care providers in rural settings. The final version of these materials is expected on Aug. 30, 2006 Funding for a frontier health project supports the Frontier Education Center, which provides technical assistance to individuals seeking information on frontier health care issues and produces 3-4 issue papers on frontier health-specific topics. Funding supported papers focusing on topics including the use of health information technology for public health activities in the U.S.-Mexico Border region, the applicability of the Frontier Extended Stay Clinic model to sites in the "lower 48," and developing baseline information to analyze the impact of the Medicare drug benefit on frontier communities with a sole pharmacy. Collaboration with the National Rural Health Association (NRHA) The Office of Rural Health Policy collaborates with the National Rural Health Association (NRHA) on several fronts to identify, analyze and address rural health needs. The purpose of one of the collaborative efforts, the Rural Medical Educators' Conference and Technical Assistance, is to share innovative ways to get more medical professionals into rural areas as well as discuss new issues in rural health education. This is an ongoing program. FY 2005 funds supported the planning and execution of the Rural Medical Educators Annual Conference in May 2006. The conference will bring together about 50 physicians, students, residents and professors who strive to bring medical professionals (including doctors and nurses) into rural environments. Additionally, in response to issues brought to the forefront by the Institute of Medicine's 2005 rural health quality report "Quality Through Collaboration," a new Rural Hospital and Community Technical Assistance project seeks to improve quality of health care in rural communities. Funding supports in-depth technical assistance through three to five site visits. These visits are designed to promote health care quality in rural areas. In addition, funds are used to collect best practices and rural needs in quality improvement as well as create a rural quality focus group. Another Quality project, new in FY 2005, was funded to support several activities including planning a quality conference, writing a rural health quality best practices manual and bringing in four speakers to the Quality Conference in July 2006. In addition, funds will provide National Quality Forum Membership for the National Rural Health Association to provide input and have a "rural vote" in the forum. The Office of Rural Health Policy also collaborates with the NRHA to hold several policy forums throughout the year for key stakeholders to discuss various issues, such as Medicare, acute care, etc. The forums educate participants about rural community-based health models and begin developing reports on best practices. Another joint endeavor by ORHP and the NRHA, the Cooperative of Health Networks, will develop a series of performance measures in order to measure progress of the Rural Health Network Grants. In FY 2005, the first year of funding, money was used to identify possible measures. The Regional Meetings - Best Practices is a new project meant to improve rural health quality and promote the use of best practices by working with State Rural Health Associations. Technical assistance will be delivered through a series of presentations and site visits. In addition to technical assistance, this program will collect quality improvement models that work. This collection of best practices will be distributed nationally. Further, an ongoing Annual Meeting Support project supports various parts of the National Rural Health Association's annual meeting. The annual meeting brings together the broad rural health community for continuing education and networking. FY 2005 funding was provided to support eight sessions on topics such as rural Health Information Technology, the National Advisory Council, Rural Voices, mental health and substance abuse, a committee on rural health and human services, improving systems collaboration, updates from ORHP and BPHC and a Medicaid update. Another collaborative effort between ORHP and NRHA brought about State Rural Health Association Grants to support the rural health community at the State level through a variety of different activities. It is a continuing project. With FY 2005 funding, 34 grants of $9,500 were administered to support activities such as rural health newsletters, conferences, educational activities, skill building, etc. In 2005, 20 of the State Rural Health Associations (SRHAs) devoted portions of their annual meeting to educating rural citizens about the findings in the Institute of Medicine's "Quality Through Collaboration" report on rural health quality issues. Other SRHAs used their meetings to share information about the new Medicare drug benefit while others focused on issues such as health information technology. Other collaborative efforts with the NRHA resulted in the Ag Health program that provides technical assistance in order to raise awareness of health and safety issues associated with agriculture, decrease the number of related accidents and illnesses, and improve treatment. It is a new program in FY 2005. The Ag Health program provided agriculture health training, such as farm safety, to health professionals who have patients working in agriculture. ORHP also facilitates intra-agency border health activities that cut across the Bureaus and Offices of HRSA. In FY 2005, funds supported the Border Health Clearinghouse in the Rural Assistance Center, which aims to develop a border Website within the RAC (www.raconline.org) for health and human services information. This bilingual site serves as a clearinghouse for information on border health issues. The border health website was launched on schedule in January 2006. ORHP also supported the U.S.-Mexico Border Health Association Meeting to further educate clinicians and community workers about HRSA programs and the progress toward achieving U.S.-Mexico Border 2010 Health Objectives. ORHP supported the annual U.S.-Mexico Border Health Association Meeting in Laredo, Texas, through the provision of logistical support for educational seminars for providers. The purpose of the Pan-American Health Organization Immunizations program is to further educate clinicians and community workers in the appropriate use of vaccines and to facilitate the vaccination of children and adults in local clinics and community health centers along the US-Mexico border. FY 2005 funding provided logistical support for Immunization in the Americas Week. In FY 2005, ORHP supported a new Border Environmental Coordination Research Program is to fund research to test the hypothesis that environmental education and training is an effective intervention tool for improving public health. The target population is lay community health workers, or promotoras, residing along the U.S.-Mexico border and the communities they serve. This project, jointly sponsored by EPA and HRSA, supports larger border health efforts including, but not limited to, the U.S.-Mexico Border 2012 program (www.epa.gov/usmexicoborder). Funding from FY 2005 supported the development of a research protocol to examine pesticide exposure in rural border areas by Texas A&M University. Medicare Rural Hospital Flexibility Grant Program
(Flex) The Rural Hospital Flexibility Program is a Federal initiative that provides funding to State governments to stabilize rural hospital economics, integrate emergency medical services (EMS) into the health care system and improve quality of care. Flex funds support the conversion of small rural hospitals to Critical Access status, which allows them to receive cost-based reimbursement from Medicare for inpatient and outpatient services. Flex funding to the States also encourages the development of collaborative systems of care in rural areas, including the CAHs, EMS providers, clinics and other providers of high-quality, necessary health care services. The CAH program requires participating States to develop rural health plans, and funds the States to support and implement community-level outreach and technical assistance. Although focused on very small, rural hospitals, this complex intervention operates on the national, State, community and facility levels and covers a broad range of health service issues. Changes to the Program Key Program Accomplishments The Program has also stimulated the development of dozens of rural health networks in the participating States. Network types have ranged from small, hospital-based networks to Statewide networks involving all CAHs to multi-State networks devoted to improving quality of care.
Small Rural Hospital Improvement Grant
Program (SHIP) The purpose of the SHIP grant program is to help small rural hospitals do any or all of the following: 1) pay for costs related to implementation of prospective payment systems (PPS); 2) comply with provisions of the Health Insurance Portability and Accountability Act (HIPAA) of 1996; and 3) reduce medical errors and support quality improvement (QI) efforts. State Offices of Rural Health help rural hospitals to participate in the program. In FY 2005, $14.7 million was awarded to 1,523 eligible hospitals in 46 States and Puerto Rico and each hospital received approximately $9,700. Changes to the Program The use of SHIP funds for reduction of medical error and quality improvement activities increased from 49 percent in FY 2003 to 53 percent in FY 2004 while the use of SHIP funds for HIPAA activities decreased from 46.5 percent in FY 2003 to 39.5 percent in FY 2004. The use of grant funds for PPS activities remains relatively constant at 6 percent. Key Program Accomplishments During FY 2004, 53 percent of the funds ($7.8 million) were expended for projects and initiatives related to quality improvement. HIPAA activities received 40 percent of the funds ($5.9 million) and PPS activities received 7 percent ($1 million) of the funds. Of the 1,523 participating SHIP hospitals, 1,095 or 72 percent used some or all of their grant funds to invest in health information technology (HIT). Seventy percent (771) of the hospitals used SHIP funds to secure new or upgrade existing hardware and software infrastructure that serve as the foundation for business office, security and quality improvement functions. Twelve percent (127) of the hospitals expended funds on hardware or software related to business office functions such as coding, billing or accounting software. Forty percent (436) identified their HIT expenditures as specific to compliance with the HIPAA security rule and 58 percent (634) invested in HIT for quality improvement activities.
Rural Health Outreach Grant Program The purpose of the Rural Health Care Services Outreach (Outreach) Grant Program is to provide funds to expand the delivery of health care services in rural communities. The history of rural health care in the United States is one of underserved people and under-resourced providers. Many factors contribute to the story: geographic isolation, low incomes, lack of insurance and too few caregivers, to name a few. The Outreach Grant Program encourages the development of new and innovative health care delivery systems in rural communities that lack essential health care services. Programs funded vary greatly and have brought care that would not otherwise have been available to at least 4 million rural citizens across the country. The emphasis of the grant program is on service delivery through creative strategies requiring the grantee to form a consortium with at least two additional partners. The consortium should include local providers and other organizations that support the delivery of health care. The Outreach projects are based on demonstrated community needs. The population to be served should be included in identifying and planning for the services that will be provided. All projects need to be responsive to the unique cultural, social, belief and linguistic needs of the target population. Applicants may propose to deliver different types of services, including primary care, dental care, mental health services, home health care, emergency care, health promotion and education programs, outpatient day care and other services not requiring inpatient care. In fiscal year FY2005, 30 new and 72 continuing grants (102 total grants) were awarded, totaling $18,821,464. Changes to the Program Key Program Accomplishments Outreach program grantees successfully expand health services delivery each year, by increasing the number of people served in rural communities. Two examples of Outreach grantees that have received national recognition for projects that were conceived and developed using Outreach Grant Program funds are the Sickness Prevention Achieved through Regional Collaboration (SPARC), which focused on breast cancer detection in older women in a contiguous rural area at the junction of Connecticut, Massachusetts and New York, as well as the Diabetes Lay Educator Program in Morehead, Minn. that provided services for migrant Hispanic farm workers who have diabetes.
Delta States Rural Development Network
Grant Program The purpose of the Delta States Rural Development (Delta) Grant Program is to support community organizations in the development and implementation of projects to address local health care needs in the rural Delta Region. A single grant is awarded to one organization within each of the eight Delta States (Alabama, Arkansas, Illinois, Kentucky, Louisiana, Mississippi, Missouri and Tennessee) collectively known as the Delta Regional Authority (DRA). The eight states are comprised of 207 eligible counties. ORHP provides support for the counties within the DRA through activities designed to strengthen the safety net and small rural hospital performance, demonstration projects for improving collaboration across counties among existing grant programs and providing technical assistance and outreach funds to small rural communities. In fiscal year 2005, eight grants were awarded to the DRA totaling $5,090,751. Changes to the Program Key Program Accomplishments The Alabama Delta grantee has garnered the buy-in of two counties, which previously opted to not be involved in the grant program, to become active participants in the Delta grant and have received funding for health implementation projects. Alabama's partnership with the Southern Rural Access Program has provided an opportunity for the grantee to engage in the practice management model by providing technical assistance to primary care providers throughout the region. This represents the first multi-county effort ever initiated by Alabama's Delta States project. Through TA, several grantees, including Arkansas and Lousiana, were able to leverage additional grant funds in excess of $1.35 million to assist in other initiatives within the various Delta States. Local projects in Illinois were able to develop school based health centers in three sites and a coordinated referral service for patients of an established volunteer free clinic. Kentucky initiated a pharmaceutical access program assisting low-income adults to take advantage of low cost pharmaceuticals in 10 Delta counties. Grantees in Kentucky and Missouri have also been involved in pilot project targeting to the ARC and DRA region regarding a new pharmaceutical web-based pharmaceutical system.
Network Development Grant Program The purpose of the grant is to "expand access to, coordinate and improve the quality of essential health care services, and enhance the delivery of health care in rural areas." These grants support rural providers who work together in formal networks, alliances, coalitions or partnerships to integrate administrative, clinical, technological and financial functions across their organizations. The funds provided through this program are not used for the direct delivery of services. The ultimate goal of the RHND Grant Program is to strengthen existing health care networks in order to achieve business (network partner return) and social (community return) competencies that increase access and quality of rural health care and, ultimately, the health status of rural residents. Nine new grants and 28 continuing grants were funded in FY 2005 (37 total grants) totaling $6,974,893. Changes to the Program Key Program Accomplishments The Upper Peninsula Health Care Network in Michigan adopted and endorsed a cooperative pharmacy formulary management system. The network then used the combined volume of their 15 hospitals to leverage Performance Discount/Rebate Agreements in the purchase of prescription drugs. In the case of one particular drug, the network expects annual net savings for the network hospitals to be as much as $74,000 from this drug alone. In addition to continuing grant-funded work in the adaptation and implementation of a web-based information management software program to link rural safety net providers, the East Texas Health Access Network (ETHAN) was able to provide significant aid to victims of hurricanes Katrina and Rita. Network members provided direct patient care and medication assistance to hundreds of evacuees, obtained donations of insulin, food, clothing and hygiene supplies, and conducted door-to-door search and rescue activities in two eastern Texas counties. Two days after Rita hit, network staff reopened the ETHAN Office using a generator, and kept updated information on the location of open hospitals, food distribution sites, etc. for evacuees. North Country Health Consortium in New Hampshire leveraged additional funds to support the Molar Express, the network's mobile regional public health dental clinic, which provided screenings to over 500 Medicaid-eligible North Country children between April and December of 2005. Grand Traverse Regional Health Care Coalition of Michigan signed a contract with the State to operate the Adult Benefit Waiver I (ABWI) program in three target counties. The network's participation in this program allows access to Federal matching dollars for other local programs.
Network Development Planning Grant Program
The purpose of the Rural Health Network Development Planning Grant Program is similar to the Network Development Grant Program in that it seeks to "achieve efficiencies; expand access to, coordinate and improve the quality of essential health care services; and strengthen the rural health care system as a whole." These grants support rural communities needing assistance in planning, organizing and developing a health care network. Funds cannot be used for direct delivery of health care services. The grant supports one year of planning to develop a network and help them become operational. Nineteen new grants were awarded in fiscal year 2005 totaling $1,563.49. Changes to the Program Key Program Accomplishments Alaska Small Hospital Performance Improvement
Network (ASHPIN), Juneau, AK Planning Equals Access for Louisiana (PEAL),
Napoleonville, LA Collaborative Action for TAOS County Health
(CATCH), Taos, NM
State Offices of Rural Health Grant Program The purpose of the State Offices of Rural Health (SORH) Grant Program is to assist States in strengthening rural health care delivery systems by creating a focal point for rural health within each State. The program provides an institutional framework that links small rural communities with State and Federal resources to help develop long term solutions to rural health problems. There are three core functions of the SORH: (1) to serve as a rural health clearing house of information and innovative approaches to the delivery of services; (2) to coordinate State activities related to rural health in order to avoid duplication of efforts and resources; and (3) to identify Federal, State, and nongovernmental programs regarding rural health and provide technical assistance to public and nonprofit private entities regarding participation in such programs. In fiscal year 2005, 50 non-competing continuation grants were awarded for a total of $7,401,171. The maximum level of funding awarded was $150,000, which 46 of the 50 States requested and received. Each State is also required to match the SORH Federal funding at a minimum 3:1 ratio; a unique leveraging component for the program. Changes to the Program Key Program Accomplishments The program encourages each State to promote rural recruitment and retention efforts of health professionals. The SORHs are the primary dues-paying members to the Rural Recruitment and Retention Network (3RNet) which in 2005 recruited 742 health professionals of which 450 of these were primary care physicians. State Offices continue to leverage significant partnerships with the goal of improving rural health. In 2005, an example of the impact of these partnerships is seen through the Rural Hospital Performance Improvement project (RHPI). SORHs in MS, LA, AR, AL, TN, IL, KY, and MO are worked collaboratively with their State Hospital Associations (SHAs) to provide input and expertise. In particular, the SORHs worked with the contractor to ensure that the on-site technical assistance was well-managed and appropriate to the needs of each hospital. The SORHs and SHAs also continue to follow up with the hospital after technical assistance is rendered. The SORHs are continuously working with Federal, State and local partners to improve the collaboration among safety net providers in rural areas of their States. In particular, 18 SORHs applied with their State partners to an ORHP initiative to "Improve Collaboration Between Critical Access Hospitals (CAHs) and Federally Qualified Health Centers (FQHCs)." Funding was available to provide technical assistance to four of the States; those were Louisiana, Texas, New Hampshire and Arkansas. In each of these States, the SORH took the lead in bringing together the State-level partners (PCO, PCA, SHA). The technical assistance was provided through consultants to the State teams to assist them in better understanding the roles and relationships between CAHs and FQHCs. As a result of the leadership from the SORHs, each of the States has developed plans and strategies for improved collaboration between the CAHs and FQHCs in their States.
Rural Access to Emergency Devices The purpose of the Rural Access to Emergency Devices (RAED) Grant Program is to provide funding to rural community partnerships to purchase automated external defibrillators (AEDs) that have been approved, or cleared for marketing by the Food and Drug Administration; and provide defibrillator and basic life support training in AED usage through the American Heart Association, the American Red Cross, or other nationally recognized training courses. The legislation that created this program states that awards will be made to community partnerships. A community partnership is composed of local emergency response entities such as community training facilities, local emergency responders, fire and rescue departments, police, community hospitals and local non-profit entities and for-profit entities. Forty-eight non-competing continuation grants were awarded in FY 2005 totaling $7,252,903. Changes to the Program Key Program Accomplishments
Public Access to Defibrillation Demonstration
Projects The purpose of the Public Access to Defibrillation Demonstration Project (PADDP) is to award grants to political subdivisions of States, Indian tribes and tribal organizations to develop and implement innovative, comprehensive, community-based public access defibrillation demonstration projects that provide cardiopulmonary resuscitation (CPR) and automated external defibrillation (AED) to cardiac arrest victims, provide training to community members in CPR and AED usage, and to maximize community access to AEDs. In fiscal year 2005 four non-competing continuation grants were awarded totaling $930,663. Changes to the Program Key Program Accomplishments The PADDP Program has resulted in increased public awareness, increased number of AEDs available and an increase in persons, first responders and lay persons, trained in the utilization of AEDs in the event of sudden cardiac arrest.
Rural Health Research Centers The Rural Health Research Centers (RHRCs) Program is designed to help policy makers understand the problems that rural communities face in assuring access to health care for their residents. The RHRCs study issues facing rural communities in their quest to secure adequate, affordable, quality health services for their residents. This is the only Federal program that is dedicated entirely to producing policy-relevant research on health care in rural areas. The work done by the Centers is also critical to helping the Office play its policy role within the Department. The research done by the RHRCs help provide important data and findings to the office's policy staff which they bring to bear in their annual review of key Departmental regulations. Eight Centers in eight States were competitively awarded cooperative agreements for the period FY 2005-2008. The eight RHRCs conducted 25 research projects and wrote 25 policy briefs and technical reports about their results. All RHRCs have websites which highlight their rural research results. Key Program accomplishments
Rural Emergency Medical Service Training
and Equipment Assistance Program The purpose of the Rural Emergency Medical Service Training and Equipment Assistance Program (REMSTEP) is to assist entities to develop improved emergency medical services (EMS) in rural areas by improving the recruitment, training, certification and retaining of volunteer and paid EMS personnel with a special emphasis in the use of technology-enhanced education methods. The grant also funds the purchase of EMS and personal protective equipment. The office provides support to these grantees through the EMS and Trauma Technical Assistance Center and by requiring the use of community partnerships and the involvement of the grantee's State Office of Rural Health program. In fiscal year 2005 three grants were awarded as continuation grants to the REMSTEP program totaling $356,313. Fiscal Year 2006 the Congress chose not to fund this program. Grantees will complete the current funded year and will be instructed on how to close the program. Changes to the Program Key Program Accomplishments Washington: Inland Northwest Health Services (INHS) in collaboration with Spokane County EMS and the Spoke County Medical Director, created EMS Live At Night! (EMS Live). EMS Live provides monthly education forum using interactive video conferencing broadcasts to rural communities throughout eastern Washington. The grant funds have been utilized to expand the program to more than 300 EMS agencies not only in the State of Washington, but also to Northern Idaho, North Central Oregon, and the Eastern Aleutian Tribes of Alaska. The success of the program prompted the State of Montana to request, and was accepted as a partner State. Wisconsin: In partnership with six hospitals, four are CAHs, 10 ambulance services from Sandusky and Huron counties, the Sanilac Medical Services in Sandusky, Michigan developed an EMS program to increase access to EMS training, reduce barriers when accessing EMS training or services, increase awareness of the value and importance of EMS volunteers, and increase the incentives to increase EMS volunteers.
Frontier Extended Stay Clinic Program The purpose of the Frontier Extended Stay Clinic (FESC) Cooperative Agreement Program is to examine the effectiveness and appropriateness of a new type of provider, the FESC, in providing health care services in certain remote locations. In remote, frontier areas of the country, weather and distance can prevent patients who experience severe injury or illness from obtaining immediate transport to an acute care hospital. For residents in some of those communities, providers offer observation services traditionally associated with acute care inpatient hospitals until the patient can be transferred or is no longer in need of transport. Provision of these services requires the staffing, equipment and quality assurance programs of an acute care hospital. However, extended stay services are not currently reimbursed by Medicare, Medicaid or other third-party payers. For several years, officials in the State of Alaska and several State Offices of Rural Health, Primary Care Offices and Primary Care Associations have explored the development of a new provider type, or other mechanism, that would enable reimbursement of these services through the FESC model. The Medicare Prescription Drug Improvement and
Modernization Act of 2003 (MMA) authorized the Centers for Medicare
and Medicaid Services (CMS) to conduct a demonstration program in
which FESCs would be treated as Medicare providers. Under MMA, FESCs
are defined as clinics that are: 1) located in communities which
are at least 75 miles away from the closest hospital or are inaccessible
by public road and 2) designed to address the needs of patients
who are unable to be transferred to an acute care facility because
of adverse weather conditions or who need monitoring and observation
for a limited period of time. Changes to the Program Key Program Accomplishments
Footnotes 1. Section 711 of the Social Security Act. 2. "One Department Serving Rural America," February, 2003. 3. This activity had received funding through the Trauma/EMS line in the annual budget due to a rural 10 percent set aside in this line item in the budget line authorized under Title XII of the Public Health Service Act. However, the funding in this line item was eliminated in the FY 2006 budget.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
![]()
Go to:
Top | HRSA | HHS
| Disclaimer | Accessibility
| Privacy