This National Cancer Institute (NCI) booklet (NIH Publication No. 08-1575) is about multiple myeloma,* a cancer that starts in plasma cells, a type of white blood cell. It's also called plasma cell myeloma. Each year in the United States, about 20,000 people learn they have this disease.
This booklet tells about diagnosis, treatment options, and tests the doctor may give you during follow-up visits. It also tells about supportive care before, during, or after treatment. Learning about the medical care for multiple myeloma can help you take an active part in making choices about your care.
This booklet has lists of questions that you may
want to ask your doctor. Many people find it helpful to
take a list of questions to a doctor visit. To help
remember what your doctor says, you can take notes or
ask whether you may use a tape recorder. You may also
want to have a family member or friend go with you
when you talk with the doctor - to take part in the
discussion, to take notes, or just to listen.
Back to Top
What is Multiple Myeloma?
Multiple myeloma is a type of cancer. Cancer is a group of many related diseases. Myeloma is a cancer that starts in plasma cells, a type of white blood cell. It's the most common type of plasma cell cancer.
Normal Blood Cells
Most blood cells develop from cells in the bone marrow called stem cells. Bone marrow is the soft material in the center of most bones.
Stem cells mature into different types of blood cells. Each type has a special job:
- White blood cells help fight infection. There are several types of white blood cells.
- Platelets help form blood clots that control bleeding.
Plasma cells are white blood cells that make antibodies. Antibodies are part of the immune system. They work with other parts of the immune system to help protect the body from germs and other harmful substances. Each type of plasma cell makes a different antibody.

Normal plasma cells help protect the body from germs and other harmful
substances.
|
Myeloma Cells
Myeloma, like other cancers, begins in cells. In cancer, new cells form when the body doesn't need them, and old or damaged cells don't die when they should. These extra cells can form a mass of tissue called a growth or tumor.
Myeloma begins when a plasma cell becomes abnormal. The abnormal cell divides to make copies of itself. The new cells divide again and again, making more and more abnormal cells. These abnormal plasma cells are called myeloma cells.
In time, myeloma cells collect in the bone marrow. They may damage the solid part of the bone. When myeloma cells collect in several of your bones, the disease is called "multiple myeloma." This disease may also harm other tissues and organs, such as the kidneys.
Myeloma cells make antibodies called M proteins and other proteins. These proteins can collect in the blood, urine, and organs.
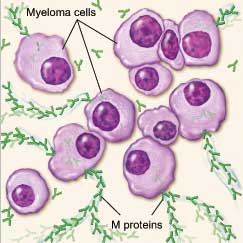
Myeloma cell (abnormal plasma cell) making M proteins.
|
Back to Top
Risk Factors
No one knows the exact causes of multiple myeloma. Doctors seldom know why one person
develops this disease and another doesn't. However, we do know that multiple myeloma isn't contagious. You cannot catch it from another person.
Research has shown that certain risk factors increase the chance that a person will develop this disease. Studies have found the following risk factors for multiple myeloma:
- Age over 65: Growing older increases the chance of developing multiple myeloma. Most people with myeloma are diagnosed after age 65. This disease is rare in people younger than 35.
- Race: The risk of multiple myeloma is highest among African Americans and lowest among Asian Americans. The reason for the difference between racial groups is not known.
- Being a man: Each year in the United States, about 11,200 men and 8,700 women are diagnosed with multiple myeloma. It is not known why more men are diagnosed with the disease.
- Personal history of monoclonal gammopathy of undetermined significance (MGUS): MGUS is a benign condition in which abnormal plasma cells make M proteins. Usually, there are no symptoms, and the abnormal level of M protein is found with a blood test. Sometimes, people with MGUS develop
certain cancers, such as multiple myeloma. There is no treatment, but people with MGUS get regular lab tests (every 1 or 2 years) to check for a further increase in the level of M protein. They also get regular exams to check for the development of symptoms.
- Family history of multiple myeloma: Studies have found that a person's risk of multiple myeloma may be higher if a close relative had the disease.
Many other suspected risk factors are under study. Researchers have studied whether being exposed to certain chemicals or germs (especially viruses), having alterations in certain genes, eating certain foods, or being obese increases the risk of developing multiple myeloma. Researchers continue to study these and other possible risk factors.
Having one or more risk factors does not mean that a person will develop myeloma. Most people who have risk factors never develop cancer.
Back to Top
Symptoms
Common symptoms of multiple myeloma include:
- Bone pain, usually in the back and ribs
- Broken bones, usually in the spine
- Feeling weak and very tired
- Feeling very thirsty
- Frequent infections and fevers
- Weight loss
- Nausea or constipation
- Frequent urination
Most often, these symptoms are not due to cancer.
Other health problems may also cause these symptoms.
Only a doctor can tell for sure. Anyone with these
symptoms should tell the doctor so that problems can
be diagnosed and treated as early as possible.
Back to Top
Diagnosis
Doctors sometimes find multiple myeloma after a
routine blood test. More often, doctors suspect multiple
myeloma after an x-ray for a broken bone. Usually
though, patients go to the doctor because they are
having other symptoms.
To find out whether such problems are from
multiple myeloma or some other condition, your doctor
may ask about your personal and family medical
history and do a physical exam. Your doctor also may
order some of the following tests:
|
You may want to ask your doctor these questions before having a bone marrow aspiration or biopsy:
- Will you remove the sample of bone marrow
from the hip or from another bone?
- Where will I go for this procedure?
- Will I have to do anything to prepare for it?
- How long will it take? Will I be awake?
- Will it hurt? What will you do to prevent or
control the pain?
- Are there any risks? What are the chances of
infection or bleeding after the procedure?
- How long will it take me to recover?
- How soon will I know the results? Who will
explain them to me?
- If I do have multiple myeloma, who will talk
to me about next steps? When?
|
Back to Top
Staging
If the biopsy shows that you have multiple
myeloma, your doctor needs to learn the extent (stage)
of the disease to plan the best treatment. Staging may
involve having more tests:
- Blood tests: For staging, the doctor considers the
results of blood tests, including albumin and
beta-2-microglobulin.
- CT scan: An x-ray machine linked to a computer
takes a series of detailed pictures of your bones.
- MRI: A powerful magnet linked to a computer is
used to make detailed pictures of your bones.
Doctors may describe multiple myeloma as
smoldering, Stage I, Stage II, or Stage III. The stage
takes into account whether the cancer is causing
problems with your bones or kidneys. Smoldering
multiple myeloma is early disease without any
symptoms. For example, there is no bone damage.
Early disease with symptoms (such as bone damage) is
Stage I. Stage II or III is more advanced, and more
myeloma cells are found in the body.
Back to Top
Treatment
People with multiple myeloma have many treatment
options. The options are watchful waiting, induction
therapy, and stem cell transplant. Sometimes a combination of methods is used.
Radiation therapy is used sometimes to treat painful
bone disease. It may be used alone or along with other
therapies. See the Supportive Care section to learn about ways to relieve pain.
The choice of treatment depends mainly on how
advanced the disease is and whether you have
symptoms. If you have multiple myeloma without
symptoms (smoldering myeloma), you may not need
cancer treatment right away. The doctor monitors your
health closely (watchful waiting) so that treatment can
start when you begin to have symptoms.
If you have symptoms, you will likely get induction
therapy. Sometimes a stem cell transplant is part of the
treatment plan.
When treatment for myeloma is needed, it can often
control the disease and its symptoms. People may
receive therapy to help keep the cancer in remission,
but myeloma can seldom be cured. Because standard
treatment may not control myeloma, you may want to
talk to your doctor about taking part in a clinical trial.
Clinical trials are research studies of new treatment
methods. See the Taking Part in Cancer Research section.
Your doctor can describe your treatment choices, the
expected results, and the possible side effects. You and
your doctor can work together to develop a treatment
plan that meets your needs.
Your doctor may refer you to a specialist, or you
may ask for a referral. Specialists who treat multiple
myeloma include hematologists and medical oncologists. Your health care team may also include an
oncology nurse and a registered dietitian.
Before treatment starts, ask your health care team to
explain possible side effects and how treatment may
change your normal activities. Because cancer
treatments often damage healthy cells and tissues, side
effects are common. Side effects may not be the same
for each person, and they may change from one
treatment session to the next.
|
You may want to ask your doctor these questions before you begin treatment:
- What stage of myeloma do I have?
- Is the disease affecting my kidneys?
- How do I get a copy of the report from the
pathologist?
- What are my treatment choices? Which do you
recommend for me? Why?
- Will I have more than one kind of treatment?
How will my treatment change over time?
- What are the expected benefits of each kind of
treatment?
- What are the risks and possible side effects of
each treatment? What can we do to control the
side effects?
- What can I do to prepare for treatment?
- Will I need to stay in the hospital? If so, for
how long?
- What is the treatment likely to cost? Will my
insurance cover the cost?
- How will treatment affect my normal activities?
- Would a clinical trial be right for me? Can you
help me find one?
- How often should I have checkups?
|
People with smoldering myeloma or Stage I
myeloma may be able to put off having cancer
treatment. By delaying treatment, you can avoid the
side effects of treatment until you have symptoms.
If you and your doctor agree that watchful waiting is
a good idea, you will have regular checkups (such as
every 3 months). You will receive treatment if
symptoms occur.
Although watchful waiting avoids or delays the side
effects of cancer treatment, this choice has risks. In
some cases, it may reduce the chance to control
myeloma before it gets worse.
You may decide against watchful waiting if you
don't want to live with untreated myeloma. If you
choose watchful waiting but grow concerned later, you
should discuss your feelings with your doctor. Another
approach is an option in most cases.
|
You may want to ask your doctor these questions before choosing watchful waiting:
- If I choose watchful waiting, can I change my mind later on?
- Will the cancer be harder to treat later?
- How often will I have checkups?
- Between checkups, what problems should I tell you about?
|
Many different types of drugs are used to treat
myeloma. People often receive a combination of drugs,
and many different combinations are used to treat
myeloma.
Each type of drug kills cancer cells in a different
way:
- Chemotherapy: Chemotherapy kills fast-growing
myeloma cells, but the drug can also harm normal
cells that divide rapidly.
- Targeted therapy: Targeted therapies use drugs that
block the growth of myeloma cells. The targeted
therapy blocks the action of an abnormal protein
that stimulates the growth of myeloma cells.
- Steroids: Some steroids have antitumor effects. It is
thought that steroids can trigger the death of
myeloma cells. A steroid may be used alone or with
other drugs to treat myeloma.
You may receive the drugs by mouth or through a
vein (IV). The treatment usually takes place in an
outpatient part of the hospital, at your doctor's office,
or at home. Some people may need to stay in the
hospital for treatment.
The side effects depend mainly on which drugs are
given and how much:
- Blood cells: When a drug used for myeloma
treatment lowers the levels of healthy blood cells,
you're more likely to get infections, bruise or bleed
easily, and feel very weak and tired. Your health
care team will check for low levels of blood cells. If
your levels are low, your health care team may stop
therapy for a while or reduce the dose of drug.
There are also medicines that can help your body
make new blood cells.
- Cells in hair roots: Chemotherapy may cause hair
loss. If you lose your hair, it will grow back, but it
may be somewhat different in color and texture.
- Cells that line the digestive tract: Chemotherapy
and targeted therapy can cause poor appetite, nausea
and vomiting, diarrhea, constipation, or mouth and
lip sores. Ask your health care team about medicines
and other ways to help you cope with these
problems.
The drugs used for myeloma may also cause
dizziness, drowsiness, numbness or tingling in hands or
feet, and low blood pressure. Most of these problems
go away when treatment ends.
You may find it helpful to read the NCI booklet
Chemotherapy and You. You may also want to read the
NCI fact sheet Targeted Cancer Therapies: Questions and Answers.
|
You may want to ask your doctor these questions before having induction therapy:
- Which drugs will I get? What will the
treatment do?
- When will treatment start? When will it end?
How often will I have treatments?
- Where will I go for treatment? Will I have to
stay in the hospital?
- Will I have side effects during treatment? What
side effects should I tell you about? Can I
prevent or treat any of these side effects?
- Will there be lasting side effects? How long
will they last? What can I do about them?
- How often will I need checkups?
|
Many people with multiple myeloma may get a
stem cell transplant. A stem cell transplant allows you
to be treated with high doses of drugs. The high doses
destroy both myeloma cells and normal blood cells
in the bone marrow. After you receive high-dose
treatment, you receive healthy stem cells through a
vein. (It's like getting a blood transfusion.) New blood
cells develop from the transplanted stem cells. The new
blood cells replace the ones that were destroyed by
treatment.
Stem cell transplants take place in the hospital.
Some people with myeloma have two or more
transplants.
Stem cells may come from you or from someone
who donates their stem cells to you:
- From you: An autologous stem cell transplant uses
your own stem cells. Before you get the high-dose
chemotherapy, your stem cells are removed. The
cells may be treated to kill any myeloma cells
present. Your stem cells are frozen and stored. After
you receive high-dose chemotherapy, the stored
stem cells are thawed and returned to you.
- From a family member or other donor: An
allogeneic stem cell transplant uses healthy stem
cells from a donor. Your brother, sister, or parent
may be the donor. Sometimes the stem cells come
from a donor who isn't related. Doctors use blood
tests to be sure the donor's cells match your cells.
Allogeneic stem cell transplants are under study for
the treatment of multiple myeloma.
- From your identical twin: If you have an identical
twin, a syngeneic stem cell transplant uses stem
cells from your healthy twin.
There are two ways to get stem cells for people with
myeloma. They usually come from the blood
(peripheral blood stem cell transplant). Or they can
come from the bone marrow (bone marrow transplant).
After a stem cell transplant, you may stay in the
hospital for several weeks or months. You'll be at risk
for infections because of the large doses of
chemotherapy you received. In time, the transplanted
stem cells will begin to produce healthy blood cells.
You may find it helpful to read the NCI fact sheet
Bone Marrow Transplantation and Peripheral Blood Stem Cell Transplantation: Questions and Answers.
|
You may want to ask your doctor these questions before having a stem cell transplant:
- What kind of stem cell transplant will I have? If I need a donor, how will we find one?
- How long will I be in the hospital? Will I need special care? How will I be protected from
germs? Will my visitors have to wear a mask? Will I?
- What care will I need when I leave the
hospital?
- How will we know if the treatment is working?
- What are the risks and the side effects? What
can we do about them?
- What changes in normal activities will be
necessary?
- What is my chance of a full recovery? How
long will that take?
- How often will I need checkups?
|
Back to Top
Second Opinion
Before starting treatment, you might want a second
opinion about your diagnosis and treatment plan. Some
people worry that the doctor will be offended if they
ask for a second opinion. Usually the opposite is true.
Most doctors welcome a second opinion. And many
health insurance companies will pay for a second
opinion if you or your doctor requests it.
If you get a second opinion, the doctor may agree
with your first doctor's diagnosis and treatment plan.
Or the second doctor may suggest another approach.
Either way, you have more information and perhaps a
greater sense of control. You can feel more confident
about the decisions you make, knowing that you've
looked at your options.
It may take some time and effort to gather your
medical records and see another doctor. In most cases,
it's not a problem to take several weeks to get a second
opinion. The delay in starting treatment usually won't
make treatment less effective. To make sure, you
should discuss this delay with your doctor. Some
people with multiple myeloma need treatment right
away.
There are many ways to find a doctor for a second
opinion. You can ask your doctor, a local or state
medical society, a nearby hospital, or a medical school
for names of specialists. NCI's Cancer Information
Service at 1-800-4-CANCER can tell you about
nearby treatment centers. Other sources can be found
in the NCI fact sheet How To Find a Doctor or Treatment Facility If You Have Cancer.
Nonprofit groups with an interest in multiple
myeloma may be of help. Such groups are listed in the
NCI fact sheet National Organizations That Offer Services to People With Cancer and Their Families.
Back to Top
Supportive Care
Multiple myeloma and its treatment can lead to other health problems. At any stage of the disease, you can have supportive care.
Supportive care is treatment to prevent or fight
infections, to control pain and other symptoms, to
relieve the side effects of therapy, and to help you cope
with the feelings that a diagnosis of cancer can bring.
You may receive supportive care to prevent or control
these problems and to improve your comfort and
quality of life during treatment.
You can get information about supportive care
on NCI's Web site at http://www.cancer.gov/cancerinfo/coping and from NCI's Cancer Information Service at 1-800-4-CANCER or
LiveHelp
(http://www.cancer.gov/help).
Because people with multiple myeloma get
infections very easily, you may receive antibiotics and
other drugs.
Some people receive vaccines against the flu and
pneumonia. You may want to talk with your health care
team about when to get certain vaccines.
The health care team may advise you to stay away
from crowds and from people with colds and other
contagious diseases. If an infection develops, it can be
serious and should be treated promptly. You may need
to stay in the hospital for treatment.
Myeloma and its treatment can lead to anemia,
which may make you feel very tired. Drugs or a blood
transfusion can help with this problem.
Multiple myeloma often causes bone pain. Your
health care provider can suggest ways to relieve or
reduce pain:
- A brace that relieves pain in the neck or back
- Drugs that fight pain anywhere in the body
- Radiation therapy from a large machine aimed at
the bone
- Surgery to fix a compressed (squeezed) spinal cord
Some people get pain relief from massage or
acupuncture when used along with other approaches.
Also, you may learn relaxation techniques such as
listening to slow music or breathing slowly and
comfortably.
You may find it helpful to read the NCI booklet Pain Control.
Myeloma cells keep new bone cells from forming,
and bones become thin wherever there are myeloma
cells. Your doctor may give you drugs to prevent bone
thinning and help reduce the risk of fractures. Physical
activity, such as walking, also helps keep bones strong.
Multiple myeloma may cause calcium to leave the
bones and enter the bloodstream. If you have a very
high level of calcium in your blood, you may lose your
appetite. You also may feel nauseated, restless, or
confused. A high calcium level can also make you very
tired, weak, dehydrated, and thirsty. Drinking a lot of
fluids and taking drugs that lower the calcium in the
blood can be helpful.
Some people with multiple myeloma have kidney
problems. If the problems are severe, a person may
need dialysis. Dialysis removes wastes from the blood.
A person with serious kidney problems may need a
kidney transplant.
Some people with myeloma develop amyloidosis.
This problem is caused by abnormal proteins collecting
in tissues of the body. The buildup of proteins can
cause many problems, some of them severe. For
example, proteins can build up in the heart, causing
chest pain and swollen feet. There are drugs to treat
amyloidosis.
Back to Top
Nutrition and Physical Activity
It's important for you to take care of yourself by
eating well, drinking plenty of fluids, and staying as
active as you can.
You need the right amount of calories to maintain a
good weight. You also need enough protein to keep up
your strength. Eating well may help you feel better and
have more energy.
However, you may not feel like eating during
treatment or soon after. You may be uncomfortable or
tired. You may find that foods do not taste as good as
they used to. In addition, the side effects of treatment
(such as poor appetite, nausea, vomiting, or mouth
sores) can make it hard to eat well. Your doctor, a
registered dietitian, or another health care provider can
suggest ways to deal with these problems. Also, the
NCI booklet Eating Hints for Cancer Patients has
many useful ideas and recipes.
Research shows that people with cancer feel better
when they are active. Walking, yoga, swimming, and
other activities can keep you strong and increase your
energy. Exercise may reduce nausea and pain and make
treatment easier to handle. It also can help relieve
stress. Whatever physical activity you choose, be sure
to talk to your doctor before you start. Also, if your
activity causes you pain or other problems, be sure to
let your doctor or nurse know about it.
Back to Top
Follow-up Care
You'll need regular checkups after treatment for
multiple myeloma. Checkups help ensure that any
changes in your health are noted and treated if needed.
If you have any health problems between checkups,
you should contact your doctor.
Your doctor will check for return of cancer. Even
when the cancer seems to have been completely
destroyed, the disease sometimes returns because
undetected myeloma cells remained somewhere in the
body after treatment. Also, checkups help detect health
problems that can result from cancer treatment.
Checkups may include a careful physical exam,
blood tests, x-rays, or bone marrow biopsy.
The NCI has publications to help answer questions
about follow-up care and other concerns. You may find
it helpful to read the NCI booklet Facing Forward: Life After Cancer Treatment. You may also want to read the NCI fact sheet Follow-up Care After Cancer Treatment: Questions and Answers.
|
You may want to ask your doctor these questions after you have finished treatment:
- How often will I need checkups?
- Which follow-up tests do you suggest for me?
- Between checkups, what health problems or
symptoms should I tell you about?
|
Back to Top
Sources of Support
Learning you have myeloma can change your life
and the lives of those close to you. These changes can
be hard to handle. It's normal for you, your family, and
your friends to have new and confusing feelings to
work through.
Concerns about treatments and managing side
effects, hospital stays, and medical bills are common.
You may also worry about caring for your family,
keeping your job, or continuing daily activities.
Here's where you can go for support:
- Doctors, nurses, and other members of your health
care team can answer many of your questions about
treatment, working, or other activities.
- Social workers, counselors, or members of the
clergy can be helpful if you want to talk about your
feelings or concerns. Often, social workers can
suggest resources for financial aid, transportation,
home care, or emotional support.
- Support groups can also help. In these groups,
patients or their family members meet with other
patients or their families to share what they have
learned about coping with the disease and the effects
of treatment. Groups may offer support in person,
over the telephone, or on the Internet. You may want
to talk with a member of your health care team
about finding a support group.
- Information specialists at 1-800-4-CANCER and
at
LiveHelp (http://www.cancer.gov/help) can help
you locate programs, services, and publications.
They can give you names of national organizations
that offer services to people with cancer and their
families.
For tips on coping, you may want to read the NCI
booklet Taking Time: Support for People With Cancer.
Back to Top
Taking Part in Cancer Research
Doctors all over the country are conducting many
types of clinical trials (research studies in which people
volunteer to take part). Clinical trials are designed to
answer important questions and to find out whether
new approaches are safe and effective.
Research already has led to advances in treatment,
such as stem cell transplants. And doctors continue to
look for better ways to treat myeloma.
Researchers are testing new drugs and drug
combinations. They are also testing ways to improve
stem cell transplants for people with multiple
myeloma.
Even if people in a trial do not benefit directly, they
still make an important contribution by helping doctors
learn more about myeloma and how to control it.
Although clinical trials may pose some risks, doctors
do all they can to protect their patients.
If you are interested in being part of a clinical trial,
talk with your doctor. You may want to read the NCI
booklet Taking Part in Cancer Treatment Research Studies. This booklet describes how treatment studies
are carried out and explains their possible benefits and
risks.
NCI's Web site includes a section on clinical trials
at http://www.cancer.gov/clinicaltrials. It has
general information about clinical trials as well as
detailed information about specific ongoing studies
of myeloma. Information specialists at
1-800-4-CANCER or at
LiveHelp at
http://www.cancer.gov/help can answer questions and
provide information about clinical trials.
Back to Top
National Cancer Institute Information Resources
You may want more information for yourself, your
family, and your doctor. The following NCI services
are available to help you.
NCI's Cancer Information Service (CIS) provides
accurate, up-to-date information about cancer to
patients and their families, health professionals, and the
general public. Information specialists translate the
latest scientific information into plain language, and
they will respond in English or Spanish, as well as
through TRS providers for the hearing or speech
impaired. Calls to the CIS are confidential and free.
Telephone: 1-800-4-CANCER (1-800-422-6237)
NCI's Web site provides information from numerous
NCI sources. It offers current information about cancer
prevention, screening, diagnosis, treatment, genetics,
supportive care, and ongoing clinical trials. It has
information about NCI's research programs, funding
opportunities, and cancer statistics.
Web site: http://www.cancer.gov
Spanish Web site: http://www.cancer.gov/espanol
If you're unable to find what you need on the Web
site, contact NCI staff. Use the online contact form at
http://www.cancer.gov/contact or send an email to
cancergovstaff@mail.nih.gov.
Also, information specialists provide live,
online assistance through
LiveHelp at
http://www.cancer.gov/help.
Back to Top
National Cancer Institute Publications
NCI provides publications about cancer, including
the booklets and fact sheets mentioned in this booklet.
Many are available in both English and Spanish.
You may order these publications by telephone, on
the Internet, or by mail. You may also read them online
and print your own copy.
- By telephone: People in the United States and its
territories may order these and other NCI
publications by calling the NCI's Cancer
Information Service at 1-800-4-CANCER.
- On the Internet: Many NCI publications may be
viewed, downloaded, and ordered from
http://www.cancer.gov/publications on the
Internet. People in the United States and its
territories may use this Web site to order printed
copies. This Web site also explains how people
outside the United States can mail or fax their
requests for NCI booklets.
- By mail: NCI publications may be ordered by
writing to the address below:
Publications Ordering Service
National Cancer Institute
P.O. Box 24128
Baltimore, MD 21227
Taking Part in Cancer Treatment Research Studies
How To Find a Doctor or Treatment Facility If You Have Cancer (also in Spanish:
 Cómo encontrar a un doctor o un establecimiento de tratamiento si usted tiene cáncer
Cómo encontrar a un doctor o un establecimiento de tratamiento si usted tiene cáncer)
Cancer Support Groups: Questions and Answers
National Organizations That Offer Services to People With Cancer and Their Families (also in
Spanish:
 Organizaciones nacionales que brindan servicios a las personas con cáncer y a sus familias
Organizaciones nacionales que brindan servicios a las personas con cáncer y a sus familias)
Chemotherapy and You (also in Spanish:
La quimioterapia y usted)
Targeted Cancer Therapies: Questions and Answers
Radiation Therapy and You (also in Spanish:
La radioterapia y usted)
Bone Marrow Transplantation and Peripheral Blood Stem Cell Transplantation: Questions and Answers

(also in Spanish:
El trasplante de médula ósea y el trasplante de células madre de sangre periférica)
Eating Hints for Cancer Patients (also in Spanish:
 Consejos de alimentación para pacientes con cáncer: Antes, durante y después del tratamiento
Consejos de alimentación para pacientes con cáncer: Antes, durante y después del tratamiento)
Pain Control (also in Spanish:
Apoyo para las personas con cáncer: Control del dolor)
Taking Time: Support for People with Cancer
Follow-up Care After Cancer Treatment: Questions and Answers
Facing Forward: Life After Cancer Treatment (also
in Spanish:
Siga adelante: la vida después del tratamiento del cáncer)
Facing Forward: Ways You Can Make a Difference in Cancer
Coping With Advanced Cancer
When Cancer Returns
Thinking about Complementary & Alternative Medicine: A guide for people with cancer
Complementary and Alternative Medicine in Cancer Treatment: Questions and Answers

(also in Spanish:
La medicina complementaria y alternativa en el tratamiento del cáncer: preguntas y respuestas)
When Someone You Love Is Being Treated for Cancer: Support for Caregivers
When Someone You Love Has Advanced Cancer: Support for Caregivers
Facing Forward: When Someone You Love Has Completed Cancer Treatment
Caring for the Caregiver: Support for Cancer Caregivers
Back to Top