Trace Elements: Iodine
Background
Iodine, a trace element found in soil, is an essential component of the thyroid hormones involved in regulating the body’s metabolic processes. Iodized salt and seafood are the major dietary sources of iodine. In the United States, salt is iodized with potassium iodide at 100 parts per million (76 milligram [mg] of iodine per kilogram [kg] of salt). Iodized salt is chosen by about 50–60 percent of the U.S. population (Institute of Medicine 2001). Still, most ingested salt comes from processed food (approximately 70 percent), which is typically not iodized in either the United States or in Canada (The Public Health Committee of the American Thyroid Association 2006).
For the thyroid to synthesize thyroid hormones, iodine is essential. Iodine deficiency disorders include mental retardation, hypothyroidism, goiter, cretinism, and varying degrees of other growth and developmental abnormalities. Iodine deficiency is the most preventable cause of mental retardation in the world (World Health Organization 2007). Thyroid enlargement (goiter) is usually the earliest clinical feature of iodine deficiency. Thyroid hormone is particularly important in the development of the central nervous system during the fetal and early postnatal periods. In areas where iodized salt is common, iodine deficiency is rare.
The median intake of iodine from food in the United States is approximately 240 to 300 micrograms (µg) per day for men and 190 to 210 µg/day for women, largely owing to the iodization of salt (Institute of Medicine 2001). Iodine deficiency develops when iodide intake is less than 20 μg/day (Beers 2006). Most dietary iodine absorbed in the body eventually appears in the urine; thus, urinary iodine excretion is recommended for assessing recent dietary iodine intake worldwide (World Health Organization 2007).
Excess iodine intake may also result in goiter, as well as in hyper- or hypothyroidism. High iodine intake has also been associated with increased risk for thyroid papillary cancer (Institute of Medicine 2001). For most people, iodine intake from usual foods and supplements is unlikely to exceed the tolerable upper intake level (1,100 μg/day).
The Institute of Medicine recommends iodine intake at 150 µg per day for nonpregnant adults, 220 µg per day for pregnant women and 290 µg per day during lactation (Institute of Medicine 2001).
World Health Organization (WHO) categories for median urinary iodine concentrations in school-age children and adults (excluding pregnant and lactating women) are widely used to define iodine intake and nutrition status for populations (World Health Organization 2007) (Table 4.a). An additional adequacy criterion is that not more than 20 percent of samples from children and non-pregnant women are below 50 nanograms per milliliter (ng/mL) of iodine.
Table 4.a
Epidemiological criteria for assessing iodine nutrition based on median urinary iodine concentrations of school-age children (≥ 6 years)*
Median Urinary Iodine (ng/mL) |
Iodine Intake |
Iodine Status |
< 20 |
Insufficient |
Severe iodine deficiency |
20–49 |
Insufficient |
Moderate iodine deficiency |
50–99 |
Insufficient |
Mild iodine deficiency |
100–199 |
Adequate |
Adequate iodine nutrition |
200–299 |
Above requirements |
Likely to provide adequate intake for pregnant/lactating women but may pose a slight risk of more than adequate intake in the overall population |
> 300 |
Excessive |
Risk for adverse health consequences (e.g., iodine-induced hyperthyroidism, autoimmune thyroid diseases) |
*Applies to adults but not to pregnant and lactating women
Note that these categories are useful for classifying population risk but are not categories to define individual risk for adverse health outcomes. The large day-to-day variations in urine iodine excretion, even among individuals with stable iodine intake, tend to offset one another when the sample includes an adequately large number (50–100 people per site) of representative individuals (Borak 2005).
For pregnant women, median urinary iodine concentrations of 150–249 ng/mL represent adequate iodine intake (World Health Organization 2007).
The Public Health Committee of the American Thyroid Association (2006) has recommended that until additional physiologic data are available to determine the appropriate requirements during pregnancy and lactation, iodine supplementation (150 μg/day) is appropriate for these two life stages in the United States and in Canada. This decision was based on data for pregnant women from NHANES III and NHANES 2001–2002: median urinary iodine concentrations were lower than recommended during NHANES III (141 ng/mL) and within the recommended range during NHANES 2001–2002 (173 ng/mL), but 95 percent confidence intervals ranged from 75 to 229 ng/mL (Caldwell 2005).
More information on iodine is available online:
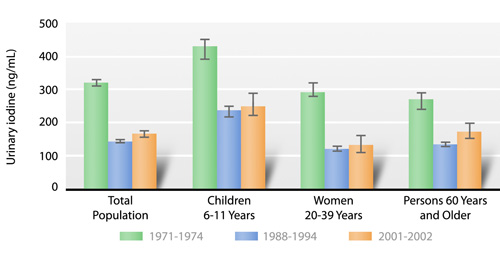
Since 1971, NHANES has measured urinary iodine. The NHANES III survey (1988–1994) showed a sizable decrease in urinary iodine concentrations compared with concentrations measured during NHANES I (1971–1974) (Hollowell 1998). This decline may have been due to the dairy industry’s effort in the mid-1980s to reduce the iodine residue in milk from feed supplements and iodophor sanitizing agents (Pennington 1996). Decreased concentrations of iodine in fruit-flavored breakfast cereals—the industry’s response to a ban on erythrosine (an iodine-containing food dye)—could also have contributed to the decline in urinary iodine concentrations (Pennington 1996). Since 2000, urinary iodine has been measured in the continuous NHANES survey. CDC uses a new method, involving inductively coupled plasma mass spectrometry (ICP-MS), to make these measurements (Caldwell 2003). This method has been compared with the established Sandell-Kolthoff spectrophotometric method used in NHANES III (Pino 1998). The two methods strongly correlate (r2 = 0.98), and the average difference between them is not statistically significant (Caldwell 2003). When CDC laboratory scientists used this new method to measure urinary iodine concentrations in NHANES 2000 (U.S. Centers for Disease Control and Prevention 2000) and NHANES 2001–2002 (Caldwell 2005), they found that the U.S. median urinary iodine concentration had stabilized since the initial drop that had occurred from NHANES I to NHANES III. This finding confirms the stability of the U.S. iodine intake and continued adequate iodine nutrition for the country generally.
Selected Observations and Highlights
The following example observations and figures are taken from the uncorrected tables of 2001–2002 data contained in this report. Statements about categorical differences between demographic groups noted below are based on non-overlapping confidence limits from univariate analysis without adjusting for demographic variables (i.e., age, sex, race/ethnicity) or other determinants of these urine concentrations (i.e., dietary intake, supplement usage, smoking, BMI). A multivariate analysis may alter the size and statistical significance of these categorical differences. Furthermore, additional significant differences of smaller magnitude may be present despite their lack of mention here (e.g., if confidence limits slightly overlap or if differences are not statistically significant before covariate adjustment has occurred). For a selection of citations of descriptive NHANES papers related to these biochemical indicators of diet and nutrition, see Appendix E.
General Observations
- Children (aged 6–11 years) have higher urinary iodine concentrations than people in any other age group.
- Females have lower urinary iodine concentrations than males.
Highlights
After a sharp decline that occurred from 1971–1988, from 1988–2002 median concentrations of urinary iodine appear to have stabilized in various population subgroups (Fig 4.a). This finding has been shown previously (Caldwell 2005).
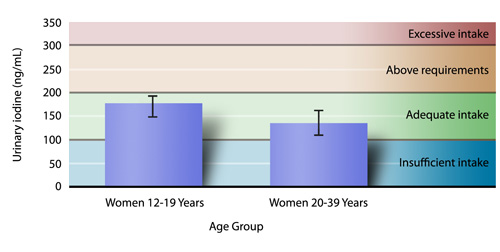
On the basis of median urinary iodine concentrations, the iodine intake of women of childbearing age appears adequate (Fig 4.b). Appropriate consideration should be given, however, to the higher intake recommendation for pregnant women (World Health Organization 2007).
| Figure 4.b
Median concentrations (95 percent confidence intervals) of urinary iodine among women of childbearing age, National Health and Nutrition Examination Survey, 2001–2002. |
Tables
Urinary iodine
- Table 4.1.a. Urinary iodine: Total population
- Table 4.1.b. Urinary iodine: Mexican Americans
- Table 4.1.c. Urinary iodine: Non-Hispanic blacks
- Table 4.1.d. Urinary iodine: Non-Hispanic whites
Urinary iodine (creatinine corrected)
- Table 4.1.e. Urinary iodine: Total population (creatinine corrected)
- Table 4.1.f. Urinary iodine: Mexican Americans (creatinine corrected)
- Table 4.1.g. Urinary iodine: Non-Hispanic blacks (creatinine corrected)
- Table 4.1.h. Urinary iodine: Non-Hispanic whites (creatinine corrected)
References
Beers MH, editor. Vitamin deficiency, dependency, and toxicity. In: Merck Manual of Diagnosis and Therapy. 18th ed. Whitehouse Station (NJ): Merck & Co., Inc.; 2006 [cited 2008]. Available from: http://www.merck.com/mmpe/sec01/ch005/ch005e.html.
Borak J. Adequacy of iodine nutrition in the United States. Conn Med. 2005;69:73-7.
Caldwell KL, Maxwell B, Makhmudov A, Pino S, Braverman LE, Jones RL, Hollowell JG. Use of inductively coupled plasma mass spectrometry to measure urinary iodine in NHANES 2000: comparison with previous method. Clin Chem. 2003;49:1019-21.
Caldwell KL, Jones R, Hollowell JG. Urinary iodine concentration: United States National Health and Nutrition Examination Survey 2001–2002. Thyroid. 2005;15:692-9.
Hollowell JG, Staehling NW, Hannon WH, Flanders DW, Gunter EW, Maberly GF, et al. Iodine nutrition in the United States. Trends and public health implications: iodine excretion data from National Health and Nutrition Examination Surveys, I and III (1971–1974 and 1988–1994). J Clin Endocrinol Metab. 1998;83:3401-8.
Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes: vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. Washington, D.C.: National Academy Press; 2001.
Pennington JAT, Schoen SA. Total Diet Study: estimated dietary intakes of nutritional elements, 1982–1991. Int J Vit Nutr Res. 1996;66:350-62.
Pino S, Fang SL, Braverman LE. Ammonium persulfate: a new and safe method for measuring urinary iodine by ammonium persulfate oxidation. Exp Clin Endocrinol Diabetes. 1998;106 Suppl 3:S22-7.
The Public Health Committee of the American Thyroid Association. Iodine supplementation for pregnancy and lactation — United States and Canada: recommendations of the American Thyroid Association. Thyroid. 2006;16:949-51.
U.S. Centers for Disease Control and Prevention: iodine level, United States, 2000 [cited 2008]. National Center for Health Statistics. Available from: http://www.cdc.gov/nchs/products/pubs/pubd/hestats/iodine.htm.
World Health Organization. Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers. 3rd ed. Geneva (Switzerland): World Health Organization, 2007 (WHO/NHD/01.1) [cited 2008]. Available from: http://www.whqlibdoc.who.int/publications/2007/9789241595827_eng.pdf.
Related Links
- American Society for Nutrition
Iodine Fact Sheet*
- Institute of Medicine Dietary Reference Intakes
Iodine Report*
* Links to non-Federal organizations found at this site are provided solely as a service to our users. These links do not constitute an endorsement of these organizations or their programs by CDC or the Federal Government, and none should be inferred. CDC is not responsible for the content of the individual organization Web pages found at these links.
- Page last reviewed: July 30, 2008
- Page last updated: July 30, 2008
- Content source: Centers for Disease Control and Prevention, National Center for Environmental Health, Division of Laboratory Sciences
Contact Us:
- Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348
24 Hours/Every Day - cdcinfo@cdc.gov