|
|
|
Management
of Hepatitis C: 2002 National
Institutes of Health
NIH Consensus and State-of-the-Science statements are prepared by independent panels of health professionals and public representatives on the basis of (1) the results of a systematic literature review prepared under contract with the Agency for Healthcare Research and Quality (AHRQ), (2) presentations by investigators working in areas relevant to the conference questions during a 2-day public session, (3) questions and statements from conference attendees during open discussion periods that are part of the public session, and (4) closed deliberations by the panel during the remainder of the second day and morning of the third. This statement is an independent report of the panel and is not a policy statement of the NIH or the Federal Government. The statement reflects the panel's assessment of medical knowledge available at the time the statement was written. Thus, it provides a "snapshot in time" of the state of knowledge on the conference topic. When reading the statement, keep in mind that new knowledge is inevitably accumulating through medical research, and that the information provided is not a substitute for professional medical care or advice. Introduction The hepatitis C virus (HCV) is one of the leading known causes of liver disease in the United States. It is a common cause of cirrhosis and hepatocellular carcinoma (HCC) as well as the most common reason for liver transplantation. At least 4 million people in this country are believed to have been infected with HCV. Following the identification of hepatitis A and hepatitis B, this disorder was categorized in 1974 as "non-A, non-B hepatitis." In 1989, the hepatitis C virus was identified and found to account for the majority of those patients with non-A, non-B hepatitis. In March 1997, the National Institutes of Health (NIH) held a Consensus Development Conference regarding management and treatment of HCV infection. This led to an important, widely distributed NIH Consensus Statement that, for several years, defined the standard of care. Now 5 years later, knowledge of hepatitis C has increased dramatically, leading to the need to reexamine the approaches to management and treatment. This conference was convened with the aim of reviewing the most recent developments regarding management, treatment options, and the widening spectrum of potential candidates for treatment and of updating the 1997 Consensus Statement. This NIH Consensus Development Conference on Management of Hepatitis C: 2002 was held June 10&endash;12, 2002. The primary sponsors of this meeting were the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the Office of Medical Applications of Research (OMAR) of the NIH. The cosponsors were the National Institute of Child Health and Human Development (NICHD); the National Cancer Institute (NCI); the National Center for Complementary and Alternative Medicine (NCCAM); the National Institute on Alcohol Abuse and Alcoholism (NIAAA); the National Institute on Drug Abuse (NIDA); the National Institute of Allergy and Infectious Diseases (NIAID); the National Heart, Lung, and Blood Institute (NHLBI); the Centers for Medicare & Medicaid Services (CMS); the Centers for Disease Control and Prevention (CDC); the U.S. Food and Drug Administration (FDA); and the U.S. Department of Veterans Affairs (VA). The Agency for Healthcare Research and
Quality (AHRQ) provided support to the NIH Consensus Development
Conference on Management of Hepatitis C: 2002 through its Evidence-based
Practice Center program. Under contract to the AHRQ, the Johns Hopkins
University Evidence-based Practice Center developed the systematic review
and analysis that served as a reference for discussion at the Conference.
On the final day of the conference, the panel chairperson read the draft statement to the conference audience and invited comments and questions. A press conference followed to allow the panel and chairperson to respond to questions from the media. The Consensus Development Panel's draft
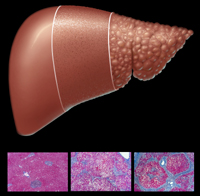
statement was posted to the Consensus Program Web site http://consensus.nih.govÐon
Wednesday, June 12, 2002. 1. What is the natural history of hepatitis C?The VirusHCV is an RNA virus of the Flaviviridae family. There are 6 HCV genotypes and more than 50 subtypes. These genotypes differ by as much as 31 to 34 percent in their nucleotide sequences, whereas subtypes differ by 20 to 23 percent based on full-length genomic sequence comparisons. The lack of a vigorous T-lymphocyte response and the high propensity of the virus to mutate appear to promote a high rate of chronic infection. The extensive genetic heterogeneity of HCV has important diagnostic and clinical implications, perhaps explaining difficulties in vaccine development and the lack of response to therapy. Genotype 1 accounts for 70 to 75 percent of all HCV infections in the United States and is associated with a lower rate of response to treatment. HCV replicates preferentially in hepatocytes but is not directly cytopathic, leading to persistent infection. During chronic infection, HCV RNA reaches high levels, generally ranging from 105 to 107 international units (IU)/mL, but the levels can fluctuate widely. However, within the same individual, RNA levels are usually relatively stable. EpidemiologyAccording to the National Health and Nutrition Examination Survey (NHANES) of 1988&endash;1994, 3.9 million Americans were infected with HCV, and of this group, 2.7 million were estimated to have chronic infection. Because NHANES is a population-based household survey, it does not include certain groups with a substantially increased prevalence of infection, such as persons who are incarcerated, homeless, or institutionalized. Although difficult to assess accurately, the incidence of HCV infections declined sharply in the late 1980s. Currently, approximately 35,000 new HCV infections are estimated to occur each year. However, the estimated prevalence of HCV in the United States is at least 1.8 percent of the population, making HCV the most common chronic blood-borne infection nationally. Because most persons with chronic HCV infection have yet to be diagnosed but are likely to come to medical attention in the next decade, a fourfold increase in the number of adults diagnosed with chronic HCV infection is projected from 1990 to 2015. Currently, persons aged 40 to 59 years have the highest prevalence of HCV infection, and in this age group, the prevalence is highest in African Americans (6.1 percent). HCV transmission occurs primarily through exposure to infected blood. This exposure exists in the context of injection drug use, blood transfusion before 1992, solid organ transplantation from infected donors, unsafe medical practices, occupational exposure to infected blood, birth to an infected mother, sex with an infected person, high-risk sexual practices, and possibly intranasal cocaine use.Transmission from blood products and organ transplants was virtually eliminated by the introduction of a more sensitive test for antibody to HCV (anti-HCV) in mid-1992. High HCV seroprevalence rates (from 15 to 50 percent) have occurred in specific subpopulations, such as the homeless, incarcerated persons, injection drug users, and persons with hemophilia who were treated with clotting factors before 1992. The highest seroprevalence rates (70 percent to more than 90 percent) have been reported in the last two of these groups. Acute InfectionAfter initial exposure, HCV RNA can be detected in blood within 1 to 3 weeks and is present at the onset of symptoms. Antibodies to HCV are detected by enzyme immunoassay (EIA) in only 50 to 70 percent of patients at the onset of symptoms, increasing to more than 90 percent after 3 months. Within an average of 4 to 12 weeks, liver cell injury is manifested by elevation of serum alanine aminotransferase (ALT) levels. Acute infection can be severe but rarely is fulminant. Symptoms are uncommon but can include malaise, weakness, anorexia, and jaundice. Symptoms usually subside after several weeks as ALT levels decline. Chronic InfectionPersistence of HCV infection is diagnosed by the detection of HCV RNA in the blood for at least 6 months. In general, prospective studies have shown that 60 to 85 percent of HCV-infected persons develop chronic infection. Factors associated with spontaneous clearance of HCV infection appear to include younger age, female gender, and certain major histocompatability complex genes. African American men appear to be least likely to spontaneously clear the virus. The most important sequelae of chronic HCV infection are progressive liver fibrosis leading to cirrhosis, end-stage liver disease, and HCC. Estimates of the proportion of chronically infected persons who develop cirrhosis 20 years after initial infection vary widely from 2 to 4 percent in studies of children and young women to as high as 20 to 30 percent in middle-aged transfused subjects. The actual risk is likely intermediate between these two ranges, on the order of 10 to 15 percent. There is little evidence that virologic factors, including viral load, viral genotype, and quasi-species diversity significantly affect the risk of progression of liver disease. However, many host factors increase this risk, including older age at time of infection, male gender, and an immunosuppressed state such as that associated with human immunodeficiency virus (HIV) infection. Concurrent chronic hepatitis B also appears to increase the risk of progressive liver disease. In addition, higher levels of alcohol use play an important role in promoting the development of progressive liver disease, with strong evidence for the detrimental effects of 30 g/day in men (~ equivalent to 2 beers, 2 glasses of wine, or 2 mixed drinks) and 20 g/day in women. Lower amounts of alcohol also may increase the risk of liver damage associated with HCV. Other factors, including iron overload, nonalcoholic fatty liver disease, schistosomal co-infection, potentially hepatotoxic medications, and environmental contaminants, also may have important effects. In the United States, deaths associated with chronic hepatitis C are currently more likely to be due to decompensated cirrhosis than to HCC. Data from death certificates suggest that there are 10,000 to 12,000 deaths yearly in the United States due to hepatitis C, but these may be underestimates. The only treatment option for persons who have developed decompensated cirrhosis is liver transplantation. Currently, HCV is the primary reason for liver transplantation in the United States. Little is known about the clinical course and risks of HCV-related complications in persons who have been infected for longer than two decades. HCV accounts for an estimated one-third of HCC cases in the United States. HCC rarely occurs in the absence of cirrhosis or advanced fibrosis. The incidence of HCV-related HCC continues to rise in United States and worldwide, in part because of the increasing numbers of persons who have been chronically infected for decades, the presence of comorbid factors, and the longer survival of persons with advanced liver disease due to improved management of complications. Risk factors for HCC in persons with chronic HCV infection are largely the same as those for the development of decompensated cirrhosis. Some but not all studies suggest that treatment with interferon and ribavirin may reduce the risk of developing HCC in HCV patients with cirrhosis, but more data are needed. Extrahepatic Manifestations of HCV InfectionPatients with chronic hepatitis C can present with extrahepatic manifestations or syndromes considered to be of immunologic origin, such as rheumatoid symptoms, keratoconjunctivitis sicca, lichen planus, glomerulonephritis, lymphoma, and essential mixed cryoglobulinemia. Cryoglobulins have been detected in the serum of up to one-half of patients with chronic hepatitis C, but the clinical features of mixed cryoglobulinemia are uncommon. Chronic hepatitis C is also related to porphyria cutanea tarda. Psychological disorders including depression have been associated with HCV infection in up to 20 to 30 percent of cases. 2. What is the most appropriate approach to diagnose and monitor patients?Various tests are available for the diagnosis and monitoring of HCV infection. Tests that detect antibodies against the virus include the enzyme immunoassay (EIA), which contains HCV antigens from the core and nonstructural genes, and the recombinant immunoblot assay. The same HCV antigens are used in both EIAs and the immunoblot assays. Target amplification techniques using either polymerase chain reaction (PCR) or transcription-mediated amplification (TMA) have been developed as qualitative tests for HCV RNA, whereas both target amplification (PCR) and signal amplification techniques (branched DNA) may be used to measure HCV RNA levels. Liver biopsy can provide direct histologic assessment of liver injury due to HCV but cannot be used to diagnose HCV infection. HCV Serologic Assays EIA tests are reproducible, inexpensive, and FDA-approved for use in the diagnosis of HCV infection. They are suitable for screening at-risk populations and are recommended as the initial test for patients with clinical liver disease. The very high sensitivity and specificity of the version 3 (third-generation) EIAs (sensitivity of greater than 99 percent, specificity of 99 percent in immunocompetent patients) obviate the need for a confirmatory immunoblot assay in the diagnosis of individual patients with clinical liver disease, particularly those with risk factors for HCV infection. A negative EIA test is sufficient to exclude a diagnosis of chronic HCV infection in immune-competent patients. Rarely, patients on hemodialysis and patients with immune deficiencies may have false-negative EIAs. Conversely, false-positive EIAs may occur in patients with autoimmune disorders. In these patients, an assay for HCV RNA is necessary for diagnosis of chronic infection. The immunoblot assay is still useful as a supplemental assay for persons screened in nonclinical settings and in persons with a positive EIA who test negative for HCV RNA. Qualitative HCV RNA Assays Acute or chronic HCV infection in a patient with a positive EIA test should be confirmed by a qualitative HCV RNA assay with a lower limit of detection of 50 IU/mL or less (approximately 100 viral genes/mL). However confirmation may be unnecessary in a patient who has evidence of liver disease and obvious risk factors for HCV infection. The FDA-approved manual and semiautomated, qualitative, HCV PCR assays have a lower limit of detection of 50 to 100 IU/mL. More recently, a transcription-mediated amplification assay has been developed with a lower limit of detection on the order of 5 to 10 IU/mL, but it has yet to be approved for use by the FDA. The specificity of these assays for detecting HCV RNA exceeds 98 percent. A single positive qualitative assay for HCV RNA confirms active HCV replication, but a single negative assay does not exclude viremia and may reflect only a transient decline in viral level below the level of detection of the assay. A followup qualitative HCV RNA should be performed to confirm the absence of active HCV replication. Once HCV infection is confirmed, repeat testing using a qualitative assay with a limit of detection of 50 IU/mL or less is not helpful in the management of untreated patients, except for determining whether an acute infection has resolved spontaneously. Until future studies determine whether the sustained virological response (SVR) will be sustained over the long term following successful antiviral treatment, periodic measurements of HCV RNA may need to be performed. Quantitative HCV RNA Assays Testing for HCV RNA level (or viral load) with a quantitative assay such as quantitative PCR (qPCR) or branched DNA (bDNA) signal amplification assay provides accurate information on HCV viral levels. An HCV RNA standard has been introduced to permit normalization of reported viral titers in IUs. The reported IU does not represent the actual number of viral particles in a preparation. Significant variability exists between available assays. The reportable range, accuracy, and precision of each assay needs to be monitored, and appropriate dilutions of sample material should be performed to obtain accurate quantitative results. The clinical utility of serial HCV viral levels in a patient is predicated on continued use of the same specific quantitative assay that was used in the initial determination of the viral level. While there is little correlation between disease severity or disease progression with the absolute level of HCV RNA, quantitative determination of the HCV level provides important information on the likelihood of response to treatment in patients undergoing antiviral therapy. In clinical trials of combination interferon and ribavirin reported to date, a positive response to antiviral therapy in patients infected with all common genotypes (genotypes 1, 2, and 3) has been correlated with low viral levels. ALT Testing for serum ALT levels is the most inexpensive and noninvasive, but relatively insensitive, means of assessing disease activity. A single determination of ALT level gives limited information about the severity of the underlying liver disease. In most studies, a weak association exists between the degree of ALT elevation and severity of the histopathological findings on liver biopsy. Serial determinations of ALT levels over time may provide a better means of assessing liver injury, but the accuracy of this approach has not been well documented. Patients who initially have a normal ALT level should undergo serial measurements over several months to confirm the persistence of normal ALT levels. Although loss or reduction in HCV RNA is the primary indicator of response to antiviral therapy, the resolution of elevated ALT levels with antiviral therapy appears to be an important indicator of disease response. Nevertheless, pegylated interferon can cause mild elevations of ALT during therapy, and ALT levels are insensitive in detecting disease progression to cirrhosis. Noninvasive Tests of Fibrosis Various noninvasive tests of hepatic fibrosis have been examined for monitoring patients with chronic HCV infection. These include routinely available laboratory tests, such as liver-associated chemistries, platelet count, and prothrombin time, as well as specific serum markers of fibrosis and inflammation not currently widely available or well validated. No single test or panel of serologic markers can provide an accurate assessment of intermediate stages of hepatic fibrosis. Similarly, quantitative tests of liver function and radiologic imaging of the liver are sensitive for diagnosing advanced cirrhosis but are not useful in assessing hepatic fibrosis and early cirrhosis. Liver Biopsy Liver biopsy provides a unique source of information on fibrosis and assessment of histology. Liver enzymes have shown little value in predicting fibrosis. Extracellular matrix tests can predict severe stages of fibrosis but cannot consistently classify intermediate stages of fibrosis. Moreover, only liver biopsy provides information on possible contributions of iron, steatosis, and concurrent alcoholic liver disease to the progression of chronic hepatitis C toward cirrhosis. Although unexpected etiologies of liver disease are rarely discovered on liver biopsies from patients undergoing evaluation of chronic hepatitis C, the information obtained on liver biopsy allows affected individuals to make more informed choices about the initiation or postponement of antiviral treatment. Thus, the liver biopsy is a useful part of the informed consent process. Adult or pediatric patients with persistently normal or slightly elevated ALT levels and minimal or no fibrosis on liver biopsy may be reassured of a favorable prognosis and decide to defer antiviral therapy in the light of treatment side effects. Since a favorable response to current antiviral therapy occurs in 80 percent of patients infected with genotype 2 or 3, it may not always be necessary to perform liver biopsy in these patients to make a decision to treat. The usefulness of a pretreatment liver biopsy in this group as well as those with other genotypes requires further study. In general, a baseline assessment of liver histology offers a valuable standard for subsequent comparisons. However, the appropriate interval for subsequent evaluations is yet to be determined. Hepatocellular Carcinoma Screening HCC complicates cirrhosis secondary to HCV. It is estimated that HCC occurs after the development of cirrhosis at a rate varying from 0 to 3 percent per year. Few studies have examined specific screening strategies for HCC in patients with advanced HCV. Alpha-fetoprotein (AFP) and ultrasound every 6 months were used in a single study of patients with cirrhosis secondary to HCV. Identification of HCC was not significantly increased in the screened population. The value of screening for AFP is uncertain because there are no available data to demonstrate the clinical impact of this screening on the management of HCC or associated mortality. Studies of the performance characteristics of AFP and hepatic ultrasound show that AFP has a poor sensitivity and a high rate of false-positive reactions. Hepatic ultrasound is more sensitive than AFP testing but is also more expensive, and it can lead to invasive and unnecessary evaluations of lesions (e.g., regenerative nodules, hemangiomas, hepatic cysts) that are not HCC. Despite the lack of evidence, screening for HCC with AFP testing and hepatic ultrasound at 6-month intervals is a common practice in the United States. However, such routine AFP or imaging screening should not be performed in patients with hepatitis C in the absence of cirrhosis because HCC is so rare in this group. There is a great need for carefully designed studies on the reliability and benefit of surveillance screening. HIV Screening Significant overlap exists for risk factors for HCV and HIV infections. Therefore, patients with documented HIV infection should be routinely screened for HCV infection. Patients with hepatitis C who are at risk for HIV infection should be offered testing for evidence of HIV infection with appropriate pretest and posttest counseling. 3. What is the most effective therapy for hepatitis C?Since the 1997 NIH Consensus Development Conference on the Management of Hepatitis C, several important therapeutic advances have occurred, particularly with combination therapy with ribavirin and the introduction of pegylated interferons. Combination therapy results in better treatment responses than monotherapy, but the highest response rates have been achieved with pegylated interferon in combination with ribavirin. Genotype determinations influence treatment decisions. Currently the best indicator of effective treatment is an SVR, defined by the absence of detectable HCV RNA in the serum as shown by a qualitative HCV RNA assay with lower limit of detection of 50 IU/mL or less at 24 weeks after the end of treatment. Treatment of Naive Patients Three large pivotal trials have examined the efficacy of pegylated interferon plus ribavirin in the treatment of chronic HCV infection. These trials excluded patients with decompensated cirrhosis and comorbid conditions. Overall, pegylated interferon plus ribavirin was more effective than standard interferon-ribavirin combination or pegylated interferon alone. SVR rates were similar with both forms of pegylated interferon (alfa-2a and alfa-2b) when used in combination with ribavirin. Factors associated with successful therapy included genotypes other than 1, lower baseline viral levels, less fibrosis or inflammation on liver biopsy, and lower body weight or body surface area. Among patients with genotypes 2 or 3, SVRs with standard interferon and ribavirin were comparable to those with pegylated interferon and ribavirin, and thus standard interferon and ribavirin could be used in treating patients with these genotypes. In two trials using pegylated interferon and ribavirin, SVR rates of 42 and 46 percent were achieved in patients with genotype 1 compared to rates of 76 and 82 percent in patients with genotypes 2 and 3. In a recent, as yet unpublished study, a 24-week course of pegylated interferon and ribavirin was found to be as effective as a 48-week course in patients with genotypes 2 and 3 (SVR rates of 73 to 78 percent), but not in patients with genotype 1 (SVR rates of 41% with 24 weeks and 51% with 48 weeks). Similarly, a reduced ribavirin dosage of 800 mg daily appeared to be adequate for patients with genotypes 2 and 3, but the higher, standard dosage of 1000 to 1200 mg daily yielded better response rates in patients with genotype 1. Thus, 24 weeks of treatment and an 800 mg dose of ribavirin appears to be sufficient for persons with genotypes 2 and 3, while patients with genotype 1 need 48 weeks of treatment and standard doses of ribavirin. Early viral response (EVR), defined as a minimum 2 log decrease in viral load during the first 12 weeks of treatment, is predictive of SVR and should be a routine part of monitoring patients with genotype 1. Patients who fail to achieve an EVR at week 12 of treatment have only a small chance of achieving an SVR even if therapy is continued for a full year. Treatment need not be extended beyond 12 weeks in these patients. Although an SVR is difficult to correlate with improved survival because of the necessity for long-term followup, the absence of detectable serum HCV RNA has been associated with resolution of liver injury, reduction in hepatic fibrosis, and a low likelihood of a relapse of the HCV infection. Additionally, in two large but uncontrolled long-term followup studies from Japan, SVR after interferon treatment was associated with a lower risk of HCC. Conversely, one observational Italian study with long-term followup found no difference in development of HCC between those with and without interferon treatment. Retreatment of Patients Selected patients who fail to achieve an SVR may benefit from re-treatment with pegylated interferon-based regimens. Decisions regarding re-treatment should be based on (1) previous type of response, (2) the previous therapy and the difference in potency of the new therapy, (3) the severity of the underlying liver disease, (4) viral genotype and other predictive factors for response, and (5) tolerance of previous therapy and adherence. "Relapsers" achieve an initial end of treatment response (ETR) for their HCV disease, but this is not sustained over time (i.e., no SVR). "Nonresponders" never achieve an ETR or an SVR. Some nonresponders achieve a substantial reduction of HCV RNA (1 log unit or more) during therapy and can be categorized as partial responders. Even in the absence of SVR, treatment may be associated with improved histology. In one study only nonresponders who had a decline in HCV RNA to an absolute level of <100,000 copies/mL during the original treatment with interferon alone achieved an SVR when re-treated with interferon and ribavirin. Preliminary results suggest that, overall, only 15 to 20 percent of nonresponders treated with standard interferon-ribavirin combinations achieved an SVR on re-treatment using pegylated interferon with ribavirin. Patients with genotypes 2 or 3 have better response rates to re-treatment than those with genotype 1. Studies are currently being conducted with pegylated interferon and ribavirin therapy in patients who relapsed after interferon monotherapy or standard interferon and ribavirin therapy. However, most patients relapse again when they are re-treated with the same regimen that was used originally. Extending the duration of re-treatment without changing the dose or regimen may reduce the relapse rate, but this has not yet been proven prospectively. Failure to respond to optimal therapy with pegylated interferon and ribavirin presents a significant problem, particularly in the presence of advanced fibrosis or cirrhosis. Currently, several large-scale, multicenter U.S. trials are evaluating the role of maintenance therapy with pegylated interferon alone in preventing further progression of cirrhosis, clinical decompensation, or development of HCC. Until the results of these studies are available, the role of long-term, continuous therapy with pegylated interferon (or ribavirin or both) for nonresponders should be considered experimental. Knowledge of the severity of the underlying liver disease is important in recommending re-treatment. Patients with advanced fibrosis or cirrhosis have an increased risk of hepatic decompensation and should be considered for re-treatment, especially if they were originally treated with interferon monotherapy. For the re-treatment of patients with intermediate degrees of fibrosis (bridging fibrosis or cirrhosis with minimal disease activity), clinicians should consider the factors enumerated above in determining whether or not to re-treat. Adherence Patient adherence is critical to the success of treatment of hepatitis C. Physicians should discuss the importance of adherence with patients before embarking on therapy and regularly assess and take steps to help their patients maximize their adherence. Such measures include management of side effects, depression, and substance abuse. Side Effects of Treatment In registration trials of pegylated interferon and ribavirin, significant side effects resulted in discontinuation of treatment in approximately 10 to 14 percent of patients. Major side effects of combination therapy include influenza-like symptoms, hematologic abnormalities, and neuropsychiatric symptoms. The education of patients, their family members, and caregivers about side effects and their prospective management is an integral aspect of treatment. Frequent monitoring of neuropsychiatric side effects, cytopenia, and adherence to HCV therapy is necessary. Psychological conditions, particularly depression, are common among persons with hepatitis C and are frequent side effects of interferon. Patients' mental health should be assessed before beginning antiviral therapy and monitored regularly during therapy. Antidepressants, such as selective serotonin re-uptake inhibitors, may be useful in the management of depression associated with antiviral therapy. In selected patients who develop persistent cytopenias despite dose reductions, treatment with hematopoietic growth factors may be useful to reduce symptoms and maintain adherence to antiviral therapy. However, this therapy is costly and the optimal dosage is not yet clear. Further, it is not known if the use of hematopoietic growth factors will enhance the likelihood of SVR. Thus, the benefits of such treatment need to be proven prospectively before it can be recommended. Severe hemolysis from ribavirin may occur in patients with renal insufficiency, and trials of pegylated monotherapy may be indicated in these patients. Lactic acidosis may be a rare complication of combination therapy in patients undergoing therapy for HIV and HCV. 4. Which patients with hepatitis C should be treated?All patients with chronic hepatitis C are potential candidates for antiviral therapy. Treatment is recommended for patients with an increased risk of developing cirrhosis. These patients are characterized by detectable HCV RNA levels higher than 50 IU/mL, a liver biopsy with portal or bridging fibrosis, and at least moderate inflammation and necrosis. The majority also have persistently elevated ALT values. In some patient populations, the risks and benefits of therapy are less clear and should be determined on an individual basis or in the context of clinical trials. Many patients with chronic hepatitis C have been ineligible for trials because of injection drug use, significant alcohol use, age, and a number of comorbid medical and neuropsychiatric conditions. Efforts should be made to increase the availability of the best current treatments to these patients. Because a large number of HCV-infected persons in the United States are incarcerated, programs should be implemented to prevent, diagnose, and treat HCV infection in these individuals. Based on the NHANES III data that demonstrate high prevalence of HCV in African American and Hispanic populations, individuals who are uninsured or have publicly funded healthcare are more likely to be infected with HCV. Efforts should also be initiated to diagnose and treat infection in these individuals. All patients with chronic hepatitis C should be vaccinated against hepatitis A, and seronegative persons with risk factors for hepatitis B virus (HBV) should be vaccinated against hepatitis B. Normal ALT Levels Approximately 30 percent of patients with chronic HCV infection have normal ALT levels, and another 40 percent have ALT levels less than two times the upper limit of normal. Although most of these patients have mild disease, histologically, some may progress to advanced fibrosis and cirrhosis. Experts differ on whether to biopsy and treat these patients. Numerous factors must be considered in recommending treatment, including favorable genotype, presence of hepatic fibrosis, patient motivation, symptoms, severity of comorbid illness, and the patient's age. When patients with normal or minimally elevated ALT levels are treated with monotherapy, their SVR rates are similar to those of patients with higher ALT levels. Studies of pegylated interferon with ribavirin have not been completed in patients with normal ALT levels. Progression to cirrhosis is likely to be slow in patients who have persistent ALT elevations but no fibrosis and minimal necroinflammatory changes. These patients may not need treatment and should be monitored periodically. However, decisions to treat such patients should be individualized and may be based on the patient's desire to eliminate the HCV infection or unwillingness to undergo subsequent liver biopsies to assess disease progression. Advanced Liver Disease Data on safety and efficacy of interferon (standard or pegylated) with or without ribavirin in patients with advanced fibrosis or compensated cirrhosis have largely been derived from subgroup analyses of larger trials. SVR rates are lower in patients with advanced liver disease than in patients without cirrhosis. Further studies are needed to evaluate whether long-term anti-viral therapy will delay histological disease progression to cirrhosis. Liver transplantation offers the primary treatment option for patients with decompensated liver disease. Studies of antiviral therapy are being conducted in patients awaiting liver transplantation, but potentially life-threatening side effects of antivirals have been observed in some patients. Recurrence After Transplantation Hepatitis C frequently recurs following liver transplantation, and disease progression is accelerated compared with immunocompetent patients with HCV disease. Once cirrhosis develops in the allograft, the risk of complications is high. While recurrence of HCV replication is almost universal after liver transplantation, the severity of the recurrence of hepatitis C after transplant correlates with the degree of immunosuppression in the posttransplantation period. Treatment of HCV recurrence after liver transplantation should be considered experimental and carried out in the context of clinical trials. Children should be screened for HCV if they are born to HCV-infected women, received transfusions prior to 1992, or have high-risk behavior. Children and adolescents with chronic HCV infection generally have no symptoms. Little is known about the treatment of children and adolescents, and further research is needed. Studies of interferon monotherapy in children have been largely uncontrolled, with small numbers of highly selected patients. SVR rates are better than in adults, ranging from 33 to 45 percent (26 percent for genotype 1 and 70 percent for other genotypes). Promising new therapies, including the pegylated interferons, should also be studied in children. Some patients may benefit from treatment even if the liver disease is mild. Given the long life expectancy of children and their better tolerance to drugs, the long-term safety of these medications needs to be studied in children. Acute Hepatitis C Acute hepatitis C is uncommonly recognized and diagnosed because most patients do not develop symptoms at the time that the infection is acquired. Studies of interferon treatment for acute hepatitis C have been very heterogeneous and limited by small sample size; lack of randomization; and variability in the timing of therapy after onset of infection, dose, schedule, end points, and followup. High SVR rates (83 to 100 percent) have been reported by small uncontrolled trials with interferon monotherapy. Accordingly, treatment of persons with acute hepatitis C is warranted, but the timing of therapy and the type of regimen to use remains to be determined from future trials. Recent, albeit limited, experience has demonstrated the feasibility and effectiveness of treating chronic hepatitis C in people who use illicit injection drugs, known as injection drug users (IDUs). This is potentially important because injection drug use is the most common risk factor for new HCV infections in the United States, and successful treatment may reduce transmission. Management of HCV-infected IDUs is enhanced by linking these patients to drug-treatment programs. Treatment for drug and alcohol abuse should be made available to all patients who want and need it. Access to methadone treatment programs should be fostered for HCV-infected IDUs whether or not they are receiving treatment for HCV. Methadone treatment has been shown to reduce risky behaviors that can spread HCV infection, and it is not a contraindication to HCV treatment. Efforts should be made to promote collaboration between experts in HCV and healthcare providers specializing in substance-abuse treatment. HCV therapy has been successful even when the patients have not abstained from continued drug or alcohol use or are on daily methadone. However, few data are available on HCV treatment in active IDUs who are not in drug treatment programs. Thus, it is recommended that treatment of active injection drug use be considered on a case-by-case basis, and that active injection drug use in and of itself not be used to exclude such patients from antiviral therapy. HIV Co-infection All HIV-infected persons should be screened for HCV. Patients with chronic hepatitis C and concurrent HIV infection may have an accelerated course of HCV disease. Therefore, although there are no HCV therapies specifically approved for patients co-infected with HIV, these patients should be considered for treatment. Thus far, studies have enrolled only patients with stable HIV infection and well-compensated liver disease. In co-infected persons, an SVR can be achieved with HCV treatment. Preliminary data suggest better responses to pegylated interferon with ribavirin than to standard interferon with ribavirin. Thus treatment of HCV infection in patients with HIV is recommended on a case-by-case basis. Although treatment of HCV does not appear to compromise treatment of the HIV infection, additional data are needed. Monitoring for potential adverse effects from these treatments, including lactic acidosis, is strongly recommended. Alcohol is an important cofactor in the progression of HCV liver disease to cirrhosis and HCC. A history of alcohol abuse is not a contraindication to therapy; however, continued alcohol use during therapy adversely affects response to treatment, and alcohol abstinence is strongly recommended before and during antiviral therapy. Efforts to diagnose and treat alcohol abuse or dependence should be performed in conjunction with treatment of HCV. Heavy alcohol consumption of >80 g/day seriously compromises HCV treatment. Furthermore, safe levels of alcohol consumption are still unclear, and even moderate levels of consumption may accelerate disease progression in some patients. 5. What recommendations can be made to patients to prevent transmission of hepatitis C?The large reservoir of individuals infected with HCV provides a source of transmission to others at risk. Direct percutaneous exposure is the most efficient method for transmitting HCV, and injection drug use accounts for more than two-thirds of all new infections in the United States. Methadone treatment programs, needle and syringe exchange programs, and comprehensive risk-modifying educational programs have been shown to be effective in preventing HIV transmission and are likely to be useful for decreasing HCV transmission. Ensuring access to sterile syringes through physician prescription and pharmacy sales of syringes to IDUs can also be helpful. IDUs should be educated about the importance of hand washing before and after giving injections, not using the others' injection equipment, and avoiding any contact with blood from other persons. HCV prevention education should be a high priority in correctional settings. The majority of cases not attributed to injection drug use can be attributed to sexual contact and occupational exposures to blood, although the actual risk of transmission through these routes is low. Data regarding transmissibility by sexual contact have been confounded in part by other exposures, including injection drug use, that can increase the risk of transmission of HCV. HCV genotypes appear to have no impact on the risk of transmission. HCV is rarely transmitted by transfusion of blood products or transplantation of organs or tissues in the United States and other countries where screening tests exclude infectious donors. In the United States, the estimated seroprevalence of HCV is 2 to 3 percent among partners of HCV-infected persons who are in long-term monogamous relationships and is 4 to 6 percent among persons with multiple sex partners, sex workers, and men who have sex with men (those at risk for sexually transmitted diseases). One study found the risk of HCV infection to be threefold higher for female than male sexual partners. Thus, sexual partners of male and female patients with hepatitis C should be tested for this infection. For heterosexual, discordant monogamous couples, the risk of transmission is estimated to be only 0 to 0.6 percent annually. Because of the low risk of HCV transmission, monogamous couples do not need to use barrier protection (condoms) although they should be advised that condoms may reduce the risk of transmission. However, HCV-infected individuals with multiple sexual partners or in short-term relationships should be advised to use condoms to prevent transmission of HCV and other sexually transmitted diseases. Sharing common household items that may be contaminated with blood, such as razors and toothbrushes, is another potential source of transmission of HCV that should be avoided. There is no evidence that kissing, hugging, sneezing, coughing, food, water, sharing eating utensils or drinking glasses, casual contact, or other contact without exposure to blood is associated with HCV transmission. Healthcare workers have a similar or slightly lower prevalence of HCV infection than the general population, although they may have acquired their infection from occupational sources. Transmission from healthcare workers to patients has also been documented, but is rare and confounded by other risk factors. HCV-infected healthcare workers should use standard (universal) precautions to prevent transmission and should not be restricted in their employment. The risk of HCV infection from a needlestick injury is estimated to be 2 percent. At this time, immune globulin or antiviral prophylaxis is not recommended following needlestick exposure. It is recommended that the source and exposed individual should be tested for antibody to HCV. If the source individual is HCV EIA positive, an immunoblot or HCV RNA assay should be done in the exposed individual. Since HCV RNA is first detected in the blood 2 weeks after transmission, the exposed individual should be tested for HCV antibody, HCV RNA, and ALT at exposure and again between 2 and 8 weeks after injury. If seroconversion occurs, such persons should be referred to a specialist knowledgeable in this area for consideration of treatment. Body piercing and tattooing are other potential sources of transmission if contaminated equipment or supplies are used. However, transmission through these activities is rare and confounded by other risk factors. The risk of perinatal transmission is approximately 2 percent for infants of anti-HCV seropositive women. When a pregnant woman is HCV RNA positive at delivery, this risk increases to 4 to 7 percent. Higher HCV RNA levels appear to be associated with a greater risk. HCV transmission increases up to 20 percent in women co-infected with HCV and HIV. There are no prospective studies evaluating the use of elective cesarean section for the prevention of mother-to-infant transmission of HCV. However, avoiding fetal scalp monitoring and prolonged labor after rupture of membranes may reduce the risk of transmission to the infant. There are currently no data to determine whether antiviral therapy reduces perinatal transmission. Ribavirin and interferons are contraindicated during pregnancy. Breast-feeding does not appear to transmit HCV. Infants born to HCV-positive mothers should be tested for HCV infection by HCV RNA tests on two occasions between the ages of 2 and 6 months and/or have tests for anti-HCV after 15 months of age. Positive anti-HCV in infants prior to 15 months of age may be due to transplacental transfer of maternal anti-HCV antibody. Children and personnel should not be excluded from day care centers, schools, or sports on the basis of HCV infection. Standard (universal) precautions should be used in any situation where exposure to blood occurs. 6. What are the most important areas for future research?
ConclusionsThe incidence of newly acquired hepatitis C infection has diminished in the United States. This decline is largely due to a decrease in cases among IDUs for reasons that are unclear and, to a lesser extent, to testing of blood donors for HCV. The virus is transmitted by blood and such transmission now occurs primarily through injection drug use, sex with an infected partner or multiple partners, and occupational exposure. The majority of infections become chronic, and therefore the prevalence of HCV infections is high, with about 3 million Americans now estimated to be chronically infected. HCV is a leading cause of cirrhosis, a common cause of HCC and the leading cause of liver transplantation in the United States. The disease spectrum associated with HCV infection varies greatly. Various studies have suggested that 3 to 20 percent of chronically infected patients will develop cirrhosis over a 20-year period, and these patients are at risk for HCC. Persons who are older at the time of infection, patients with continuous exposure to alcohol, and those co-infected with HIV or HBV demonstrate accelerated progression to more advanced liver disease. Conversely, individuals infected at a younger age have little or no disease progression over several decades. The diagnosis of chronic hepatitis C infection is often suggested by abnormalities in ALT levels and is established by EIA followed by confirmatory determination of HCV RNA. Several sensitive and specific assays are now partly automated for the purposes of detecting HCV RNA and quantifying the viral level. Although there is little correlation between viral level and disease manifestations, these assays have proven useful in identifying those patients who are more likely to benefit from treatment and, particularly, in demonstrating successful response to treatment as defined by an SVR. Liver biopsy is useful in defining baseline abnormalities of liver disease and in enabling patients and healthcare providers to reach a decision regarding antiviral therapy. Noninvasive tests do not currently provide the information that can be obtained through liver biopsy. Information on the genotype of the virus is important to guide treatment decisions. Genotype 1, most commonly found in the United States, is less amenable to treatment than genotypes 2 or 3. Therefore, clinical trials of antiviral therapies require genotyping information for appropriate stratification of subjects. Recent therapeutic trials in defined, selected populations have clearly shown that combinations of interferons and ribavirin are more effective than monotherapy. Moreover, trials using pegylated interferons have yielded improved SVR rates with similar toxicity profiles. However, results continue to show that the SVR rate is less common in patients with genotype 1 infections, higher HCV RNA levels, or more advanced stages of fibrosis. Genotype 1 infections require therapy for 48 weeks, whereas shorter treatment is feasible in genotype 2 and 3 infections. In genotype 1, the lack of an early virologic response (< 2 log decrease in HCV RNA) is associated with failure to achieve an SVR. The SVR is lower in patients with advanced liver disease than in patients without cirrhosis. Ongoing trials are exploring the usefulness of combination therapy in various populations. Preliminary experience in IDUs, individuals co-infected with HIV, children, and other special groups suggests similar responses are achievable in these populations. Patients with acute hepatitis C may be treated, but specific recommendations for antiviral treatment must await further evaluation of the rate of spontaneous clearance of the virus and determination of the optimal time to initiate treatment. Preventive measures beyond blood-banking practices include prompt identification of infected individuals, awareness of the potential for perinatal transmission, implementation of safe-injection practices, linkage of drug users to drug treatment programs, and implementation of community-based education and support programs to modify risk behavior. Some of these measures have been successfully implemented in the control of HIV infections, and it stands to reason that they would be valuable for reducing HCV transmission. Future advances in the diagnosis and management of hepatitis C require continued vigilance concerning the transmission of this infection, extending treatment to populations not previously evaluated in treatment trials, and the introduction of more effective therapies. RECOMMENDATIONS
Consensus Development Panel
Speakers
Planning Committee
Conference Sponsors National Institute of Diabetes and Digestive and Kidney Diseases Office of Medical Applications of Research Conference Cosponsors National Institute of Child Health and Human Development National Cancer Institute National Center for Complementary and Alternative Medicine National Institute on Alcohol Abuse and Alcoholism National Institute on Drug Abuse National Institute of Allergy and Infectious Diseases National Heart, Lung, and Blood Institute Centers for Medicare & Medicaid Services Centers for Disease Control and Prevention U.S. Food and Drug Administration U.S. Department of Veterans Affairs |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Contact
Consensus Program | Privacy Notice | Disclaimer | Accessibility | Contact NIH |