U.S. Department of Health and Human Services President’s Management Agenda ReportFiscal Year 2005TO HHS EMPLOYEES: The Department of Health and Human Services has accomplished a great deal over the past year thanks to your efforts and focus on results. It is important that we take time to look back on all we have accomplished together and celebrate even as we look forward to future achievements. OVERVIEW The Department of Health and Human Services (HHS) is the United States government's principal agency for protecting the health of all Americans and providing essential human services, especially for those who are least able to help themselves. The Department manages more than 300 programs, covering a wide spectrum of activities. Our many accomplishments were realized in part due to improved effectiveness of management practices being implemented across the Department with the help of the President’s Management Agenda. THE PRESIDENT’S MANAGEMENT AGENDA The President's Management Agenda (PMA) is a bold strategy for improving the management and performance of the federal government. The PMA contains five government-wide goals to improve federal management and deliver results that matter to the American people: - Strategic Management of Human Capital
- Competitive Sourcing
- Improved Financial Performance
- Expanded Electronic Government
- Budget and Performance Integration
The PMA was designed to "address the most apparent deficiencies where the opportunity to improve performance is the greatest." It focuses on remedies to problems generally agreed to be serious, and commits to implementing them fully. In addition to the five government-wide management initiatives, the PMA also focuses on nine agency-specific reforms, of which HHS has four of the Program Initiatives: - Faith-Based and Community Initiative
- Broadening Health Insurance Coverage and Improving Health Services Delivery Through State Initiatives
- Eliminating Improper Payments
- Federal Real Property Asset Management
Lastly, HHS works with other agencies involved in research and development on the PMA initiative: Research and Development (R&D) Investment Criteria. In keeping with the PMA, HHS has achieved management performance results in FY 2005 that are important to HHS’ mission and to the American taxpayer. HHS has done well in institutionalizing our focus on results and citizen-centric government, and we have achieved a “green” progress rating in all but three areas of the PMA. We have also moved to “green” for status in the areas of Competitive Sourcing and Strategic Management of Human Capital and “yellow” for Budget and Performance Integration, Broadening Health Insurance Coverage Through State Initiatives, Expanded Electronic Government, and Faith-Based and Community Initiatives. STRATEGIC MANAGEMENT OF HUMAN CAPITAL HHS has implemented strategies to ensure our ability to recruit and retain appropriately skilled employees. We were one of the first federal agencies to achieve and maintain “green” status in this area on the President’s Management Agenda scorecard. We were also one of the first agencies to receive approval and provisional certification of our new Senior Executive Service (SES) performance-based appraisal system. A centerpiece of our new SES performance system is the linkage between organizational achievement and individual accomplishments of our SES members. Recently, the OPM cited our approach as a government “best-practice” and our SES performance management system has been re-certified for calendar year 2005. Our operating and staff divisions have developed succession workforce plans and identified human capital needs as well as any gaps between current employment and future needs in mission critical positions. These plans provide a map for assessing future human capital needs and are tied to the strategic mission and direction of the Department. We continue to use and expand the use of flexible employment authorities. One example is our highly successful Emerging Leaders Program, currently entering its fourth year, which brings the best and brightest recent graduates to work for HHS. To date, HHS has graduated two classes of Emerging Leaders and placed 115 in permanent positions. The current class has 86 participants and a new class of 60 begins July 25, 2005. The program has a retention rate of approximately 95%. Another is our SES Candidate Development Program, tailored to meet the leadership development needs of each participant. We have placed nearly 40% of the first graduating class of 26 into SES positions. We are currently recruiting the third class of SES candidates. Both of these programs provide a needed resource option to fill behind an ever-growing number of employees who retire or seek other interests outside of HHS. We continue to reshape the workforce using flexibilities such as Voluntary Separation Incentive Payments and Voluntary Early Retirement Authority as authorized by OPM and OMB. These flexibilities are great tools as they provide options for employees and assist management when new programs and initiatives are implemented. The future of HHS’ human capital program is bright, and we continue to be a leader in the Federal workplace. We are the first federal agency to implement a fully electronic Official Personnel Folder (eOPF) integrated with our enterprise human resources system to allow employees access to their personnel folders anywhere, anyplace and anytime. Also, the Department has implemented the first phase of a Learning Management System that provides employee access to nearly 2000 free courses. These courses are available 24 hours each day, 7 days each week on the HHS Learning Portal. Employees can access the learning portal at http://learning.hhs.gov/. In an effort to make the work of the human resources program more responsive to employee and management needs, HHS has embarked upon the development of a transparent workflow system. This system will allow human resource professionals and managers to know the status of personnel requests, from initiation to completion. It is currently being piloted and has received funding for Department-wide rollout. Deployment of the program and tracking of as many as 12 business processes, to include awards tracking, will begin late in the 4th quarter. This will be one of the first-in-government deployments of an HR workflow system. The “draft" of the new performance management system for managers and non-union employees has been distributed for comment. The guide outlines the policies and procedures for planning, monitoring, developing, appraising, and recognizing performance of all HHS non-SES managers, supervisors, and non-bargaining unit employees. This new system will help take the guesswork out of establishing performance expectations, holding progress discussions and appraising employees at the end of the rating period. As the Department moves toward implementation of its new system, managers and employees will receive training on the new performance system. It is anticipated that the new system will be implemented in FY 2006. HHS is also formally documenting its mission-critical and support competencies across the department. A Department-wide work group is documenting competencies for mission critical occupations and developing core competencies that all HHS employees will be expected to possess. The competencies will be placed in the HHS Learning Portal and the Learning Management System and a department-wide gap analysis will be performed. Following the gap analysis, appropriate training opportunities or other interventions will be identified for each employee to close any potential skills gaps in mission critical, support and leadership occupations. The competency-based approach will help employees know what training and development opportunities they will need to explore, and how to satisfy required and desired training to best prepare for achieving greater success in their current positions as well as prepare for future growth opportunities. COMPETITIVE SOURCING Thorough planning and use of competition as a routine management practice have resulted in HHS’ continued leadership in the competitive sourcing initiative. To date, HHS has studied more than 3,500 FTEs. Competitive sourcing is expected to free up nearly $300 million over a six-year period, which can be reallocated to core missions of the Department. To date HHS has completed or announced 134 streamlined competitions and 23 standard competitions. These competitions have served as a focal point for HHS to improve the quality and lower the cost of Department-provided commercial activities through consolidation, process reengineering, workforce realignment, and better leveraging of technology. An additional $150 million in estimated competitive sourcing-related savings is expected to be realized as a result of competitions that are currently under way. HHS is working to apply competition in the most strategic manner possible, such as by reorganizing in-house operations, grouping related activities to form business units that would be more competitive with the commercial market place, and aligning competitive sourcing and human capital efforts to close competency and skill gaps. With ever increasing levels of experience in performing competitive sourcing, the Department expects to achieve even greater savings and efficiencies. The FY 2005 Federal Activities Inventory Reform (FAIR) Act inventory was submitted to OMB in June of this year. In addition to building an HHS FAIR Act dictionary of function code definitions, HHS has implemented a FAIR Act database that maintains Departmental FAIR Act inventory data. The database system is tailored to HHS specifications and allows for greater ease in obtaining necessary and consistent information. The system processes data to assist in the assembly of informative reports and serves to promote consistency in the application of functional codes across the Department through side-by-side comparisons of organizational unit inventories. FAIR Act inventory results are utilized as a basis for determining future studies. IMPROVED FINANCIAL PERFORMANCE In FY 2005, HHS made important performance improvements in its financial management activities. Specifically, HHS: - Improved efficiencies for financial systems by providing a standardized accounting treatment manual currently in use at CDC and FDA, which ensures users have consistent guidance. This enabled CDC and FDA to complete the month-end closing in two days for April and May of 2005.
- Improved system integrity for financial systems by implementing UFMS as the system of record for CDC and FDA as of 6/27/05. As a result, CDC and FDA are United States Standard General Ledger (USSGL) compliant with UFMS, which provides global interfaces and error handling. This uniform approach to problem-solving allowed replication across operating divisions as a centralized governance structure.
- Earned its sixth consecutive unqualified opinion on its FY 2004 financial statement audit.
- Continued to improve the content and presentation of the Department’s Performance and Accountability Report (PAR) to provide important and user-friendly performance and financial information concerning the Department’s program and management goals.
- Performed more frequent financial analyses, thereby strengthening the accuracy of our financial data.
- Continued an operating division-wide analysis to identify the extent to which financial and performance information is currently being used to support routine or 'day-to-day' management decisions. This analysis is intended to ultimately help identify core mission business functions within operating divisions and across the Department and to improve the utility and use of routine financial and performance information to support program and Department management.
- Continued to produce timely interim and annual financial statements and other required reports, enabling managers to make timely decisions.
- Began a phased-in implementation plan for a standardized financial management system (Unified Financial Management System) in all operating components beginning with NIH effective FY 2004, to culminate with IHS and the final phase of CMS contractors in FY 2007. Both CDC and FDA began actively using UFMS as of April 22, 2005, and the PSC implementation is underway with a projected start date of October 2006.
- Began a rollout to Medicare contractors of the Healthcare Integrated General Ledger Accounting System (HIGLAS) – many years in development – a system to extend a standardized financial management component to the handling of Medicare claims transactions.
- Began to leverage economies of scale by replacing five obsolete systems, with Total On-line Processing System (TOPS) and General Ledger Accounting System (GLAS) replaced at CDC and FDA respectively by UFMS, thus reducing administrative costs. The UFMS Business Case projects discounted life-cycle benefits of $423.2 million, versus discounted life-cycle costs of $266.4 million, resulting in an overall return on investment of 58.9 percent.
- Began implementing the recommendations from the FY 2004 Financial Shared Services Study project that specifically explored the benefits of a shared services environment for Department-wide financial asset functions. The first Center of Excellence model is operating the maintenance of the accounting system and the Department began an internal competitive process for an E-Travel Center of Excellence. Operating in a shared services environment will standardize and streamline traditional financial transaction processes and achieve operating efficiencies by leveraging technological investments and standardizing processes across business units. The E-travel Center of Excellence competition will set the framework for additional Centers in Customer Call Center activities and payments.
EXPANDED ELECTRONIC GOVERNMENT (E-GOV) Information Technology (IT) Security Implementing Secure One HHS has propelled the Department’s work toward its goal of continued security for HHS information systems and information that these systems transmit, process, and store. Secure One HHS has established a comprehensive framework that facilitates the development, assessment, and continuous improvement of the HHS IT security program. It incorporates key functional components of security, such as policy, privacy, education and awareness, and certification and accreditation (C&A), spanning the entire spectrum of security from prevention to intervention to follow-up activities. HHS is implementing a network and security-monitoring tool that ensures consistent and continuous security of the HHS technical environment. HHS will implement the Securify product across the entire Department, which will allow consistent security monitoring and reporting capability HHS-wide. HHS now has continuous 24/7 visibility into the HHS network security posture. Secure One HHS is currently working to attain a 100 percent C&A completion; to date 99 percent of systems have been certified and accredited. HHS system security analysis continues to improve, with 100 percent of systems having been assessed for risk. In addition, Secure One HHS continues to build upon foundational processes pertaining to Plan of Action & Milestones (POA&M) activities. Secure One HHS has developed and distributed the HHS Plan of Action & Milestones Guide throughout the Department. Secure One HHS has worked closely with the operating divisions and the OIG to identify information security weaknesses. Furthermore, to date 56 percent of employees have been trained in FY 2005; HHS’ goal is to ensure 100 percent of HHS employees participate in security awareness training. Enterprise Architecture HHS has made great strides in a formalized process to establish and implement an HHS-wide enterprise architecture (EA), which aligns with and supports the Federal Enterprise Architecture. A new website has been developed for the HHS EA program for posting updated EA information http://intranet.hhs.gov/ea/. The enterprise architecture repository and analysis and reporting tool has been implemented and is in the process of being populated with previously collected data. This tool also provides an enhanced ability to publish enterprise architecture information in a variety of ways. As the use of this tool is refined, enterprise architectural information that is targeted for specific audiences can be made available. Using these evolving EA capabilities, HHS has achieved EA Program maturity at Level 3, as measured by the FEA Assessment Tool. HHS.gov The HHS.gov Web site continues to demonstrate increased service to the public. Site statistics show approximately 2.5 million visits per quarter to the HHS.gov Web pages. Site visits increased more than 30 percent over the same period in 2004. The frequently asked questions (FAQ) database now has 450 answers available for viewing by an average 125,000 people each month. Approximately 36 percent fewer unique questions per month are being submitted to the Department as a result of the availability of new answers. The statistics demonstrate that the HHS.gov Web site effectively serves an increasing number of visitors by providing information on the Web site and in the FAQ database. Perhaps the most significant business impact continues to be in the area of Health Insurance Portability and Accountability Act (HIPAA) privacy rule information dissemination. Since April 2003, OCR had more than 3 million Privacy Rule answers viewed on the FAQ site maintained by HHS. These materials have consistently been the most requested of all HHS.gov subject matter resources. HHS continues to improve upon the site, include continued Web site analyses, and integrate usability principles and evidence-based design. In March 2005, a new enterprise-wide Web search debuted which brings greater flexibility to search services and improves user results. It has also allowed us to begin consolidating search services that were supported by multiple tools. The new HHS Web Management Program is managing the Department’s Web presence and serving as a Department-wide resource for delivering effective and usable Web communications to the American public. Grants.gov HHS serves as the Managing Partner for this cross-government initiative. The goal of Grants.gov is to make the grant location, application, and submission process faster, easier, and more efficient. Grants.gov has been working closely with grant-making agencies to meet their grant application package posting goals. As of June 2005, 21 of the 26 grant-making agencies have collectively posted 1025 application packages and received over 8,500 electronic application submissions from the grant community via Grants.gov’s Apply mechanism. Over 10,000 organizations have registered with Grants.gov, allowing them to apply for Federal grants via Grants.gov. In addition, all agencies are posting their funding opportunities on Grants.gov’s Find mechanism. The Grants.gov site receives over 340,000 hits per day and sends over one million emails per week at the request of the grant community. Grants.gov has been working with the grant community to test applicant system-to-system functionality, and has completed system-to-system tests with 15 grant-making agencies. Grants.gov continues its outreach and marketing activities, to include monthly meetings with the Grants Executive Board, stakeholders, and OMB. Recently, Grants.gov conducted its first live Webcast titled "Spread the Word” which was attended by more than 2,500 grant community organizations. Health Information Technology The HHS Office of the National Coordinator for Health Information Technology (ONCHIT) has been working toward the President's goal to adopt electronic heath records (EHRs) for most Americans within 10 years. In 2004 we published, "Framework for Strategic Action: The Decade of Health Information Technology," in which we outlined an approach toward nationwide implementation of interoperability. Since then, significant progress has been made. Within the Federal government, ONCHIT has consulted with and actively partnered with numerous federal agencies (e.g., OPM, VA, DoD, DHS, Treasury, and Commerce) and established a consortium of federal agencies called the ONC Advisory Committee (consisting of HHS, DoD, VA, OPM, and DHS) to provide strategic direction on coordination of health IT across the federal enterprise. ONCHIT now has responsibility for the Federal Health Architecture (FHA), as well as the Consolidated Health Informatics (CHI), which has recommended 20 standards for health information exchange to be used by the federal government. ONCHIT has been focusing on subsequent efforts to enhance the usability of these standards as well as supporting the adoption of additional standards. To lay the business foundation for health IT, HHS formed a Health Information Technology Leadership Panel of nine CEOs from Fortune 100 companies to assess the costs and benefits of health IT and to evaluate the urgency of investments in these tools. Among its findings, the panel stated that the widespread adoption of health IT should be a top priority for the U.S. health care system and that the federal government should use its leverage as a healthcare purchaser and payer to drive health IT adoption. These findings were published in a report in May 2005. To lay the technical foundation for health IT, HHS issued a Request for Information (RFI) that solicited public input about whether and how a Nationwide Health Information Network (NHIN) could be developed. These responses have yielded one of the richest and most descriptive collections of thoughts on interoperability and health information exchange that has likely ever been assembled in the U.S. As such, it has set the foundation for actionable steps designed to meet the President's goal. The Secretary initiated Phase One of the HHS health IT strategy in June 2005. In Phase One, we will form the American Health Information Community (AHIC), a federal advisory committee that will develop recommendations for coordinating efforts in the public and private sectors for interoperable health IT adoption. In coordination with the AHIC, Phase One of the Secretary's health IT strategy will include evaluating and implementing the following critical actions: harmonizing health information standards; certifying health IT products to assure consistency with standards; addressing privacy and security policies; and developing an architecture for nationwide sharing of electronic health information. Citizen Centric Service The CDC has established an operational contact center for major health topic areas, including influenza vaccine, HIV/AIDS, STDs, immunizations, and hot topics in the media. CDC is consolidating all public and medical professional inquiry hotlines to establish a single, integrated, customer-centric service center. This includes inquiries received by phone, fax, letter, e-mail, or web. The Medicare Beneficiary Portal (MBP), part of the Indiana Pilot for CMS’ Virtual Call Center Strategy, is leveraging the Next Generation Desktop application infrastructure to provide beneficiaries with a set of secure, self-service transactions, including the ability to view Medicare claim information via the web. The MBP went live in Indiana in December 2004. Plans are currently underway to provide a broader set of functionality to a national population of Medicare beneficiaries in the near future. MBP marks a significant step and another turning point in the history of Medicare.gov to better serve Medicare beneficiaries and provide secure transactions and relevant information through the Internet. One of the President’s Management Agenda electronic government initiatives is USA Services, managed by the General Services Administration (GSA). HHS and GSA have established, as a service provided by USA Services, an automated method to handle e-mail messages from the public that do not pertain to HHS. HHS has established an e-mail address and identified contact phone numbers for HHS employees to route erroneously received incoming communications; this information has been made available on our internal eGov Web site at: http://intranet.hhs.gov/egov/. HHS employees are now able to forward misdirected email for an appropriate timely response. In addition, HHS maintains and disseminates, via the HHS.gov web site, a directory of information sources and contacts, as well as an extensive Frequently Asked Questions database. IT Consolidation The HHS Network Modernization (HHSNet) implementation team continues to manage the implementation of HHSNet in three phases to reduce risk and to ensure a seamless migration to the unified HHS network. Phase I encompassed internal/Intranet wide area network access within each operating division. Phase II achieved these same objectives between all operating divisions. Phase III will consolidate external/Internet access across the Department. HHSNet is now in Phase III, which will result in a reduced number of independent Internet gateways across the Department from 31 to 11. FDA began an effort to update the FY 2004 FDA IT Consolidation Plan in order to reflect FDA’s key priorities in FY 2005. In the original plan, three areas of focus were identified: organization, infrastructure services and processes. Efforts in FY 2004 focused primarily on organizational consolidation, specifically the standing up of the IT Shared Services organization and the transition of all formal IT organizations to direct reports to the CIO. For FY 2005, the CIO will concentrate more on the areas of infrastructure services and processes, with the White Oak Data Center Consolidation initiative as the overarching objective, in order to keep supporting efforts in line with the overall schedule and budget. NIH established a Central Network Management System and Network Operations Center to implement performance management and to monitor NIH Institutes/Centers local area networks. This accomplishment provides proactive monitoring and problem notification across the NIH network, resulting in improved network reliability and reduced repair time. NIH also completed consolidation of directories operated by 18 NIH Institutes/Centers into a single NIH domain. This consolidation improves the reliability and robustness of directory services and of NIH's single sign-on system, which lets authorized users access multiple enterprise systems by logging on only once. Furthermore, it protects against loss of directory services resulting from server or local network failure. The improved reliability and robustness of NIH systems optimizes NIH's ability to provide information to the public through NIH Web sites and through email communications. BUDGET AND PERFORMANCE INTEGRATION In FY 2005, HHS continued to successfully integrate performance information into budget and management decision processes at the Department, operating division, and program level. The purpose of budget and performance information is to improve program performance and efficiency. The following are examples of improved program performance across the Department: Program Accomplishments - 65 Percent of Head Start teachers held an AA, BA, Advanced Degree, or a degree in a field related to early childhood education in FY 2004. (ACF)
- 69 Percent of American Indian/Alaska Native patients over 65 have received a pneumovax immunization as of FY 2004. (IHS)
- 91 Percent of original generic drug applications were reviewed and acted on by the Center for Drug Evaluation and Research within six months of submission. (FDA)
- 91 Percent of children receiving services under the Comprehensive Community Mental Health Services for Children and Their Families program attended school 75 percent or more of the time in FY 2004. (SAMHSA)
- 24,928 homes of American Indian/Alaska Native patients received appropriate sanitation during FY 2004. (IHS)
- 70,926 field examinations of imported food by the Center for Food Safety and Applied Nutrition and Office of Regulatory Affairs in FY 2004 (a 6-fold increase from 12,000 field import examinations conducted in FY 2001). (FDA)
- 86,000 individuals received essential HIV/AIDS medications at least one month of the year during FY 2003 through the AIDS Drug Assistance Program. (HRSA)
- 293,500 severely disabled elders received home-delivered meals in FY 2004, allowing them to remain in their homes in the community. (AoA)
- 5,800,000 children enrolled in the State Children's Health Insurance Program in FY 2003. (CMS)
- 7,800,000 single nucleotide polymorphisms (SNPs) discovered by 2004 – 4.8 million more than originally planned. (NIH)
- 12,400,000 people accessed primary and preventive health care through the Health Centers program in FY 2003 – a 20 percent increase since FY 2001. (HRSA)
- 30,000,000 number of Americans who can be given prophylaxis to prevent illness from anthrax exposure through antibiotics the Strategic National Stockpile had purchased by the end of FY 2004. (CDC)
- 42,000,000 individuals covered by Medicare in FY 2004. (CMS)
- 42,900,000 poor and disabled individuals provided medical assistance by Medicaid in FY 2004. (CMS)
FY 2006 Integrated Performance Budget In February 2005, HHS submitted to Congress the Department's first integrated performance budgets. The FY 2006 performance budget combines budget and performance information in a single volume. It includes a number of changes from the traditional budget structure, such as a new performance budget overview section and supporting performance information that addresses the requirements of the Government Performance and Results Act (GPRA). Additionally, in each program narrative, there is both a rationale for the budget request and a performance analysis. The FY 2006 performance budgets for HHS Operating Divisions are located on the Office of Budget website at: http://www.hhs.gov/budget/opdivs.html. HHS will build on the success of the FY 2006 performance budgets during the FY 2007 budget process. PART Assessment HHS has participated actively in the OMB PART process, completing a total of over 60 PART assessments for the FY 2004-FY 2006 budget process. More than 40 programs received a rating of Adequate, Moderately Effective, or Effective. HHS uses PART information to improve program performance and efficiency and to inform program management and budget decisions. HHS’ use of PART is highlighted below. - FDA established a senior level Strategic Planning Council that utilizes performance and budget information including PART results to inform management and budget decisions.
- HRSA’s Rural Health and Children’s Hospital GME programs proposed budget reductions in FY 2006 in response to the PART finding them duplicative of other programs.
- IHS uses the PART assessment to improve programs by conducting an independent evaluation of the Sanitation Facilities Construction program.
- In response to PART, SAMHSA implemented web-based data systems to improve data collection and reporting. Additionally, SAMHSA rewrote grantee guidelines to include incentive and disincentive procedures to improve efficiency and cost effectiveness. SAMHSA has also initiated funding for a national evaluation of the Substance Abuse Prevention and Treatment block grant.
- At CDC, the 317 Immunization, Occupational Safety and Health, and Diabetes Prevention and Control programs initiated independent evaluations, a principal objective of PART. In addition, the Domestic HIV/AIDS Prevention program implemented the Performance Evaluation Monitoring System to better collect performance data from grantees.
- AoA is conducting an evaluation of the Preventive Health Services component in response to a PART recommendation.
In addition, HHS uses the PART assessment to identify and improve program deficiencies. Programs that have received a rating of Results Not Demonstrated will develop plans to improve their programs, address their deficiencies, and prepare for a PART reassessment. HHS also uses the PART assessments to improve program efficiency. Many PART-ed programs now have an efficiency measure. Programs that do not have an efficiency measure are developing a plan with a timeline to have a finalized efficiency measure. Senior Manager Meetings In the summer of 2005, HHS will kick off the FY 2007 Departmental budget process. During this period, senior staff will meet to discuss each operating division’s budget requests in the context of the Presidential and Secretarial priorities and overall funding levels. Senior officials will review performance information regarding program effectiveness, including performance on key programs as part of the budget process. FAITH-BASED AND COMMUNITY INITIATIVE The mission of the Faith-Based and Community Initiative (FBCI) at HHS is to create an environment within the Department that welcomes the participation of faith-based and community organizations as valued and essential partners in assisting Americans in need. Through the collaborative efforts of the Center for Faith-Based and Community Initiatives and several Operating Divisions, HHS has achieved a green progress rating for every quarter this fiscal year. HHS has made the following accomplishments in outreach/technical assistance, pilot projects, data collection and regulatory reform. Outreach/Technical Assistance CFBCI continues to reach out to faith-based and community organizations to provide information about grant opportunities at the Department. Earlier this year, CFBCI released the 2005 Grant Opportunities Notebook that provides information about multiple grant opportunities at the Department. In addition to meeting and corresponding with faith-based and community organizations from across the country, HHS has also participated in Regional Conferences on the Faith-Based and Community Initiative and has developed web resources and information to help organizations increase their capacity and improve grant applications. Pilot Projects HHS has continued its commitment to pilot projects this fiscal year through the Compassion Capital Fund and Mentoring Children of Prisoners programs at the Administration for Children and Families and the Access to Recovery Program at the Substance Abuse and Mental Health Services Administration. Through these programs, services are being provided to help thousands of Americans in need and to assist organizations in building their capacity to serve even more people. Program officials continue to provide training and technical assistance to grantees and are working to implement outcome-based, evaluative research for each of these pilot projects. Data Collection HHS contributed to a report released by the White House Office of Faith-Based and Community Initiatives on grant awards made to faith-based organizations in FY 2004. The report found that HHS awarded $681 million through 908 grants to faith-based organizations in FY 2004. This was a 43% increase in the amount of funding awarded to faith-based organizations from 2002 and an 88% increase in the number of grants awarded over the same period. Regulatory Reform The Office of General Counsel has taken steps to train HHS staff on the implementation of the Equal Treatment and Charitable Choice Regulations that were published in previous fiscal years. HHS is also working with other Federal agencies to develop guidance for State and local administrators of Federal funds on the implementation of these regulations, in order to continue to level the playing field for grassroots organizations at all levels of government. BROADENING HEALTH INSURANCE COVERAGE and IMPROVING HEALTH SERVICES DELIVERY THROUGH STATE INITIATIVES The Medicaid program provides healthcare to millions of low-income Americans who otherwise would lack health insurance coverage. However, many Americans still lack either private or public insurance coverage. Through a variety of initiatives, and in partnership with the Nation’s Governors, the Administration has made significant strides in addressing access to coverage for uninsured low-income Americans, and in improving the health care coverage that Medicaid beneficiaries receive. The Health Insurance Flexibility & Accountability Initiative-Eligibility for New Health Care Coverage Affects Hundreds of Thousands In 2002, CMS first announced the Health Insurance Flexibility and Accountability (HIFA) demonstration initiative, a new approach to demonstrations in Medicaid and the State Children's Health Insurance Program (SCHIP). Since that time, the Administration has encouraged new comprehensive state approaches to increase the number of individuals with health insurance coverage within current-level Medicaid and SCHIP resources. HIFA puts a particular emphasis on broad statewide approaches that maximize private health insurance coverage options and target Medicaid and SCHIP resources to populations with income below 200 percent of the Federal poverty level (FPL). By supporting private coverage options in the states, the Administration has sought to promote new health care coverage without encouraging a “one-size-fits-all” approach. CMS estimates that HIFA demonstrations, 1if fully implemented, could potentially enroll as many as 825,250 new people. Four additional HIFA proposals2 are pending approval that estimate potential enrollment at an additional 78,500. New Condition-Specific Health Care Coverage: Breast and Cervical Cancer CMS has been working to ensure that as many states as possible take advantage of the opportunity for enhanced Federal funding under the Breast and Cervical Cancer Prevention and Treatment Act of 2000 (BCCPTA). The BCCPTA gives states enhanced federal matching funds to provide Medicaid eligibility to a new group of women previously not Medicaid eligible. The new option allows states to provide full Medicaid benefits to uninsured women under age 65 who are identified through the CDC’s National Breast and Cervical Cancer Early Detection Program (NBCCEDP), are in need of treatment for breast or cervical cancer, including pre-cancerous conditions, and are not otherwise eligible for Medicaid. This provision, effective October 1, 2000, also allows states to extend presumptive eligibility to applicants in order to ensure that needed treatment begins as early as possible and that life-saving interventions may be made in a timely fashion. All 50 states and the District of Columbia are now participating in the BCCPTA. Nearly half of the states have also adopted a presumptive eligibility option. At the end of March 2005 states reported having approximately 15,100 women enrolled in Medicaid through the BCCPTA. The enrollment number is a “point in time” enrollment and reflects all the women enrolled nationally at the same time. The number of women enrolled increased from approximately 11,500 in March of 2004 to 15,100 in March of 2005. Women remain eligible for Medicaid under the BCCPTA as long as they require treatment for breast or cervical cancer. Health Care Coverage for Seniors and Individuals with Disabilities-Improved Access, Improved Services Helping Individuals with Disabilities Participate in the Ownership Society through Employment Access to health care coverage is also a crucial factor in allowing Americans with disabilities to realize their fullest employment potential. To ensure that the contributions of disabled individuals in the workforce are not overlooked and that the business community takes full advantage of disabled individuals’ skills and talents, CMS has designed and implemented two groundbreaking employment initiatives mandated by the Ticket to Work and Work Incentives Improvement Act of 1999 (TWWIIA): the Demonstration to Maintain Independence and the Medicaid Infrastructure (MIG) Grants. In FY 2005, CMS awarded $21.8 million in these grants to 42 States and the District of Columbia to help people with disabilities find and keep work without losing their health benefits. With these awards, HHS has given a total of $100 million in Medicaid Infrastructure Grants (MIG) to 47 States and the District of Columbia under this program. On April 29, 2005, CMS released the FY06 solicitation and expects to award 15-25 additional awards totaling approximately $42 million. Thirty-one States have implemented Medicaid Buy-In programs that ensure health coverage for over 76,000 people enrolled in the program who work. Improving the Availability of Services in the Home and Community Since 2001, CMS has awarded a total of approximately $188 million (2001 - 2004) to all States, District of Columbia, and two territories to help develop programs that enable people of all ages with disabilities or long-term illnesses to live meaningful lives in the community. For the current fiscal year, CMS issued the Fiscal Year 2005 solicitation on April 29, 2005 and plans to award up to 20 additional grants totaling approximately $30 million. Since Fiscal year 2001 and through the current fiscal year, CMS has also funded feasibility study grants that laid the groundwork for larger initiatives included in the President’s FY 2006 budget: - Respite for Adults: Approximately $348,000 in total to CA, NY, RI, and OH.
- Respite for Children: Approximately $574,000 in total to AL, AR, MD, MI, OR, and RI.
- Community-Based Treatment Alternatives for Children: Approximately $593,000 total to IL, MD, MA, MS, MO, and TX.
- Rebalancing Long-Term Care Systems: Approximately $2,023,582 in total to IL, LA, ND, NC, MS, VA, and TN.
In collaboration with the Administration on Aging (AoA), CMS has awarded 24 Aging and Disability Resource Center grants (AK, AR, CA, CMNI, FL, GA, IA, IL, IN, LA, ME, MD, MA, MN, MT, NC, NH, NJ, NM, PA, RI, SC, WI, and WV) of up to $800,000 each to help States develop one-stop shopping centers for seniors and people with disabilities who need long-term care information. On April 29, 2005, CMS and AoA jointly issued the FY05 solicitation and plan to award up to 20 additional grants totaling approximately $15 million. Improving the Quality of Services for Disabled and Elderly Individuals CMS' Action Plan for Quality is a multi-pronged strategy to address quality of care issues in home and community-based services (HCBS), with the aim of both assuring and improving quality and also strengthening state and federal oversight of quality. The initiative began in 2002; for 2005, CMS is: - Completing a second draft revision to the 1915(c) HCBS waiver application incorporating design requirements for self-direction (a constituent element for any quality strategy) and expectations for quality management. The application incorporated input from relevant stakeholder associations and was distributed to them March 7, 2005 for further comment. The modernized and enhanced waiver application is being converted to an electronic, web-based format; completion of the web-based application is expected in Fall 2005.
- Contracting with national organizations with the necessary expertise to provide on-site technical assistance to more than half of the states; the assistance will help them redesign their quality management systems and remedy identified problems.
- Continuing our publication of a series of Quality Communications, which disseminate tools to assist states in managing and improving quality in waiver programs. Our most recent technical assistance paper was Risk Management and Quality in HCBS (Feb. 2005). This Quality Communication builds upon previous technical assistance documents/surveys circulated to improve quality, including the Quality Framework (Aug. 2002); HCBS Quality Workbook (Oct. 2003); National Quality Inventory Survey (Feb. 2004); and The Participant Experience Survey, for aged, disabled, and for mental retardation/developmentally disabled populations and users guides (May 2004).
- Continuing to implement a revamped CMS protocol for reviewing each state’s management of waiver programs and each state's adherence to the waiver assurances. The new protocol is based on a review of evidence generated from each state’s oversight systems. CMS makes a determination about the adequacy of the evidence and each state’s system of oversight and provides its findings, conclusions and recommendations to the state through a standard, written report. Where inadequacies are identified, states are advised to incorporate remedies or changes to the program into their waiver renewal application.
ELIMINATING IMPROPER PAYMENTS In FY 2005, HHS made significant progress in its activities to identify, reduce and recover improper payments in seven of its largest programs. These programs make up 89 percent of HHS total FY04 expenditures ($543 billion). Specifically, HHS: - Reported improper payment error rates for the Medicare Program. In addition, we made significant progress toward reducing the FY 04 Medicare error rate of 10.1% ($21.7 billion) to the FY 05 target rate of 7.9%.
- Reported an improper payments error rate of 3.9% for the Head Start Program. In addition, worked aggressively toward reducing that rate to 3.5%.
- Improved on the risk assessment model and completed all HHS program risk assessments for FY05.
- For the first time determined a payment error rate in the Foster Care Program. Worked toward identifying and implementing appropriate action to reduce the 10.33% ($186M) payment error rate.
- Completed recovery auditing of PSC FY02 and FY03 contract payment transactions (identifying a very insignificant amount of improper payments). Also, completed 50 percent to 75 percent of recovery auditing work at four other contract payment offices.
- Developed and initiated pilots in the TANF and Child Care Programs to assist with identification of methodologies for estimating improper payments in those programs.
FEDERAL REAL PROPERTY ASSET MANAGEMENT Real Property Asset Management was added to the General Accounting Office’s High Risk Series in January 2003, due to “Long-standing problems with excess and underutilized real property, deteriorating facilities, unreliable real property data, and costly space challenges…” The President issued Executive Order (EO) 13327, “Real Property Asset Management” in February 2004, and Real Property was added to the President’s Management Agenda scorecard in the third quarter of 2004. The PMA requires Departments and Agencies to take numerous steps to improve real property asset management, and to follow the lead of the new Federal Real Property Council (FRPC), established by the EO and chaired by the OMB Deputy Director for Management. Similar to other PMA elements, several of the Real Property goals are difficult to achieve and will take time. Goals include development of an HHS Real Property Asset Management Program (RAMP) linked to agency program goals, an integrated real property inventory used in daily decision-making with 23 mandatory FRPC data elements, use of common FRPC performance measures, and evidence that the plan is being implemented with a 3-year timeline of goals and objectives. The RAMP will encompass all aspects of real property asset management, including: planning, design, and construction; leasing; operations and maintenance; environmental management; historic preservation; energy management; and human resources in the facilities area. The quality and expense of the workplace affects everyone in HHS, and the integrated planning demanded by the EO has many potential benefits. Opportunities for cost avoidance can allow more money to be available for operating divisions to expend on other important needs, such as program, salaries, benefits, and training. As HHS integrates sustainable design concepts, facilities will use less energy and be more environmentally friendly, benefiting everyone. Unneeded facilities will be demolished or sold instead of deteriorating in place and consuming funds that could be better spent on active issues. Development of the RAMP Like other agencies, HHS began with “red” Scorecard status, but HHS has laid out a strategy to get to “green” and has thus far received “green” progress scores every quarter. The HHS RAMP is based on three guiding principles: - Efficient portfolio management
- Fostering mission success through occupant productivity and efficiency, and
- Appropriate stewardship of HHS owned, leased, or otherwise managed properties
The HHS team, working collaboratively, deserves great credit for the significant progress made so far. Teams of HHS facilities personnel representing the operating divisions (OPDIVs) are developing consistent ways to implement FRPC-mandatory metrics: - Facility Condition Index
- Operating Cost
- Facility Utilization
- Facility Mission Dependency
While these measures may not sound complex, they can be. OPDIVs have historically used at least some of them but all are doing it differently, and using different automated real property systems as well. The efforts of the teams have been truly outstanding. Teams are also developing internal HHS facility management metrics; are rewriting the PHS Facilities Program (policy) Manual; and above all are keeping in mind the basic health mission that the facilities infrastructure supports. Ultimately, as these measures are put into use, employees will see better prioritization of facility projects because facilities staffs will have improved information. Maintenance and repair will improve as dollars are better directed to the most urgent problems. New and Renovated Facilities HHS real property asset management is already improving dramatically. New facilities are being completed that will improve the mission capability at CDC, IHS, NIH as well as the quality of workplace for HHS employees. All land-holding operating divisions (CDC, FDA, IHS, NIH) are accomplishing repair and improvement projects on owned buildings. Department-wide Pre-Project Planning (P3) training is complete, and over 200 facilities professionals are now armed with new tools to reduce project risks. P3 implementation is driving better construction requirements development, better early cost estimates and therefore better project outcomes. Acquisition planning is assuring that the right approach is used for construction. The CDC Design-Build acquisition pilot project, Environmental Health Facility, generated over $13M in savings compared to the previously planned acquisition approach. Improved Space Management Consistent space management policies are driving significant cost avoidances while preserving a productive work environment. Our consistent space standard across the Department assures that all employees are assigned space under the same standard and avoids high costs associated with duplicative and excessive space requirements. This enables HHS to better withstand impacts of budget cuts without impacting salaries, which also come from operating accounts. Better space management has generated at least $40M in cost avoidances over the past three years. Facilities Competencies Building systems are more complex every year. Environmental and regulatory requirements are increasing. Professional knowledge requirements are transitioning from the drafting board to the boardroom as inherently governmental technical staff is expected to become ever stronger on personnel, project, and contract management. Largely due to competitive sourcing, workforce demographics are changing as land-holding operating divisions implement most efficient organizations. The Department-wide P3 training is the first of several activities to facilitate workforce transition and competency development to face a challenging future. The Department still has much to do in Real Property Asset Management, and the collaborative approach will result in a much more strategic and integrated Real Property Asset Management function. The Department is on track to reach that goal. RESEARCH AND DEVELOPMENT (R&D) INVESTMENT CRITERIA HHS continues its commitment to ensuring that its investments in R&D are effective and yield new knowledge that is applied to the development of new diagnostics, treatments, and preventive measures to improve health and health-related quality of life. Central to the development and implementation of objectives under the Department’s Strategic Plan Goal 4, “Enhance the capacity and productivity of the Nation’s health science research enterprise” are the PMA R&D Investment Criteria. These criteria—relevance, quality, and performance—are carefully considered as research goals and annual targets are developed, as performance is monitored, and as budget decisions are made by HHS and its operating divisions. Several agencies within HHS are evaluated with respect to these criteria. The first criterion—relevance—is addressed in several ways as it relates to research. One way is in setting research priorities—by considering public health needs, as judged by the incidence, severity, and cost of specific disorders as a key factor in determining areas of research support. Relevance is also ensured through seeking the views of the public through a variety of forums. In addition, relevance is also considered when planning activities that will occur after the research is completed.  For example, NIH conducted outreach programs in 5 U.S. cities and distributed 109,619 Know Stroke brochures through targeted educational programs, including 27,236 brochures to African American audiences. Additionally, 3,000 Know Stroke community education kits were distributed through an ongoing national marketing campaign to city and county health officials. Through all of these efforts, in FY 2005, across the Nation, policymakers, consumers, patients, and providers of care are making better-informed health care decisions and are receiving higher quality care thanks to HHS-supported research. Quality—the second criterion—is embodied by a commitment on the part of HHS operating divisions to support work of the highest scientific caliber. The operating divisions ensure quality through the peer review process for grants. What You Need to Know About Stroke (Brochure) 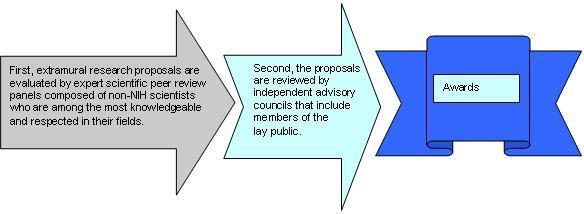 The third criterion—performance—is key to each and every R&D goal set by the Department. Performance is considered in the initial review of grant applications, in funding decisions, and is continually monitored. For example, grantees must submit annual progress reports, and this information is reviewed to assess their performance and follow-up actions taken when necessary. Aside from project-specific reviews, there are state-of-the-science reviews, workshops, and other scientific meetings where knowledge in a particular area of research is reviewed, and progress and performance are assessed. Performance is exemplified through HHS efforts to accelerate research productivity. For example, deliberate exposure of the civilian population of the United States to anthrax in 2001 uncovered a need for tests to rapidly diagnose, prevent, treat, or cure disease caused by agents of bioterrorism. Development of five new animal models, several of which were ahead of schedule, is accelerating research on new diagnostics, vaccines, and therapies for biodefense. 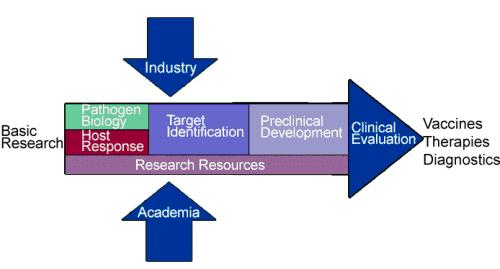  In one of the largest adult vaccine clinical trials ever, researchers have found that an experimental vaccine against shingles (zoster vaccine) prevented about half of the cases of shingles — a painful nerve and skin infection — and dramatically reduced its severity and complications in vaccinated persons who got the disease. Because we cannot predict discoveries or anticipate the opportunities new discoveries will create, HHS supports research across the spectrum of basic, clinical, and applied sciences. CONCLUSION As HHS continues our focus on management results, we look forward to the benefits of a fully integrated department providing 21st century service to our employees and customers, in a more cost-effective and timely manner.
1Eleven States (Arizona, California, Colorado, Idaho, Illinois, Maine, Michigan, New Jersey, New Mexico, Oregon and Virginia) have approved HIFAs. According to the demonstration applications, the combined total of potential enrollees for these eleven states is 825,250. The breakdown by state is: Arizona (48,250), California (275,000), Colorado (13,000), Idaho (1,000), Illinois (300,000), Maine (11,500), Michigan (62,000), New Jersey (12,000), New Mexico (40,000), Oregon (60,000) and Virginia (2,500).
2CMS is currently reviewing four HIFA proposals (Arkansas, Louisiana, Oklahoma and Texas). According to the demonstration applications, the combined potential enrollment for the four proposals is approximately 78,500. The breakdown by state is: Arkansas (55,000), Louisiana (4,000), Oklahoma (10,000) and Texas (9,500).
|