|
|
|||||
|
|
A 40 year old man, resident of the United States, presents to an emergency room with a 5-day history of fever, chills, nausea, vomiting, and myalgias. He returned 2 weeks ago from a 16-day visit to Zambia. Question 1: What chemoprophylaxis regimen (if any) should be recommended for travel to Zambia? (more than one might apply)
For this travel to Zambia, the patient had been prescribed chloroquine. However, he took only a few doses during his visit. On the return flight home, the patient had fever, nausea, and myalgias. Upon arrival to the United States, the symptoms dissipated and the patient did not seek medical care. Nine days later, he had again fever, chills, nausea, vomiting, and myalgias. He went to an outpatient clinic where he was diagnosed with viral syndrome and sent home. Question 2: Based on the observed time intervals, could the symptoms experienced by the patient be due to malaria?
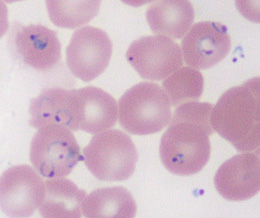
Some days later, the patient was seen at another clinic, where on a routine CBC malaria parasites were seen. He was then referred to a hospital, where he presents to the emergency room, at 4 am, with continuing fever, nausea, vomiting, and myalgias. On physical examination, the patient is febrile (102°F), tachycardic. jaundiced and pale. He is well oriented but slow in answering questions. A thin blood smear obtained while in the emergency room is read as Plasmodium, species not determined. Other laboratory findings include: hematocrit 33% , creatinine 3.6 mg/dL, and total bilirubin 11.0 mg/dL. The urine is dark, with a measured output of 40 mL/6 hours. Question 3: Which one of the following would be the best next step in the clinical management of this case?
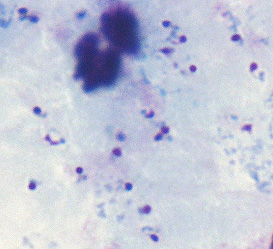
The patient is admitted to the medical intensive care unit and treated with oral quinine and doxycycline. Later that day, the blood smear is reviewed by more experienced personnel for speciation.
Question 4: What is the diagnosis? The smears are diagnosed as P. falciparum, and a parasite quantification shows that 17% of the erythrocytes are infected. The patient's mental status deteriorates and his urine output decreases. Question 5: Which of the following measures would be appropriate?
Treatment with oral antimalarials is continued and an exchange transfusion is ordered. While preparing for the exchange transfusion, the patient becomes hypotensive, requiring a dopamine drip. During the exchange transfusion, the patient becomes increasingly tachypneic and develops atrial flutter, which exacerbates the hypotension. DC cardioversion is attempted without success. The patient develops asystole and expires 17 hours after admission to the medical intensive care unit.
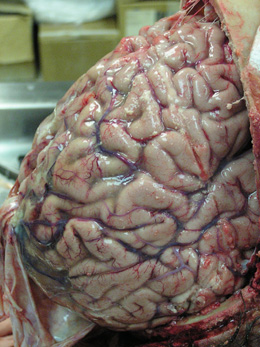
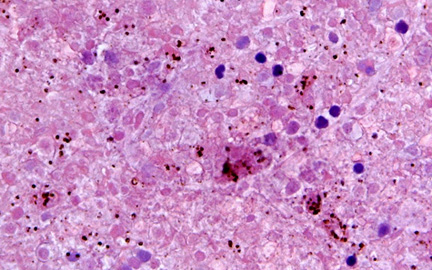
An autopsy was performed, but after a delay of 8 days. The gross findings show a slight swelling of the cerebral gyri, with consequent narrowing of the sulci; some blood vessels are engorged, with scattered petechial hemorrhage. The hematoxylin-eosin section of the brain shows autolysis, some pycnotic nuclei, and scattered pigment felt to be malarial in origin. The pigment and pinpoint hemorrhages are felt to be pre-mortem. Main points:
Page last modified : July 30, 2004 Content source: Division of Parasitic Diseases National Center for Zoonotic, Vector-Borne, and Enteric Diseases (ZVED)
|
|
||||||||||||||||||||||||||
| Home | Policies and Regulations | Disclaimer | e-Government | FOIA | Contact Us | ||||||
|