|
Prostate Changes That Are Not Cancer
What is prostatitis and how is it treated?
What is enlarged prostate or BPH?
How can BPH be treated?
Prostatitis (pronounced "PRAH-stuh-TYE-tis") is an inflammation or
infection of the prostate gland. It affects at least half of all men at
some time in their lives. Having this condition does not increase
your risk of any other prostate disease.
| Prostatitis Symptoms |
- Trouble passing urine or pain when passing urine
- A burning or stinging feeling when passing urine
- Strong, frequent urge to pass urine, even when there
is only a small amount of urine
- Chills and high fever
- Low back pain or body aches
- Pain low in the belly, groin, or behind the
scrotum
- Rectal pressure or pain
- Urethral discharge with bowel movements
-
Genital
and rectal throbbing
- Sexual problems and loss of sex drive
- Blocked urine
- Painful ejaculation (sexual climax)
|
Prostatitis is not contagious. It is not spread through sexual
contact. Your partner cannot catch this infection from you.
Several tests, such as DRE and a urine test, can be done to see if
you have prostatitis. Getting the right diagnosis of your exact type
of prostatitis is the key to getting the best treatment. Even if you
have no symptoms, you should follow your doctor's suggestion to
complete treatment.
There are four types of prostatitis:
-
Acute bacterial prostatitis
This infection comes on suddenly (acute) and is caused by
bacteria. Symptoms include severe chills and fever. There is often
blood in the urine. You must go to the doctor's office or
emergency room for treatment. It's the least common of the four
types, yet it's the easiest to diagnose and treat.
|
Treatment: | |
Most cases can be cured with a high dose of
antibiotics, taken for 7 to 14 days, and then lower
doses for several weeks. You may also need drugs to
help with pain or discomfort.
|
-
Chronic bacterial prostatitis
Also caused by bacteria, this condition doesn't come on suddenly,
but it can be bothersome. The only symptom you may have is
bladder infections that keep coming back. The cause may be a
defect in the prostate that lets bacteria collect in the urinary tract.
|
Treatment: | |
Antibiotic treatment over a longer period of time is
best for this type. Treatment lasts from 4 to 12 weeks.
This type of treatment clears up about 60 percent of
cases. Long-term, low-dose antibiotics may help
relieve symptoms in cases that won't clear up.
|
-
Chronic prostatitis or chronic pelvic pain
syndrome
This disorder is the most common but least understood form of
the disease. Found in men of any age from late teens to elderly, its
symptoms go away and then return without warning. There can
be pain or discomfort in the groin or bladder area.
|
Treatment: | |
There are several different treatments for this
problem, based on your symptoms. These include
antibiotics and other medicines, such as
alpha-blockers.
Alpha-blockers relax muscle tissue in the
prostate to make passing urine easier.
|
-
Asymptomatic inflammatory prostatitis
You usually don't have symptoms with this condition. It is often
found when your doctor is looking for other conditions like
infertility
or prostate cancer. If you have this problem, often
your PSA test (see The PSA Test) will show a higher number than
normal. It does not necessarily mean that you have cancer.
|
Treatment: | |
Men with this condition are usually given antibiotics
for 4 to 6 weeks, and then have another PSA test.
|

"Changes happen so slowly that you don't
even realize they're happening."
BPH stands for benign prostatic hyperplasia (pronounced "be-NINE
prah-STAT-ik HY-per-PLAY-zha").
Benign means "not cancer," and hyperplasia means too much
growth. The result is that the prostate becomes enlarged. BPH is
not linked to cancer and does not raise your chances of getting
prostate cancer--yet the symptoms for BPH and prostate cancer
can be similar.
| BPH Symptoms |
BPH symptoms usually start after the age of 50.
They can include:
- Trouble starting a urine stream or making more than a
dribble
- Passing urine often, especially at night
- Feeling that the bladder has not fully emptied
- A strong or sudden urge to pass urine
- Weak or slow urine stream
- Stopping and starting again several times while passing urine
- Pushing or straining to begin passing urine
At its worst, BPH can lead to:
- A weak bladder
- Backflow of urine causing bladder or kidney infections
- Complete block in the flow of urine
- Kidney failure
|
BPH affects most men as they get older. It can lead to urinary
problems like those with prostatitis. By age 60, many men have
signs of BPH. By age 70, almost all men have some prostate
enlargement.
The prostate starts out about the size of a walnut. By the time a
man is 40, it may have grown slightly larger, to the size of an
apricot. By age 60, it may be the size of a lemon.
As a normal part of aging, the prostate enlarges and can press
against the bladder and the urethra. This can slow down or block
urine flow. Some men might find it hard to start a urine stream,
even though they feel the need to go. Once the urine stream has
started, it may be hard to stop. Other men may feel like they need
to pass urine all the time or are awakened during sleep with the
sudden need to pass urine.
Early BPH symptoms take many years to turn into bothersome
problems. These early symptoms are a cue to see your doctor.
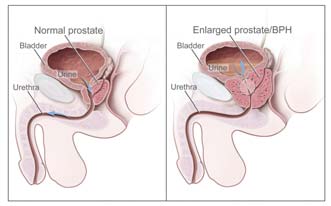
Urine flow of normal (left) and enlarged prostate (right). In diagram on
the left, urine flows freely. On the right, urine flow is affected because of
the prostate pressing on the bladder and urethra.
About half the men with BPH eventually have symptoms that are
bothersome enough to need treatment. BPH cannot be cured, but
drugs or surgery can often relieve its symptoms. BPH symptoms
do not always grow worse.
There are three ways to manage BPH:
- Watchful waiting (regular follow-up with your doctor)
- Drug therapy
- Surgery
Talk with your doctor about the best choice for you. Your
symptoms may change over time, so be sure to tell your doctor
about any new changes.
Watchful waiting
Men with mild symptoms of BPH who do not find them
bothersome often choose this approach.
Watchful waiting means getting annual checkups. The checkups
can include DREs and other tests (see "Types of Tests"). Treatment is
started only if symptoms become too much of a problem.
If you choose to live with symptoms, these simple steps can help:
- Limit drinking in the evening, especially drinks with
alcohol or caffeine.
- Empty the bladder all the way when you pass urine.
- Use the restroom often. Don't wait for long periods
without passing urine.

"My doctor and I decide visit by visit about
how long I should stay on watchful waiting
for my BPH.
Some medications can make BPH symptoms worse, so talk with
your doctor or pharmacist about any medicines you are taking
such as:
- Over-the-counter cold and cough medicines (especially
antihistamines)
- Tranquilizers
-
Antidepressants
- Blood pressure medicine
Drug therapy
Millions of American men with mild-to-moderate BPH symptoms
have chosen prescription drugs over surgery since the early 1990s.
There are two main types of drugs used. One type relaxes muscles
near the prostate while the other type shrinks the prostate gland.
There is evidence that shows that taking both drugs together may
work best to keep BPH symptoms from getting worse.
Alpha-blockers
These drugs help relax muscles near the prostate to relieve pressure
and let urine flow more freely, but they don't shrink the size of the
prostate. For many men, the drug can improve urine flow and
reduce symptoms within days. Possible side effects include
dizziness, headache, and fatigue.
5 alpha-reductase inhibitor
This drug, known as
finasteride, shrinks the prostate. It relieves
symptoms by blocking an
enzyme
that acts on the male
hormone, testosterone, to boost organ growth. When the
enzyme
is blocked, growth slows down. This helps shrink the prostate,
reduce blockage, and limit the need for surgery.
Taking this drug for at least 6 months to 1 year can increase urine
flow and reduce your symptoms. It seems to work best for men
with very large prostates. You must continue to take the drug to
prevent symptoms from coming back.
This drug is also used to treat baldness in men. It can cause these
side effects in a small percentage of men:
- Decreased interest in sex
- Trouble getting or keeping an
erection
- Smaller amount of semen with ejaculation
It's important to note that taking this drug can lower your PSA test
levels. There is also evidence that finasteride lowers the risk of
getting prostate cancer, but whether it lowers the risk of dying
from prostate cancer is still unclear.
| BPH Medications |
| Category |
Activity |
Generic Name |
Brand Name |
| Alpha-blockers |
Relax muscles
near prostate |
doxazosin
tamsulosin
terazosin
prazosin
|
Cardura
Flomax
Hytrin
Minipres
|
| 5 alphareductase
inhibitor |
Slows prostate growth, shrinks
prostate |
finasteride |
Proscar or
Propecia |
BPH surgery
The number of prostate surgeries has gone down over the years.
But operations for BPH are still one of the most common surgeries
for American men. Surgery is used when symptoms are severe or
drug therapy has not worked well.
Types of surgeries include:
-
TURP (transurethral resection of the prostate) is the most
common surgery for BPH. It accounts for 90 percent of all
BPH surgeries. It takes about 90 minutes. The doctor passes
an instrument through the urethra and trims away extra
prostate tissue. A
spinal block
is used to numb the area.
Tissue is sent to the laboratory to check for prostate cancer.
TURP generally avoids the two main dangers linked to other
prostate surgeries:
- Incontinence (not being able to hold in urine)
- Impotence (not being able to have an erection)
The recovery period for TURP is much shorter as well.
-
TUIP (transurethral incision of the prostate) is similar to
TURP. It is used on slightly enlarged prostate glands. The
surgeon places one or two small cuts in the prostate. This
relieves pressure without trimming away tissue. It has a low
risk of side effects. Like TURP, this treatment helps with urine
flow by widening the urethra.
-
TUNA (transurethral needle ablation) burns away excess
prostate tissue using radio waves. It helps with urine flow,
relieves symptoms, and may have fewer side effects than TURP.
Most men need a
catheter
to drain urine for a period of time
after the procedure.
-
TUMT (transurethral microwave thermotherapy) uses
microwaves sent through a catheter to destroy excess prostate
tissue. This can be an option for men who should not have
major surgery because they have other medical problems.
-
TUVP (transurethral electroevaporation of the prostate)
uses electrical current to vaporize prostate tissue.
-
Open prostatectomy means the surgeon removes the prostate
through a cut in the lower abdomen. This is done only in very
rare cases when obstruction is severe, the prostate is very large,
or other procedures can't be done. General or spinal
anesthesia is used and a catheter remains for 3 to 7 days after
the surgery. This surgery carries a higher risk of complications
than medical treatment. Tissue is sent to the laboratory to
check for prostate cancer.
Be sure to discuss options with your doctor and ask about the
potential short- and long-term benefits and risks with each
procedure. For a list of questions to ask, see
Checklist of Questions for Your Doctor.
Back to Top
< Previous Section | Next Section > |