Introduction
Facts about Prostate Cancer
Thinking About Treatment Choices
Comparing Your Treatment Options
1. What factors might help me decide on the treatment that is right for me?
2. What are the medical terms for these treatment options?
3. What happens during treatment?
4. What are the benefits of this treatment option?
5. What are the side effects and risks of this treatment option?
6. How will this treatment affect my ability to have sex, an erection for sex, or get a woman pregnant?
7. How can I live with side effects? What can be done to help?
8. Is this treatment painful? What can be done to help with pain?
9. What other treatment will I need and how long will I need it?
10. What if my treatment doesn't work?
11. How long can I expect to live after I have this treatment?
Making a Choice About Treatment
Resources
Introduction
As a man with early-stage
prostate cancer, you will be
able to choose which kind of
treatment is right for you.
There can be several
reasonable options, which can
make the decision difficult.
And each choice has its pros
and cons.
Active treatment usually
begins a few weeks to months
after diagnosis. During this
time, you should meet with
various doctors to learn about
your treatment choices. Use
this article to help you talk
over possible treatments with
your doctor before deciding which is best for you.
You will want to think about what is important to you. It's
also a good idea to include your spouse or partner in your
decision-making process. After all, a diagnosis of cancer and
the treatment choice you make affect both of you.
Terms that may be new to you appear in bold type.
|
This booklet is meant to
be a starting point.
Its purpose is to help you
learn about early-stage
prostate cancer, current
treatments, and the pros
and cons of each treatment.
But most men will need
more information than this
booklet gives to reach their
decisions. For a list of
organizations that provide
more information and
support, please see the
Resources section. If your prostate cancer
has spread beyond the
prostate, or if it has
returned after treatment,
also refer to this section.
|
Many men with prostate cancer have shared their
advice to help other men who are newly diagnosed:
- There are treatment options--be sure to know them all.
- Treatments and medical procedures have improved over
the past 10 years.
- You must make the decision that is right for you--not
your doctor.
- Seek the opinions of several different doctors since
some may only recommend the option they know the
most about.
- Take the time you need to research your options before
making your decision. There's usually no need to rush.
- Your spouse or partner has an important role in your
decision and will be affected by your choice. Try to be
open and honest with each other about your concerns.
- Organizations and support groups can help you learn
more about what others in your situation are doing for
their prostate cancer.
- It is possible to live a full life after prostate cancer.
|
"When my doctor said
watch and wait,
I thought he meant that I should give
up. But after he explained my stage of
cancer, it made sense to me. It doesn't mean
giving up or never having treatment."
|

| "I talked it over with my wife and son.
I chose radiation therapy because we
thought that it had the best potential
for my situation." |

| "My wife and I looked at the pros and
cons of each treatment. In talking with
several doctors who specialize in
prostate cancer, we concluded that
surgery was the best option for me." |
 Back to Top Back to Top
Facts about Prostate Cancer
Early-stage prostate cancer means that cancer cells are found
only in your prostate gland. Compared with many other
cancers, prostate cancer tends to grow more slowly. This
means that it can take 10 to 30 years before a tumor gets big
enough to be found or cause problems (or symptoms).
Older men who have prostate cancer often die of something
else, not of prostate cancer.
- Prostate cancer is most often diagnosed in men 65
and older, although younger men can be diagnosed
with it as well.
- By age 80, more than half of all men have some cancer
in their prostate.
- African American men tend to be diagnosed at
younger ages with more aggressive prostate cancer
than men of other races.
Today, prostate cancer is most often found in earlier stages.
There are a number of treatment options available.
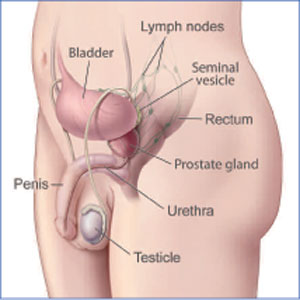
The prostate is a small gland in a man's reproductive
system. It helps make semen - the milky fluid that
carries sperm from the testicles through the penis
when a man ejaculates.
The prostate is about the size and shape of a walnut.
It lies low in the pelvis, below the bladder and in front
of the rectum. The prostate also encircles part of the
urethra, the tube that carries urine out of the bladder
and through the penis.
 Back to Top Back to Top
Thinking About Treatment Choices
Watchful waiting, surgery, and radiation therapy are the
standard treatment choices for early-stage prostate cancer
(see Types of Treatment). Each has benefits (how
treatment can help) and risks (problems treatment may
cause). There is seldom just one "right" treatment choice.
"The bottom line is to have enough information
to know what treatment to choose."
- Ken
Treatment choices depend on several factors:
Prostate cancer characteristics. This includes the size
of your prostate, prostate-specific antigen (PSA) score,
Gleason score, and stage of cancer. (Go to Medical Tests
and Terms to learn more.) Health problems, other than prostate cancer.
This means whether you have heart problems, diabetes,
or other illnesses or have had a previous surgery for an
enlarged prostate. Having such health problems may
affect which treatment you choose. Age. If you are older, you may view treatment choices
differently than younger men because the benefits and
risks of treatment vary with age. Type of care available to you. The skills of specialists
and types of treatment can vary. You will need to ask
what you may feel are tough questions to make sure that
you get the best care and outcomes. See Talking with Your Medical Team and Asking Questions for questions to ask. Balancing what you value most.Your unique
experiences in life shape your feelings and perceptions
about how to deal with your prostate cancer. Keep in
mind what is important to you personally to help guide
your decision.
Many men may ask their doctor, "What would you do, if
you were me?" Try to remember, the doctor isn't you and
his or her personal values may be different from yours.
How do you view the potential risks and benefits of the
treatment options offered to you? Are you a person who
could cope with knowing cancer is in your body? Would
you rather have the cancer treated and know that there
could be side effects? Do you know of other men's
experiences with prostate cancer that may influence
your decision? Spouse or partner. Even though the treatment
decision is yours, involve your spouse, partner, or
caregiver to help you sort out what is most important
to you and your family. Your treatment choice will
affect your spouse or partner.
By now you may have had several tests to find out the extent
of your cancer. Your doctor will take into account your
physical exam, PSA level, Gleason score, and stage when
discussing your treatment options. What do these mean?
Prostate-Specific Antigen (PSA) test. PSA is a
protein made by normal cells and prostate cancer cells.
PSA is found in the blood and is measured with a blood
test. Doctors sometimes watch the rate of change in
your PSA levels over time. A score of 4 nanograms (ng)
or higher is often the trigger for further tests. Gleason score of your biopsy. When you had a biopsy,
tissue samples (called "cores") were taken from several
areas in your prostate. The pathologist checked for
cancer in the samples using a microscope. He or she can
also estimate how much cancer there is by looking
at how many tissue samples are positive. A Gleason
score (or sum) on a scale of 2 to 10 is assigned to the
cancer. This score tells how different the prostate cancer
tissue looks from the normal prostate tissue and helps
estimate how likely it is that the tumor cells will spread
(how aggressive the cancer is).
A low-risk score is 2 to 4. A low score means that the
cancer tissue still looks similar to normal prostate tissue,
and the tumor cells are less likely to spread. A score of 5
to 7 means moderate risk, while a score of 8 to 10 means
higher risk. As the score gets higher, it means that the
prostate cancer tissue becomes more and more different
from normal tissue and that the tumor cells are more
likely to spread.Most men with early-stage prostate
cancer have a Gleason score of 5, 6, or 7. Stage. The stage of cancer is an important factor in
choosing a treatment. The stage tells how much the
cancer may have grown within the prostate and
whether it has spread to other tissues or organs.
Doctors use a standard rating system to describe the
stage, called the TNM System. T means the size of the
main tumor, N means whether nearby lymph nodes are
involved, and M means whether the cancer has spread
beyond the region around the prostate.
First, the doctor will assess the stage of your prostate
cancer based on clinical findings (such as a physical
exam, digital rectal exam, or DRE, and biopsy). If you
have surgery to remove your prostate, seminal vesicles
or nearby lymph nodes, then your cancer can be
assessed from a pathologic stage. This means that by
looking at what is removed, doctors are better able to
predict your outcome and survival.
Your doctor may also suggest other tests such as a bone
scan, MRI, CT scan, removing lymph nodes in the
pelvis, or a seminal vesicle biopsy.
Prostate cancer tumor stages range from stage T1 to T4.
They may also be further classified a, b, or c. This
article addresses early stages, which are Stage T1 and
T2, where the cancer is confined to the prostate.
|
|
|
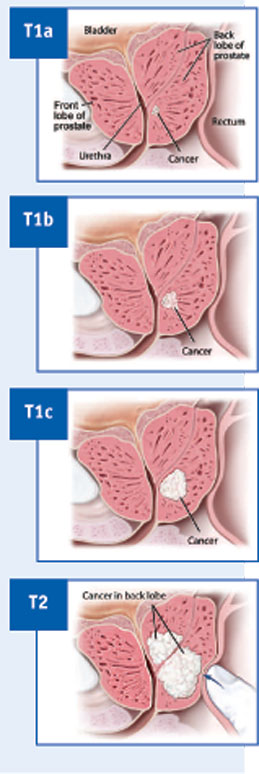 Sometimes cancer is found
"by accident," or incidentally
(called T1a or T1b) when
men have surgery to correct
a non-cancerous prostate
enlargement. T1 means that a
tumor is not usually felt
during a digital rectal exam. Sometimes cancer is found
"by accident," or incidentally
(called T1a or T1b) when
men have surgery to correct
a non-cancerous prostate
enlargement. T1 means that a
tumor is not usually felt
during a digital rectal exam.
Since most prostate cancer
is found through PSA
testing, T1c is the stage
most often diagnosed
through biopsy.
A stage of T2 means that
prostate cancer can be felt
during a digital rectal exam
but that it is still confined
to the prostate gland. Your
doctor may also assign a, b,
or c stages depending on
the cancer's size and
location in the prostate.
|
Surgery is often a treatment choice for men who have earlystage
prostate cancer and are in good health. Surgery to
remove the prostate is called prostatectomy (PRAHS-ta-
TEK-toe-mee). There are two approaches that are typically
used by surgeons:
| Other Options |
|
Cryosurgery freezes and thaws tissue to kill prostate cancer
with the surgeon being guided by ultrasound. Also called
cryotherapy, it is often used when the prostate has more
advanced, yet still confined disease, and when surgery is not
an option. The prostate is not removed with this approach.
Cryosurgery can result in injury to the rectum, incontinence,
swelling of the scrotum, pain or numbness in the penis, or
blocked urine flow. In 1 in 200 cases, a hole (called a fistula)
appears between the rectum and prostate. Results depend
highly on the doctor's skill and experience. Success rates may
not be as high as with prostatectomy or with any form of
external beam radiation therapy. Long-term results for this
type of treatment are not yet known.
Laparoscopic surgery is the newest type of surgery to
remove the prostate. It is done with smaller incisions using a
slender tube with a camera on the end (laparoscope), which
may be robotically controlled. The scope is inserted through
the navel, and the surgeon can see a highly enlarged image of
the prostate. Compared with other types of prostatectomy, this
technique may lead to shorter hospital stays, faster recovery,
and less blood loss and pain. However, it is fairly new and not
widely used. Some surgeons have limited experience with this
type of surgery. Since it is newer, researchers have not had the
chance to follow its effectiveness for as long as they have for
standard surgery.
|
This type of treatment uses high doses of radiation energy
to treat cancer. Radiation therapy is an option when cancer
is in your prostate but has not spread to other organs. It is
also used when you cannot have surgery because of your
age, health, or personal choice. There are two types of
radiation therapy:
- External beam radiation. A machine aims radiation at
your cancer cells. It rotates around your body, sending
radiation from many directions. After the doctor maps
out the exact part of your body that needs radiation,
treatment usually happens once a day, 5 days a week,
for 6 to 8 weeks. Each treatment session usually lasts
about 15 minutes. The latest types of radiation are
called 3-D Conformal Radiation Therapy and
Intensity-Modulated Radiation Therapy (IMRT).
These types of radiation are more precise in destroying
cancer while leaving nearby healthy cells unharmed.
They are designed to lower the exposure of the rectum
and bladder to radiation to help lessen side effects.
- Brachytherapy (BRA-kee-THAYR-uh-pee). This is a
type of internal radiation therapy. It is also called
seed implants. Radiation is delivered inside your body by
implanting tiny seeds in your prostate. Usually 40 to
130 seeds are inserted into the prostate, depending on
the size of your prostate. Each seed has a small amount
of radioactive material that emits radiation within an
inch of its surroundings. Low-dose seeds are left in the
prostate permanently, although their radiation lasts for
only 3 to 6 months. This procedure is usually done on
an outpatient basis, without a hospital stay.
Both types of radiation can be used together (placing
radioactive seeds internally and using external beam
radiation to kill any cancer that may be close to the
prostate) or with hormone therapy.
Watchful waiting is often called "active surveillance" or
"observation" and means that you decide to have no active
treatment now. Your doctor will want to follow you closely
to look for any signs that the disease may be changing. You
will have tests like the ones you've already had such as
digital rectal exams, PSA tests, and repeat biopsies. You can
change your mind and decide to have treatment at any time.
Watchful waiting is based on the fact that many early-stage
prostate cancers grow so slowly that they may never cause
problems or become life threatening. In some cases, it
may be a way to avoid the harms of treatment without
shortening life expectancy. Or it can be a decision based on
your age and other serious health problems - older men in
their 70s and 80s may not have the same views about
undergoing surgery or radiation therapy as younger men.
| About Hormone Therapy |
|
Hormone therapy may be used in combination with other
treatment, such as radiation therapy, when the tumor is large.
Male sex hormones such as testosterone make prostate
tumors grow. Hormone therapy slows a tumor's growth by
stopping or blocking testosterone from entering the cancer
cells. Hormone therapy can be given for several years. Side
effects usually occur during treatment, but they go away after
treatment is over. Side effects may include loss of sex drive,
impotence, and hot flashes.
|
The chart in the next section lists common questions and answers
for the three options outlined in this booklet. As mentioned
earlier, most men will need more information than this
booklet gives to reach their decisions. You may use this
chart as a guide for talking with your doctor or researching
your options.
 Back to Top Back to Top
Comparing Your Treatment Options
Below are some questions you may be thinking about. Click on the question to learn more.
Regardless of the treatment you choose, you will continue to have
PSA tests for monitoring.
| For More
Information |
| For more information about treatment options or
clinical trials for prostate cancer, visit NCI's Web site
at www.cancer.gov/cancertopics/types/prostate
or call the National Cancer Institute's Cancer
Information Service toll-free at 1-800-4-CANCER
(1-800-422-6237). |
Below is a list of types of doctors who treat or specialize in prostate
cancer (also see Talking With Your Medical Team):
- Medical oncologist. A doctor who specializes in diagnosing and
treating cancer using chemotherapy, hormonal therapy, and
biological therapy. This doctor is often the main health care
provider for people with cancer. He or she can also give supportive
care and may coordinate treatment given by other specialists.
- Pathologist. A doctor who finds diseases by studying cells and tissue
under a microscope. Although you won't personally interact with this
doctor, he or she writes up a pathology report, which contains the
cancer information from your biopsy or prostate surgery.
- Radiation oncologist. A doctor who specializes in using radiation
to treat cancer.
- Urologic oncologist. A doctor who specializes in treating cancers of
the urinary system.
- Urologist. A doctor who specializes in diseases of the male urinary
system and sex organs.
 Back to Top Back to Top
1. What factors might help me decide on the treatment that is right for me?
| Watchful
Waiting | If you have a smaller or slow-growing type of prostate
cancer confined to the prostate, and it is considered
low risk
If you are in your 70s or older, or have serious
medical problems
If you are able to live with the fact that you have
cancer in your body
If you can be vigilant about going to your check-ups |
| Surgery | If you are younger than 70 and in good health
If you want the cancer cells removed
If you are able to accept that serious side effects
often happen with surgery |
| Radiation
Therapy | If you are a man of any age with early-stage
prostate cancer
If you are unable to choose surgery because of other
serious medical conditions
If you are able to go for treatment 5 days a week for
6 to 8 weeks |
Back to Questions List
|
Next Question
>
 Back to Top Back to Top
2. What are the medical terms for these treatment options?
| Watchful
Waiting | Also called active surveillance or observation |
| Surgery |
- Prostatectomy
- Retropubic
- Perineal
- Cryosurgery (or cryotherapy)
- Laparoscopic prostatectomy
|
| Radiation
Therapy |
External Beam Radiation
- 3-D Conformal Radiation Therapy
- Intensity-Modulated Radiation Therapy (IMRT)
Brachytherapy or Seed Implants - low dose or
high dose |
< Previous
Question |
Back to Questions List
|
Next Question
>
 Back to Top Back to Top
3. What happens during treatment?
| Watchful
Waiting | You will not start active treatment.
You will have regular visits to the doctor and
examinations.
You and your doctor will watch for signs that the
cancer may be changing.
You may repeat the same tests you had before, such
as DREs and PSA tests. |
| Surgery | Surgery takes about 2 to 4 hours.
Most patients stay in the hospital for 2 to 4 days.
After surgery, you will need to use a catheter (tube to
drain your urine) for 1 to 2 weeks. |
| Radiation
Therapy | External Beam Radiation
- Your doctor will calculate the dose of the radiation
beam to the cancer location while trying to avoid
the nearby normal tissue.
- You will lie on a table while a large machine with a
beam targets your cancer cells using radiation.
- Each session takes about 15 minutes and is given
daily for 5 days a week for 6 to 8 weeks.
Brachytherapy or Seed Implants
- Radioactive seeds (the size of grains of rice) are
inserted into the prostate or surrounding area
using hollow needles through the space between
the scrotum and the anus.
- It takes 1 to 2 hours with spinal or general
anesthesia.
- The seeds are left in permanently.
|
< Previous
Question |
Back to Questions List
|
Next Question
>
 Back to Top Back to Top
4. What are the benefits of this treatment option?
| Watchful
Waiting | There are no side effects to manage such as bladder
or bowel control or impotence.
You can decide to begin treatment at any time. |
| Surgery | Prostate cancer cells are removed. |
| Radiation
Therapy |
External Beam Radiation
- No hospital stay
- No anesthesia risk
- May have fewer urine problems than with surgery
- Similar effectiveness to surgery over a
10-year period.
Brachytherapy or Seed Implants
- No hospital stay
- Can be easier on your body than surgery
- Less damage to the rectum and surrounding tissue
than external beam radiation.
Both types of radiation can be used together (placing
radioactive seeds internally and using external beam
radiation to kill any cancer that may be close to the
prostate) or with hormone therapy. |
< Previous
Question |
Back to Questions List
|
Next Question
>
 Back to Top Back to Top
5. What are the side effects and risks of this treatment option?
| Watchful
Waiting |
You may have feelings of worry and anxiety about
living with cancer and not treating it.
The cancer needs to be followed closely - it could
spread and become harder to treat. |
| Surgery |
There are risks with any surgery, such as bleeding,
infection, heart problems, or death.
Recovery is longer than with radiation.
Problems holding and passing urine, called
incontinence, can occur. Managing this often means
wearing pads to catch urine. The most common type
of incontinence is passing a small amount of urine
from the stress of coughing, laughing, or sneezing.
A small number of men may have more serious
incontinence that can be lifelong.
Problems getting or keeping an erection (impotence
or erectile dysfunction or
ED) can occur. Most men
should expect a decline in being able to get an erection
after surgery.
If your tumor is too close to the nerves that control
erections, the nerves could be damaged or removed.
This means that there is a strong chance of problems
with sexual potency after surgery.
Your age and prior strength of erections can affect
erectile dysfunction that result from surgery. |
| Radiation
Therapy | External Beam Radiation
During Treatment
- Fatigue (being extremely tired)
- More frequent and loose bowel movements
(fecal incontinence) or urinary problems
- Rectal irritation or bleeding.
After Treatment
- Loss of sexual function within 5 years of treatment
in half of those treated; potency rates are closer to
surgery after that time.
- This type of therapy also causes more bowel problems
than prostatectomy or brachytherapy.
- After treatment, there can be a temporary increase
in the PSA reading.
- If radiation does not get rid of the cancer, surgery
can be more difficult due to scarring around the
prostate from radiation.
Brachytherapy or Seed Implants
During Treatment
- More frequent passing of urine, especially at night
- More discomfort when passing urine
- Can affect bowel function and cause serious
problems in some men
- Delayed onset of sexual problems
- Impotence, as can occur with external beam
radiation.
After Treatment
- Urinary problems can occur.
|
< Previous
Question |
Back to Questions List
|
Next Question
>
 Back to Top Back to Top
6. How will this treatment affect my ability to have sex, an erection for sex, or get a woman pregnant?
| Watchful
Waiting | It should not affect your sex life. |
| Surgery |
Having the prostate removed can affect getting
erections. Talk with your doctor about whether nerve-sparing
surgery can be used to allow the nerves that
control erections to be kept. Medications and devices
can help with impotence in many men.
After surgery, the orgasm may be "dry," meaning no
ejaculation. If you are interested in having children,
you will need to preserve your sperm (sperm
banking) before surgery (see the
Resources
section for a list of
resources for more information). |
| Radiation
Therapy | There is less risk of impotence with radiation therapy,
but over time it may become a problem. Your age and
overall health can affect impotence. |
< Previous
Question |
Back to Questions List
|
Next Question
>
 Back to Top Back to Top
7. How can I live with side effects? What can be done to help?
| Watchful
Waiting | There are no side effects. |
| Surgery |
Knowing the possible side effects you may have
before surgery is very important.
Medicines such as sidenafil (Viagra®), vardenafil
(Levitra®), and tadalafil (Cialis®) increase blood flow
to the penis, leading to an erection.
Injection therapy (or shots) can help with getting an
erection. Medicine is self-injected with a needle into
the penis to produce an erection. The drug takes about
5 minutes to work and lasts for 20 to 90 minutes.
For men who don't do well with either oral medicine
or injection therapy, they should talk with their
doctor about other options. This includes MUSE
(medicated urethral system for erection), where a
small pellet is inserted into the urethra using an
applicator to help with erections. Vacuum erection
devices or penile implants can be other options to
help with erections.
Lack of bladder control may be severe for about 6 to
12 weeks after surgery. During this time, you will need
to wear a pad. Emptying your bladder often may help
to control leaks. Other options for managing
incontinence include absorbent products, collection
devices, biofeedback, and various surgical options. |
| Radiation
Therapy | Bladder and bowel function may be affected, but
there are bladder muscle exercises and medications
that can help. |
< Previous
Question |
Back to Questions List
|
Next Question
>
 Back to Top Back to Top
8. Is this treatment painful? What can be done to help with pain?
| Watchful
Waiting | There is the discomfort of additional testing. |
| Surgery | Some men have little pain after surgery, while
others need pain relief. If you feel pain, your doctor
can help control it using various medications. |
| Radiation
Therapy | External beam radiation therapy itself does not cause
pain, but over time it can cause side effects that
cause discomfort. Medications can help with
discomfort or pain.
For seed implants, men may pass urine more often,
notice a slower stream, or feel some pain. Medicine
can help treat these symptoms. |
< Previous
Question |
Back to Questions List
|
Next Question
>
 Back to Top Back to Top
9. What other treatment will I need and how long will I need it?
| Watchful
Waiting | Hormone therapy may be used for a rising PSA. |
| Surgery | Hormone therapy may be used before surgery to
shrink the prostate. |
| Radiation
Therapy | Hormone therapy may be used to shrink the prostate
before radiation therapy and for several years after
radiation. |
< Previous
Question |
Back to Questions List
|
Next Question
>
 Back to Top Back to Top
10. What if my treatment doesn't work?
| Watchful
Waiting | This allows monitoring of the cancer for an increase
in symptoms or PSA. |
| Surgery | The final surgery pathology report will tell whether
the cancer was confined to the prostate or was found
in lymph nodes or seminal vesicles. But even with a
microscope, it may not be possible for the surgeon to
see all of the cancer.
Some men who have surgery may need additional
treatment within 5 years.
If surgery fails, hormone therapy can be a successful
treatment option. |
| Radiation
Therapy | Radiation therapy may fail if the tumor cannot be
seen completely in the planning process. Some men
who had radiation therapy will need hormone therapy
or a prostatectomy within 5 years. |
Regardless of the treatment you choose, you will continue to have PSA tests for monitoring.
< Previous
Question |
Back to Questions List
|
Next Question
>
 Back to Top Back to Top
11. How long can I expect to live after I have this treatment?
| Watchful
Waiting,
Surgery,
and
Radiation
Therapy | Depending on age and the nature of the disease, a
man with cancer confined to the prostate can lead a
long and healthy life.
The 5-year survival rate for men with early-stage
prostate cancer is nearly 100 percent. The 10-year
survival rate is 86 percent and the 15-year survival
rate is 56 percent. The average age of men at
diagnosis is 65 years old.
And even if the cancer comes back, there are many
treatment options that are known to be effective. |
< Previous
Question |
Back to Questions List
 Back to Top Back to Top
Making a Choice About Treatment
Most prostate cancers found in the early stages grow slowly.
This means that you usually do not have to rush when
making a treatment choice. Often, you have several weeks
to several months from the time you first learn you have
prostate cancer until you have to make a choice.
Many men use this time to find out more about prostate
cancer treatment options. Be sure to find all of the
information you need to answer your questions and be
comfortable with your decision.
It may be helpful to use this extra time to attend a prostate
cancer support group to talk with other men who have
faced the same decision-making process. The Resources Section lists the National Cancer Institute's toll-free numbers to call
and request contact information for prostate
cancer organizations.
Studies show that men felt better about their treatment
decision when they took part in making their own
treatment choice. But making this choice can be hard to do.
The following are some ideas that may help.
Here are some things to keep in mind:
- Questions. Ask your doctor or nurse questions that you
are thinking about, but that you normally may not feel
comfortable asking. These questions can be about topics
that are new to you or side effects that concern you. For
example,"How many operations (prostatectomies) do
you do a month?"Make sure you understand the
answers, or ask your doctor or nurse to explain in other
ways such as with pictures, models, or charts. (See Asking Questions
for a list of key questions to ask.)
- Health history. This includes your age, family history,
health (other than cancer), and whether you have any
other illness, such as diabetes or heart problems, or
have had a previous prostate surgery.
- Cancer history. You will talk about your prostate
cancer in terms of PSA number, grade, Gleason score,
and stage. This means size, location of the cancer, and
what it looks like under the microscope. (To learn more about these terms, see
Medical Tests and Terms)
- Treatment choices. It's important to ask your doctors
about all the treatment options that are available to you.
This includes benefits (how each treatment can help)
and long- and short-term side effects. This may even
include the small risk of death from surgery.
- Your part in making a choice. Men who actively take
part in their treatment tend to have fewer regrets than
men who let others decide for them. Let your health
provider know how active you want to be in making
this choice.
- What is important to you. Keep in mind what's
important to you and what worries you. This is also a
good time for you and your spouse or partner to have
an open, honest discussion with each other about your
treatment choices and their side effects.
- Ask a family member or trusted friend or caregiver
to come to appointments with you. This person can
help listen, ask questions, take notes, and talk with you
about what your doctor or nurse said.
- Bring a copy of your pathology report. Make sure to
ask your doctor for a copy of this report and bring a
copy with you when you see new doctors. Your
pathology report includes the results of tests that
describe details about your cancer. If you are seeing a
new doctor, it's important to bring all the information
he or she requests to your visit.
"Investigate all your options and be
comfortable with the choice you make,
because you can't second guess
when it's all over."
- Lawrence
- Get a second or even third opinion. Seeking other
opinions means talking about prostate cancer treatment
with doctors you are not working with now. You may
want to talk with other prostate cancer specialists, such
as a urologist, urologic oncologist, surgeon, medical
oncologist, internist, or radiation oncologist.
Getting second and third opinions can be confusing,
because you may get different advice or opinions.
Because of this, many men find it helpful to see a
medical oncologist for a general view of prostate cancer
treatment options. Talking with other doctors can give
you ideas to think about or help you feel better about
the choice you are making.Most insurance companies
pay for second opinions. It is better to get a second
opinion than worry that you made the wrong choice.
"When you are faced with a medical decision
like this, you almost want to put yourself in the
hands of the expert. But it's really a decision
that you have to make, and you have to make it
on an informed basis and seek out more than
one opinion from a doctor."
- Paul
Many men with prostate cancer find that it helps to learn
a lot about their disease and its treatment. Doing so can
help you feel more in control and at ease with your
treatment choice.
You can learn more by reading books and articles, searching
the Internet, or calling organizations that focus on prostate
cancer. But too much information can sometimes be
overwhelming or confusing as you are adjusting to your
diagnosis. Instead, learn as much as you want to know at a
time when you are ready. Later, you can always find out
more. Let your doctor or nurse know what else you need to
know to be comfortable reaching a decision.
Some men want to read books and articles that outline the
current research on prostate cancer treatment options.
Others prefer to meet with men at support groups who
have had prostate cancer to learn how they made their
treatment choices. Some men may not want information or
want to talk about it at first - only later are they ready for
more information. All of these approaches are natural
reactions to coping with a diagnosis of prostate cancer.
For more details, see the fact sheet "How to Evaluate Health
Information on the Internet: Questions and Answers" at
www.cancer.gov, search term "Internet." Also see Resources for more information.
It's natural to feel many emotions at this time. Sometimes
you may have many strong feelings at once, while at other
times, you may feel overwhelmed or angry. Your spouse or
partner will also feel a range of emotions but may not have
the same emotions at the same time as you do.
A diagnosis of prostate cancer can stir up many feelings,
such as fear of the cancer getting worse or of dying. You
may also worry about changes to your body or being
intimate with your spouse or partner.Many men describe a
feeling of loss - loss of the life they had before cancer, loss
of energy levels, or the physical loss of the prostate. These
feelings are a natural part of the coping process.
Your spouse or partner may be worried about losing you,
changes to your lives, and how to best give you the support
you need. They may want to talk about it more than you
want to at first. If you find that you need time to adjust and
sort out your feelings and values, let your spouse or partner
and family know your needs. Chances are that they are also
trying to cope with the news and may not know how best
to help you. If you are holding your worries and feelings
inside for too long and your silence is hurting you or your
family, ask your doctor, counselor, or religious leader for
suggestions about getting help.
Reaching a decision on how you want to treat your prostate
cancer is very personal - it is a blending of what is
important to you, what you value the most, what types of
treatment options are available to you, and what the
benefits and side effects are.
Along with talking to their health professionals and spouse
or partner, many men find it helpful to meet with others
and talk about treatment choices. For example, you might
want to meet with:
- Family. This includes your relatives and close friends
who care about you. Your family can support your
choice about treatment.
- Men who faced prostate cancer. There is a lot to learn
from other men who faced these same prostate cancer
treatment decisions. You may want to join a support
group or meet with others to talk about the choices
they made and what life is like now that treatment is
over. Remember that while your prostate cancer may be
similar to someone else's, your life and desires may be
very different.
- Others who can help you. You may have other people
in your life who can help. This may be a close friend,
neighbor, counselor, social worker, or religious leader
you like and trust.
You may find it helpful to ask the following questions:
Could you write down my exact type of prostate cancer?
May I have a copy of my pathology report?
If I wish to have another pathologist look at my prostate
biopsy, how do I get the slides?
What is the clinical stage and Gleason score of this cancer?
What treatment option do you recommend?
- Watchful waiting
- Surgery (What type, can the nerves be spared, and how
often do you do this procedure?)
- Radiation (What type do you use, and what can be
done to minimize side effects?)
- Other
What are the short- and long-term side effects of this
particular treatment?
What are my chances of:
- Becoming incontinent
- Becoming impotent
- Having other urine or bowel problems
What are the chances of the cancer coming back if I have
this treatment?
What is the expected survival rate?
"Prostate cancer gives you the opportunity to make
a deliberate, considered choice. In the majority of
cases, the disease is very slow growing and is never
a medical emergency.
With prostate cancer, you have ample time to
assess the situation, evaluate your particular
needs and resources, and devise the most sensible,
strategic plan of action.
Doctors can and should help you to understand
your medical situation, but only you can decide
what trade-offs you can tolerate, what level of risk
you find acceptable, and which potential sacrifices
you're willing to make."
- Dr. Peter Scardino,
Chairman of the Department of Urology, Memorial
Sloan Kettering Cancer Center
 Back to Top Back to Top
Resources
You can find out more from these free NCI services:
Cancer Information Service (CIS)
Toll-free ...................1-800-4-CANCER (1-800-422-6237)
TTY ............................1-800-332-8615
NCI Online ................www.cancer.gov
Chat Online ..............www.cancer.gov/cis
Clinical Trials ...........www.cancer.gov/clinicaltrials/search
Free booklets that are available include:
Medicare
For more information about Medicare benefits, contact:
Toll-free ...................1-800-MEDICARE (1-800-633-4227)
Online ......................www.medicare.gov
National Kidney and Urologic Diseases
Information Clearinghouse
Toll-free ...................1-800-891-5390
Online ......................www.kidney.niddk.nih.gov
American Cancer Society Man-to-Man Program
This support group of the American Cancer Society offers
advice on coping with illness and the side effects of
treatment, along with newsletter archives and a directory of
prostate cancer publications. Call toll-free 1-800-ACS-2345
(1-800-227-2345) or visit online at www.cancer.org.
American Urological Association Foundation
The AUA Foundation supports research; provides education
to patients, the general public, and health professionals; and
offers patient support services for those who have or may be
at risk for a urologic disease or disorder. The Foundation
provides information on urologic diseases and dysfunctions,
including prostate cancer treatment options, bladder health,
and sexual function. It also offers prostate cancer support
groups (Prostate Cancer Network). Some Spanish language
publications are available. Call toll-free 1-800-828-7866 or
visit online at www.afud.org.
CancerCare
CancerCare is a national nonprofit agency that offers free
support, information, financial assistance, and practical
help to people with cancer and their loved ones. Services
are provided by oncology (cancer) social workers and are
available in person, over the telephone, and through the
agency's Web site. A section of the CancerCare Web site and
some publications are available in Spanish, and staff can
respond to calls and e-mail in Spanish. Call toll-free
1-800-813-HOPE (1-800-813-4673) or visit online at
www.cancercare.org.
Fertile Hope
Fertile Hope is a national organization that provides
reproductive information, support, and hope to cancer
patients whose medical treatments present the risk of
infertility. The organization offers fertility preservation
financial assistance options for patients. Call toll-free
1-888-994-HOPE (1-888-994-4673) or visit online at
www.fertilehope.org.
Prostate Cancer Foundation
The Prostate Cancer Foundation is a nonprofit
organization that provides funding for research projects to
improve methods of diagnosing and treating prostate
cancer. It also offers printed resources for prostate cancer
survivors and their families. The mission of the Prostate
Cancer Foundation is to find better treatments and a cure
for prostate cancer. Call toll-free 1-800-757-CURE
(1-800-757-2873) or visit online at
www.prostatecancerfoundation.org.
Us TOO International
Us TOO International Prostate Cancer Education and
Support Network is a non-profit education and support
group organization with more than 325 chapters
throughout the world. It provides men and their families
with fellowship, peer counseling, and timely, personalized,
unbiased, and reliable information about prostate cancer,
enabling informed choices about detection, treatment
options, and quality of life after treatment. Call toll-free
1-800-80-USTOO (1-800-808-7866) or visit online at
www.ustoo.org.
The Wellness Community
The Wellness Community gives free psychological and
emotional support to cancer patients and their families. It
offers support groups facilitated by licensed therapists,
stress reduction and cancer education workshops,
nutrition guidance, exercise sessions, and social events.
Call toll-free 1-888-793-WELL (1-888-793-9355) or visit
online at www.thewellnesscommunity.org.
 Back to Top Back to Top
|