

In a development that is literally lifesaving, Dr. Staudt, who has been on the staff of NCI for nearly 20 years, has successfully used genomic technology to reliably distinguish Burkitt’s lymphoma from Diffuse Large B-Cell Lymphomas (DLBCL).
The Lymphoma/Leukemia Molecular Profiling Project (LLMPP) is a network of 11 clinical groups that maintain biospecimens and clinical data from hundreds of patients with this cancer of the lymphatic system. An international consortium of investigators, including NCI-funded investigators and researchers around the world, the LLMPP is classifying lymphoma by distinct molecular characteristics and is then using that information to more accurately guide diagnosis and to target treatment.
Louis M. Staudt, M.D., Ph.D., studies lymphoma, a cancer of the lymphatic system that affects 23,000 patients yearly and causes 10,000 deaths Treatment can be dfficult, because this cancer has many subtypes, which require different treatment options. For example, Burkitt's lymphoma and diffuse large-B-cell lymphoma (DLBCL) are difficult to diagnose because the two cancers appear very similar under a microscope. However, the two are genetically distinct, and thus require very different treatments.
And the stakes couldn't be higher. "If Burkitt's patients are treated with intensive therapy, there is roughly an 80 percent survival rate," says Dr. Staudt, deputy chief of the Metabolism Branch and head of the Molecular Biology of Lymphoid Malignancies Section in NCI's Center for Cancer Research. "However, if they are misdiagnosed and treated with the lower intensity chemotherapy recommended for DLBCL, the survival rate is 20 percent or even less."
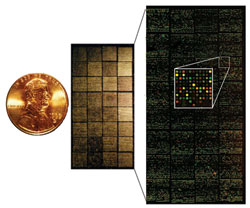
In a development that is literally life-saving, Dr. Staudt, who has been on the staff of NCI for nearly 20 years, has successfully used genomic technology to reliably distinguish Burkitt's lymphoma from DLBCL. Dr. Staudt demonstrated that DNA microarrays, a technology rooted in the Human Genome Project, can accurately distinguish Burkitt's lymphoma from DLBCL, thereby optimizing the treatment choice for each patient. "The current goal with the improved diagnostics technology is to make it uniform, reproducible, and available as a cost-effective test," notes Dr. Staudt.
In collaboration with a private sector company, researchers are now enrolling 2,000 to 4,000 patients for a large study of a new test designed to distinguish between all types of lymphomas and other, benign conditions.
Even as work continues on better diagnostics, Dr. Staudt points out that improved lymphoma treatments are also being discovered. Dr. Wyndham Wilson, a clinician at the NIH Clinical Center, has developed a novel, less toxic form of chemotherapy to treat Burkitt's lymphoma, called dose-adjusted EPOCH-R. In this treatment, the dosage of chemotherapeutic drugs is increased with every cycle until a maximum tolerated dosage is reached. "It's an empirical way of adjusting the dosage to fit each patient, which avoids both under treatment and over treatment," says Dr. Staudt. "This approach adjusts for differences in metabolism, age and genetics that can influence a patient's response to drugs."

NCI's Glioma Molecular Diagnostic Initiative (GMDI) aims to develop a comprehensive molecular classification system for this type of brain cancer, thus allowing consistent prediction of response to therapies for individual patients. The largest study ever conducted to merge genetic and clinical information, GMDI is a nationwide partnership of several NIH Institutes and NCI-funded consortia and scientists. GMDI investigators are conducting retrospective studies, which look backward to examine exposures to suspected risk, and prospective studies, which watch for outcomes over a long period of time, to build and validate molecular and genetic models of glioma. The molecular, genetic, and clinical data from GMDI are being compiled in REMBRANDT (REpository for Molecular BRAin Neoplasia DaTa), a publicly accessible online database and universal classification system.
Dr. Howard Fine "sees as many patients as want to see me." As the Chief of NCI's Neuro-Oncology Branch, he evaluates between 2,000 and 3,000 brain tumor patients a year. Brain cancer, he says, "is a disease that impacts patients physically, while eroding their cognition and personality, exacting a devastating toll on both the patient and caretaking families." Unfortunately, as Dr. Fine points out, "the current standard of care is not optimal." The disease is not amenable to prevention or early diagnosis, and care for brain cancer patients falls between the expertise of neurology and medical and surgical oncology. Dr. Fine is committed to changing that situation.
Gliomas are the most common tumors that originate in the brain, beginning in the cells that surround and support nerve cells. Patients with low-grade glioma, which tends to grow more slowly, have a survival rate that averages 5 to 10 years, while patients with high-grade, or aggressive, glioma (glioblastoma being most common) have a 14-month survival rate. The standard treatment for glioblastoma is surgery, radiation, and chemotherapy. Dr. Fine explains that glioblastomas are "hugely different" from patient to patient, which makes the case for a better understanding of the underlying genetic abnormalities that distinguish one type from another. Although several key genes have been shown to play a role in glioblastoma, and drugs that inhibit these targets have been developed, many other genes remain to be identified.
Dr. Fine envisioned an integrated program to study large numbers of glioma patients—comprised of 20 NCI-designated Cancer Centers, the pharmaceutical industry, brain tumor consortia, clinical trial cooperative groups, and other NIH Institutes. His concept, the Glioma Molecular Diagnostic Initiative, or GMDI, collects and correlates standardized data from tumor specimens that can be analyzed to identify patient genetic profiles and novel molecular targets—and to help develop patient-tailored therapy. For Dr. Fine, efforts such as this "represent a flagship initiative that brings together divergent programs in a war that couldn't be won otherwise."