Kidney Stones in Adults
On this page:
Kidney stones, one of the most painful of the urologic disorders, have beset humans for centuries. Scientists have found evidence of kidney stones in a 7,000-year-old Egyptian mummy. Unfortunately, kidney stones are one of the most common disorders of the urinary tract. Each year, people make almost 3 million visits to health care providers and more than half a million people go to emergency rooms for kidney stone problems.
Most kidney stones pass out of the body without any intervention by a physician. Stones that cause lasting symptoms or other complications may be treated by various techniques, most of which do not involve major surgery. Also, research advances have led to a better understanding of the many factors that promote stone formation and thus better treatments for preventing stones.
[Top]
Introduction to the Urinary Tract
The urinary tract, or system, consists of the kidneys, ureters, bladder, and urethra. The kidneys are two bean-shaped organs located below the ribs toward the middle of the back, one on each side of the spine. The kidneys remove extra water and wastes from the blood, producing urine. They also keep a stable balance of salts and other substances in the blood. The kidneys produce hormones that help build strong bones and form red blood cells.
The urinary tract.
Narrow tubes called ureters carry urine from the kidneys to the bladder, an oval-shaped chamber in the lower abdomen. Like a balloon, the bladder’s elastic walls stretch and expand to store urine. They flatten together when urine is emptied through the urethra to outside the body.
[Top]
What is a kidney stone?
A kidney stone is a hard mass developed from crystals that separate from the urine within the urinary tract. Normally, urine contains chemicals that prevent or inhibit the crystals from forming. These inhibitors do not seem to work for everyone, however, so some people form stones. If the crystals remain tiny enough, they will travel through the urinary tract and pass out of the body in the urine without being noticed.
Kidney stones may contain various combinations of chemicals. The most common type of stone contains calcium in combination with either oxalate or phosphate. These chemicals are part of a person’s normal diet and make up important parts of the body, such as bones and muscles.
A less common type of stone is caused by infection in the urinary tract. This type of stone is called a struvite or infection stone. Another type of stone, uric acid stones, are a bit less common, and cystine stones are rare.

Kidney stones in the kidney, ureter, and bladder.
Urolithiasis is the medical term used to describe stones occurring in the urinary tract. Other frequently used terms are urinary tract stone disease and nephrolithiasis. Doctors also use terms that describe the location of the stone in the urinary tract. For example, a ureteral stone—or ureterolithiasis—is a kidney stone found in the ureter. To keep things simple, the general term kidney stones is used throughout this fact sheet.
Gallstones and kidney stones are not related. They form in different areas of the body. Someone with a gallstone is not necessarily more likely to develop kidney stones.
[Top]
Who gets kidney stones?
For unknown reasons, the number of people in the United States with kidney stones has been increasing over the past 30 years. In the late 1970s, less than 4 percent of the population had stone-forming disease. By the early 1990s, the portion of the population with the disease had increased to more than 5 percent. Caucasians are more prone to develop kidney stones than African Americans. Stones occur more frequently in men. The prevalence of kidney stones rises dramatically as men enter their 40s and continues to rise into their 70s. For women, the prevalence of kidney stones peaks in their 50s. Once a person gets more than one stone, other stones are likely to develop.
[Top]
What causes kidney stones?
Doctors do not always know what causes a stone to form. While certain foods may promote stone formation in people who are susceptible, scientists do not believe that eating any specific food causes stones to form in people who are not susceptible.
A person with a family history of kidney stones may be more likely to develop stones. Urinary tract infections, kidney disorders such as cystic kidney diseases, and certain metabolic disorders such as hyperparathyroidism are also linked to stone formation.
In addition, more than 70 percent of people with a rare hereditary disease called renal tubular acidosis develop kidney stones.
Shapes of various stones. Sizes are usually smaller than shown here.
Cystinuria and hyperoxaluria are two other rare, inherited metabolic disorders that often cause kidney stones. In cystinuria, too much of the amino acid cystine, which does not dissolve in urine, is voided, leading to the formation of stones made of cystine. In patients with hyperoxaluria, the body produces too much oxalate, a salt. When the urine contains more oxalate than can be dissolved, the crystals settle out and form stones.
Hypercalciuria is inherited, and it may be the cause of stones in more than half of patients. Calcium is absorbed from food in excess and is lost into the urine. This high level of calcium in the urine causes crystals of calcium oxalate or calcium phosphate to form in the kidneys or elsewhere in the urinary tract.
Other causes of kidney stones are hyperuricosuria, which is a disorder of uric acid metabolism; gout; excess intake of vitamin D; urinary tract infections; and blockage of the urinary tract. Certain diuretics, commonly called water pills, and calcium-based antacids may increase the risk of forming kidney stones by increasing the amount of calcium in the urine.
Calcium oxalate stones may also form in people who have chronic inflammation of the bowel or who have had an intestinal bypass operation, or ostomy surgery. As mentioned earlier, struvite stones can form in people who have had a urinary tract infection. People who take the protease inhibitor indinavir, a medicine used to treat HIV infection, may also be at increased risk of developing kidney stones.
[Top]
Foods and Drinks Containing Oxalate
People prone to forming calcium oxalate stones may be asked by their doctor to limit or avoid certain foods if their urine contains an excess of oxalate.
High-oxalate foods—higher to lower
- rhubarb
- spinach
- beets
- swiss chard
- wheat germ
- soybean crackers
- peanuts
- okra
- chocolate
- black Indian tea
- sweet potatoes
Foods that have medium amounts of oxalate may be eaten in limited amounts.
Medium-oxalate foods—higher to lower
- grits
- grapes
- celery
- green pepper
- red raspberries
- fruit cake
- strawberries
- marmalade
- liver
Source: The Oxalosis and Hyperoxaluria Foundation.
[Top]
What are the symptoms of kidney stones?
Kidney stones often do not cause any symptoms. Usually, the first symptom of a kidney stone is extreme pain, which begins suddenly when a stone moves in the urinary tract and blocks the flow of urine. Typically, a person feels a sharp, cramping pain in the back and side in the area of the kidney or in the lower abdomen. Sometimes nausea and vomiting occur. Later, pain may spread to the groin.
If the stone is too large to pass easily, pain continues as the muscles in the wall of the narrow ureter try to squeeze the stone into the bladder. As the stone moves and the body tries to push it out, blood may appear in the urine, making the urine pink. As the stone moves down the ureter, closer to the bladder, a person may feel the need to urinate more often or feel a burning sensation during urination.
If fever and chills accompany any of these symptoms, an infection may be present. In this case, a person should contact a doctor immediately.
[Top]
How are kidney stones diagnosed?
Sometimes “silent” stones—those that do not cause symptoms—are found on x rays taken during a general health exam. If the stones are small, they will often pass out of the body unnoticed. Often, kidney stones are found on an x ray or ultrasound taken of someone who complains of blood in the urine or sudden pain. These diagnostic images give the doctor valuable information about the stone’s size and location. Blood and urine tests help detect any abnormal substance that might promote stone formation.
The doctor may decide to scan the urinary system using a special test called a computerized tomography (CT) scan or an intravenous pyelogram (IVP). The results of all these tests help determine the proper treatment.
[Top]
Preventing Kidney Stones
A person who has had more than one kidney stone may be likely to form another; so, if possible, prevention is important. To help determine their cause, the doctor will order laboratory tests, including urine and blood tests. The doctor will also ask about the patient’s medical history, occupation, and eating habits. If a stone has been removed, or if the patient has passed a stone and saved it, a stone analysis by the laboratory may help the doctor in planning treatment.
The doctor may ask the patient to collect urine for 24 hours after a stone has passed or been removed. For a 24-hour urine collection, the patient is given a large container, which is to be refrigerated between trips to the bathroom. The collection is used to measure urine volume and levels of acidity, calcium, sodium, uric acid, oxalate, citrate, and creatinine—a product of muscle metabolism. The doctor will use this information to determine the cause of the stone. A second 24-hour urine collection may be needed to determine whether the prescribed treatment is working.
[Top]
How are kidney stones treated?
Fortunately, surgery is not usually necessary. Most kidney stones can pass through the urinary system with plenty of water—2 to 3 quarts a day—to help move the stone along. Often, the patient can stay home during this process, drinking fluids and taking pain medication as needed. The doctor usually asks the patient to save the passed stone(s) for testing. It can be caught in a cup or tea strainer used only for this purpose.
Lifestyle Changes
A simple and most important lifestyle change to prevent stones is to drink more liquids—water is best. Someone who tends to form stones should try to drink enough liquids throughout the day to produce at least 2 quarts of urine in every 24-hour period.
In the past, people who form calcium stones were told to avoid dairy products and other foods with high calcium content. Recent studies have shown that foods high in calcium, including dairy products, may help prevent calcium stones. Taking calcium in pill form, however, may increase the risk of developing stones.
Patients may be told to avoid food with added vitamin D and certain types of antacids that have a calcium base. Someone who has highly acidic urine may need to eat less meat, fish, and poultry. These foods increase the amount of acid in the urine.
To prevent cystine stones, a person should drink enough water each day to dilute the concentration of cystine that escapes into the urine, which may be difficult. More than a gallon of water may be needed every 24 hours, and a third of that must be drunk during the night.
Medical Therapy
A doctor may prescribe certain medications to help prevent calcium and uric acid stones. These medicines control the amount of acid or alkali in the urine, key factors in crystal formation. The medicine allopurinol may also be useful in some cases of hyperuricosuria.
Doctors usually try to control hypercalciuria, and thus prevent calcium stones, by prescribing certain diuretics, such as hydrochlorothiazide. These medicines decrease the amount of calcium released by the kidneys into the urine by favoring calcium retention in bone. They work best when sodium intake is low.
Rarely, patients with hypercalciuria are given the medicine sodium cellulose phosphate,
which binds calcium in the intestines and prevents it from leaking into the urine.
If cystine stones cannot be controlled by drinking more fluids, a doctor may prescribe medicines such as Thiola and Cuprimine, which help reduce the amount of cystine in the urine.
For struvite stones that have been totally removed, the first line of prevention is to keep the urine free of bacteria that can cause infection. A patient’s urine will be tested regularly to ensure no bacteria are present.
If struvite stones cannot be removed, a doctor may prescribe a medicine called acetohydroxamic
acid (AHA). AHA is used with long-term antibiotic medicines to prevent the infection that leads to stone growth.
People with hyperparathyroidism sometimes develop calcium stones. Treatment in these cases is usually surgery to remove the parathyroid glands, which are located in the neck. In most cases, only one of the glands is enlarged. Removing the glands cures the patient’s problem with hyperparathyroidism and kidney stones.
Surgical Treatment
Surgery may be needed to remove a kidney stone if it
- does not pass after a reasonable period of time and causes constant pain
- is too large to pass on its own or is caught in a difficult place
- blocks the flow of urine
- causes an ongoing urinary tract infection
- damages kidney tissue or causes constant bleeding
- has grown larger, as seen on follow-up x rays
Until 20 years ago, open surgery was necessary to remove a stone. The surgery required a recovery time of 4 to 6 weeks. Today, treatment for these stones is greatly improved, and many options do not require major open surgery and can be performed in an outpatient setting.
Extracorporeal Shock Wave Lithotripsy
Extracorporeal shock wave lithotripsy (ESWL) is the most frequently used procedure for the treatment of kidney stones. In ESWL, shock waves that are created outside the body travel through the skin and body tissues until they hit the denser stones. The stones break down into small particles and are easily passed through the urinary tract in the urine.
Several types of ESWL devices exist. Most devices use either x rays or ultrasound to help the surgeon pinpoint the stone during treatment. For most types of ESWL procedures, anesthesia is needed.
In many cases, ESWL may be done on an outpatient basis. Recovery time is relatively short, and most people can resume normal activities in a few days.
Complications may occur with ESWL. Some patients have blood in their urine for a few days after treatment. Bruising and minor discomfort in the back or abdomen from the shock waves can occur. To reduce the risk of complications, doctors usually tell patients to avoid taking aspirin and other medicines that affect blood clotting for several weeks before treatment.
Sometimes, the shattered stone particles cause minor blockage as they pass through the urinary tract and cause discomfort. In some cases, the doctor will insert a small tube called a stent through the bladder into the ureter to help the fragments pass. Sometimes the stone is not completely shattered with one treatment, and additional treatments may be needed.
As with any interventional, surgical procedure, potential risks and complications should be discussed with the doctor before making a treatment decision.
Extracorporeal shock wave lithotripsy.
Percutaneous Nephrolithotomy
Sometimes a procedure called percutaneous nephrolithotomy is recommended to remove a stone. This treatment is often used when the stone is quite large or in a location that does not allow effective use of ESWL.
In this procedure, the surgeon makes a tiny incision in the back and creates a tunnel directly into the kidney. Using an instrument called a nephroscope, the surgeon locates and removes the stone. For large stones, some type of energy probe—ultrasonic or electrohydraulic—may be needed to break the stone into small pieces. Often, patients stay in the hospital for several days and may have a small tube called a nephrostomy tube left in the kidney during the healing process.
One advantage of percutaneous nephrolithotomy is that the surgeon can remove some of the stone fragments directly instead of relying solely on their natural passage from the kidney.
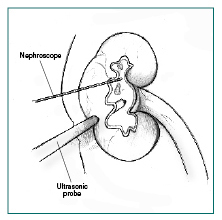
Percutaneous nephrolithotomy.
Ureteroscopic Stone Removal
Although some stones in the ureters can be treated with ESWL, ureteroscopy may be needed for mid- and lower-ureter stones. No incision is made in this procedure. Instead, the surgeon passes a small fiberoptic instrument called a ureteroscope through the urethra and bladder into the ureter. The surgeon then locates the stone and either removes it with a cage-like device or shatters it with a special instrument
that produces a form of shock wave. A small tube or stent may be left in the ureter for a few days to help urine flow. Before fiber optics made ureteroscopy possible, physicians used a similar “blind basket” extraction method. But this technique is rarely used now because of the higher risks of damage to the ureters.
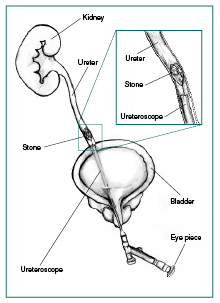
Ureteroscopic stone removal.
[Top]
Hope through Research
The Division of Kidney, Urologic, and Hematologic Diseases of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) funds research on the causes, treatments, and prevention of kidney stones. The NIDDK is part of the National Institutes of Health in Bethesda, MD.
New medicines and the growing field of lithotripsy have greatly improved the treatment of kidney stones. Still, NIDDK researchers and grantees seek to answer questions such as
- Why do some people continue to have painful stones?
- How can doctors predict, or screen, those at risk for getting stones?
- What are the long-term effects of lithotripsy?
- Do genes play a role in stone formation?
- What is the natural substance(s) found in urine that blocks stone formation?
Researchers are also developing new medicines with fewer side effects.
[Top]
Points to Remember
- A person with a family history of stones or a personal history of more than one stone may be more likely to develop more stones.
- A good first step to prevent the formation of any type of stone is to drink plenty of liquids—water is best.
- Someone who is at risk for developing stones may need certain blood and urine tests to determine which factors can best be altered to reduce that risk.
- Some people will need medicines to prevent stones from forming.
- People with chronic urinary tract infections and stones will often need a stone removed if the doctor determines that the stone is causing the infection. Patients must receive careful follow-up to be sure that the infection has cleared.
The U.S. Government does not endorse or favor any specific commercial product or company. Trade, proprietary, or company names appearing in this document are used only because they are considered necessary in the context of the information provided. If a product is not mentioned, the omission does not mean or imply that the product is unsatisfactory.
[Top]
For More Information
American Urological Association Foundation
1000 Corporate Boulevard
Linthicum, MD 21090
Phone: 1–866–RING–AUA (746–4282) or 410–689–3700
Email: patienteducation@auafoundation.org
Internet: www.auafoundation.org
www.UrologyHealth.org
National Kidney Foundation
30 East 33rd Street
New York, NY 10016
Phone: 1–800–622–9010 or 212–889–2210
Internet: www.kidney.org
Oxalosis and Hyperoxaluria Foundation
201 East 19th Street, Suite 12E
New York, NY 10003
Phone: 1–800–OHF–8699 (643–8699) or 212–777–0470
Fax: 212–777–0471
Email: execdirector@ohf.org
Internet: www.ohf.org
For Information About Hyperparathyroidism:
National Endocrine and Metabolic Diseases Information Service
National Institute of Diabetes and Digestive and Kidney Diseases
National Institutes of Health
6 Information Way
Bethesda, MD 20892–3569
Phone: 1–888–828–0904
Fax: 703–738–4929
Email: endoandmeta@info.niddk.nih.gov
For Information About Gout:
National Institute of Arthritis and Musculoskeletal and Skin Diseases Information Clearinghouse
National Institutes of Health
1 AMS Circle
Bethesda, MD 20892–3675
Phone: 1–877–22–NIAMS (226–4267) or 301–495–4484
TTY: 301–565–2966
Fax: 301–718–6366
Email: niamsinfo@mail.nih.gov
Internet: www.niams.nih.gov
The National Kidney and Urologic Diseases Information Clearinghouse collects resource information about kidney and urologic diseases for the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Reference Collection. This database provides titles, abstracts, and availability information for health information and health education resources. The NIDDK Reference Collection is a service of the National Institutes of Health.
You may view the results of the automatic search on kidney stones.
If you wish to perform your own search of the database, you may access and search the NIDDK Reference Collection database online.
This publication may contain information about medications used to treat a health condition. When this publication was prepared, the NIDDK included the most current information available. Occasionally,
new information about medication is released. For updates or for questions about any medications, please contact the U.S. Food and Drug Administration at 1–888–INFO–FDA (463–6332 ), a toll-free call, or visit their website at www.fda.gov. Consult your doctor for more information.
[Top]
National Kidney and Urologic Diseases Information Clearinghouse
3 Information Way
Bethesda, MD 20892–3580
Phone: 1–800–891–5390
TTY: 1–866–569–1162
Fax: 703–738–4929
Email: nkudic@info.niddk.nih.gov
Internet: www.kidney.niddk.nih.gov
The National Kidney and Urologic Diseases Information Clearinghouse (NKUDIC) is a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The NIDDK is part of the National Institutes of Health of the U.S. Department of Health and Human Services. Established in 1987, the Clearinghouse provides information about diseases of the kidneys and urologic system to people with kidney and urologic disorders and to their families, health care professionals, and the public. The NKUDIC answers inquiries, develops and distributes publications, and works closely with professional and patient organizations and Government agencies to coordinate resources about kidney and urologic diseases.
Publications produced by the Clearinghouse are carefully reviewed by both NIDDK scientists and outside experts. This publication was reviewed by Frederic L. Coe., M.D., University of Chicago.
This publication is not copyrighted. The Clearinghouse encourages users of this publication to duplicate and distribute as many copies as desired.
NIH Publication No. 08–2495
October 2007
[Top]
|