Breast cancer is the second
most common form of cancer
and the second leading cause
of cancer deaths for
American women. Each year,
more than 210,000 women in
the United States learn that
they have breast cancer.
Some kinds of cancer, such as breast and ovarian cancer, seem to run
in families. There is a test that may tell some people if they are at
risk for breast, ovarian, and other cancers. Before getting tested,
though, there are many factors you should consider.
This booklet will give you an overview of testing for breast and
ovarian cancer risk. This information may also apply to risk of other
cancers. It describes the advantages and disadvantages of this kind of
testing. It also gives basic medical terms to help as you talk with
your doctor or other health care professionals trained in genetics.
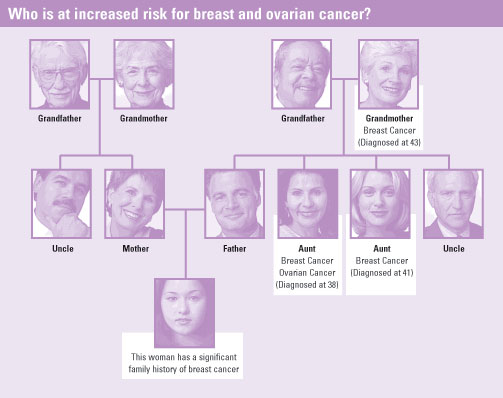
A woman with a significant family history
of breast and/or ovarian cancer has a higher risk
of getting these cancers. You have a significant
family history if:
- You have two or more close family members
who have had breast and/or ovarian cancer,
and/or
- The breast cancer in the family members has
been found before the age of 50.
Talk with your doctor or other health care
professional trained in genetics about your
family history. He or she can help you know if
you have a significant family history of breast
and/or ovarian cancer. This information may
help you learn about your cancer risk and help
you decide if genetic testing is right for you.
| A Note About Family History |
|
A close family member can be your:
- Mother
- Father
- Sister
- Brother
- Grandparent (on your mother's or
father's side)
- Mother's sister and/or brother
- Father's sister and/or brother
Having a family history of cancer does not
mean you are going to get cancer. Many
things, such as family history and age, may
increase a person's chance (or risk) of getting
cancer. But family history alone is not the only
reason people get cancer. Scientists do not
know all the reasons why people get cancer.
|
Genes are nature's blueprints for
every living thing. Most genes come
in pairs: one set of genes is passed
down (or inherited) from your mother
and the other set from your father.
Genes determine how your body will
function and grow, as well as the
color of your hair and eyes.
Sometimes genes do not function properly because there is a
mistake in them. If a gene has a mistake, it is said to be
mutated or altered. When a gene with a mistake is passed
along in family members, it is called an inherited altered
gene. All people have altered forms of some genes. Certain
altered genes can increase your risk of illnesses such as cancer.
Gene alterations have been found in many families with a
history of breast cancer. Some women in these families have
also had ovarian cancer.
These alterations are most often found in genes named BRCA1
and BRCA2 (BReast CAncer Gene 1 and BReast CAncer Gene
2). Both men and women have BRCA1 and BRCA2 genes, so alterations in these genes can be passed
down from either the mother or the father. More genes like these may be discovered in the future.
A woman with a BRCA1 or BRCA2 alteration is at higher risk for developing breast, ovarian, and other
cancers than a woman without an alteration. However, not every woman who has an altered BRCA1 or
BRCA2 gene will get cancer, because genes are not the only factor that affects cancer risk.
Most cases of breast cancer do not involve altered genes that are inherited. At most, about 1 in 10 breast
cancer cases can be explained by inherited alterations in BRCA1 and 2 genes.
Although breast cancer in men is rare, men with altered BRCA1 and BRCA2 genes have higher rates of
breast cancer than men without an altered gene. Men with an altered BRCA1 or 2 gene may also have a
slightly higher risk of other cancers. Even if a man never develops cancer, he can pass the altered gene to
his sons and daughters.
Genetic testing is a process that looks for inherited genetic alterations that may increase your risk of certain
cancers. This type of testing may show whether the risk in a family is passed through their genes.
Although the lab test itself is quite complex, only a blood sample is needed. For breast and ovarian cancer
risk, the testing involves looking for altered genes such as BRCA1 and BRCA2. Finding an altered gene can
take several weeks. So your test results may not be ready right away.
The price of testing varies and, in some cases, may not be covered by health insurance. Ask your doctor or
other health professionals for more information on genetic testing, privacy issues, and insurance coverage.
- The limits of the test
- The advantages and disadvantages of the test
- Would knowing this information cause me to make changes in my medical care?
Testing for breast and ovarian cancer risk will not
give you a simple "yes" or "no" answer. If a gene
alteration is found, this will tell that you have an
increased risk of getting cancer, but it will not tell
if or when cancer will develop. If an alteration is
not found, it still is no guarantee that cancer
won't develop.
Genetic testing can affect relationships with family
members. Think about who in your family might
want to know your test results, and who you'd like
to tell.
If you are thinking about being tested, you should
decide what the advantages and disadvantages of
testing are for you. What is right for one person is
not always right for another.
If you are thinking about genetic testing, you should
be informed, both verbally and in writing, about the
risks of getting tested, as well as what the test can
and cannot tell you. You can decide if testing is or
is not right for you. You may also choose to delay
the decision, if this is not the best time for you to
be tested.
| Advantages and Disadvantages |
|
Having a genetic test may help you to:
- Make medical and lifestyle choices
- Clarify your cancer risk
- Decide whether or not to have risk-reducing
surgery (see below)
- Give other family members useful
information (if you choose to share
your results)
- May explain why you or other family
members have developed cancer
The disadvantages to testing:
- There is no guarantee that your test
results will remain private
- Although rare, you may face
discrimination for health, life,
disability, and other insurance
- You may find it harder to cope with
your cancer risk when you know your
test results
- If you find that you do not have an
inherited altered gene, you may think that
you have no chance of getting cancer.
People who are found not to have an
inherited cancer gene can still get cancer.
|
You can make choices that help lower your risk of getting cancer or help find cancer early. You do not need
to be tested to consider these options.
- Increased monitoring. You may choose to be watched more closely for any sign of cancer.
This can include more frequent breast and pelvic exams, mammograms, breast MRI, breast self-exams,
ultrasound of the ovaries and breasts, and blood tests.
- Risk-reducing surgery. Called prophylactic (PROH-fuh-LAK-tik) surgery, this is when women
choose to have healthy ovaries and/or breasts removed to reduce their chance of getting cancer. You
may want to talk with your doctor and other health care professionals to learn more about this.
A person who is considering genetic testing should talk with a professional trained in genetics before
deciding whether to be tested. For more information on genetic testing or for a referral to centers that have
health care professionals trained in genetics, call the National Cancer Institute's Cancer Information Service
toll-free at 1-800-4-CANCER (1-800-422-6237), or visit online at www.cancer.gov. The Cancer Information
Service can also provide information about clinical trials, other research studies, and current risk
management information.
| What are the main questions I should ask? |
|
If you are thinking about genetic testing, be sure to talk with your doctor, nurse, genetic
counselor, or other health professionals, and take some time to answer these questions
together. You may want to get more than one opinion.
- What are the chances that an inherited gene alteration is
involved in the cancer in me or
my family?
- What are my chances of having an inherited altered gene?
- Besides having altered genes, what are my other risk factors
for breast and ovarian cancer?
- Are all genetic tests the same? How much does the test cost?
How long will it take to get
my results?
- What are the possible results of the test?
- What would a positive result mean for me?
- What would a negative result mean for me?
- How might a positive test result affect my health, life, and disability insurance options?
- How might a positive test result affect my employment?
- Do I want to ask my insurance company to pay for my test?
- Where will my test results be placed/recorded? Who will have access to them?
- Would knowing this information cause me to make changes in my medical care?
- What are my reasons for wanting to be tested?
- What type of cancer screening is recommended if I don't get tested?
Other questions to think about and discuss with your family:
- What effect will the test results have on me and my relationship with my family members if
I have an inherited altered gene? If I don't have an altered gene?
- Should I share my test results with my spouse or partner? Parents? Children? Friends?
Others? How will they react to the news, which may also affect them?
- Are my children ready to learn new information that may one day affect their own health?
|
Back to Top |