Placebos: Sugar, Shams, Therapies, or All of the Above?

Ted Kaptchuk
Ever since NCCAM cosponsored a conference in 2000 on placebos and placebo responses, the Center has funded research to advance knowledge in this area. Members of NCCAM's National Advisory Council for Complementary and Alternative Medicine (NACCAM) heard new developments in placebo research when two NCCAM-supported investigators spoke at the Council's meeting in June 2007. The sessions were open to the public.
What Are Placebos and Their Effects?
Catherine Stoney, Ph.D., NCCAM program officer, served as moderator of the scientific symposium. A placebo response, she said, is one or more beneficial physical or psychological changes that occurs in response to a placebo--which can be defined in various ways as:
- An inactive substance (for example, a sugar pill) designed to look like an active medication
- A "sham" procedure or device, such as a procedure designed to look like acupuncture but not to deliver treatment effects
- A "therapeutic encounter or symbol," such as:
- An interaction with a health care provider
- Something symbolic in such an encounter (for example, the "white-coat effect" that some researchers have noted).
Placebos like inactive pills and sham procedures have a history of use in controlled experiments. They allow researchers to obtain a truer picture of the effects of the active treatment under study, above and beyond what might occur over time and due to the expectation of positive benefit. Placebos are also widely viewed as nuisances, however--producers of "noise" that complicate analysis of study data--because sometimes there are therapeutic responses to them.
Increasingly, scientists and clinicians have come to believe that the power of placebos, when harnessed, could potentially enhance health and health care. Studies of placebo effects could also provide insight into the mind's effects on the body and on practices in the CAM domain of mind-body medicine (such as meditation, hypnosis, and yoga). NCCAM is supporting a variety of studies that are looking at placebos and their effects:
- At many levels, ranging from molecules, cells, and organ systems; to thoughts, emotions, expectations, and interactions; and to social and economic factors
- In many ways, including how they operate in specific diseases and conditions and how they can be enhanced in clinical practice.
"People Get Well in Ways We Don't Understand"
Ted Kaptchuk is an associate professor of medicine at Harvard Medical School, associate director of the Division for Research and Education in Complementary and Integrative Medical Therapies at Harvard's Osher Institute, and a member of NCCAM's Advisory Council. He received his training in Asian medicine in China. Professor Kaptchuk recalled that when he was working as director of a chronic pain unit at a chronic disease facility in the United States, he saw some improvements that led him to think, "People get well sometimes in ways that we don't understand. Practitioners usually credit their therapies. Sometimes, it seemed to me that relief and healing had nothing to do with the specific therapy--indeed, that important processes were going on underneath the official therapy. That's why I became interested in studying the placebo effect."
Professor Kaptchuk describes the placebo response in randomized, controlled trials as a "box" of many complex elements that he and his colleagues are seeking to "unpack." In an illustration that he has developed (see figure), the last three bulleted items are the focus of his research.
He described a few of his studies, including one published in 2006 in which he and his colleagues compared the effects of a sham device and an inactive pill with each other and with real treatments. His team was interested primarily in the placebos' effects. The participants were 270 adults with persistent arm pain from repetitive use.
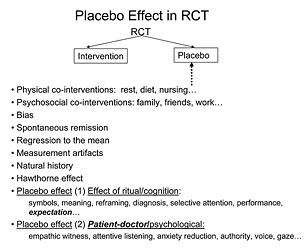
Components of the response to placebo treatment in randomized controlled trials.
© T.J. Kaptchuk, Used by permission
Each participant was randomized into a so-called acupuncture group or amitryptyline (a type of medication) group. During the first 2 weeks, or "run-in period," all participants received either the sham acupuncture treatment or the inactive pill. Next, half of each group received the active treatment and the other half received the corresponding sham or placebo. Participants did not know at any time whether they were receiving active treatment or a sham/placebo. The team then looked at various pain outcomes.
Among their findings:
- The sham acupuncture device worked better than the placebo pill (except during the run-in period) on the primary measure of pain and on the severity of symptoms.
- A pain-relieving placebo effect persisted over time--not just for a short time, which is a commonly held belief about placebos.
- Placebo effects may relate to the expectations of participants and the information provided to them. As part of the standard informed-consent process, all participants had been told before the study started about possible side effects they might experience if they received an active treatment. Each group was told to expect different side effects. Interestingly, many participants who received only the sham device (about one-quarter) or inactive pill (about one-third) reported they experienced the side effects of the corresponding active treatment. This, said Professor Kaptchuk, also illustrates a strong "nocebo effect"--the flip side of the placebo effect. A person experiences negative, not positive, physical and psychological effects in response to a nocebo.
Professor Kaptchuk described a second study that also worked with participants' expectations about pain relief from an actual acupuncture treatment and that used a sham device. This controlled study used fMRI brain imaging to study participants' brain responses, literally shedding light on multiple pathways and mechanisms of the brain that may play an important role in placebo pain-relief effects. Another study, now being submitted for publication, examines various proposed components of the placebo effect both separately and together.
CAM at the NIH asked Professor Kaptchuk about his future study plans. In addition to further examining the underlying biological mechanisms of placebo effects, he hopes to investigate such issues as whether a "placebo responder" exists; whether placebo effects can be administered in a dose-dependent manner; and whether behavioral methods can amplify and harness the placebo effect in clinical practice and dampen and reduce it in clinical trials.
"There Are Perfections in the Brain That Need To Be Exploited"
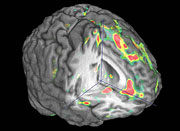
PET scan of the brain regions--anterior cingulate, dorsolateral prefrontal cortex, anterior insula, and nucleus accumbens--in which the endogenous opioid system and mu-opioid receptors were activated during placebo administration.
© J.K. Zubieta, Used by permission
The second speaker, Jon-Kar Zubieta, M.D., Ph.D., is a professor of psychiatry, radiology, and neurosciences at the University of Michigan Medical School and at the university's Molecular and Behavioral Neuroscience Institute. His training is in neuroimaging, nuclear medicine, and psychiatry.
Dr. Zubieta has been studying brain activity and responses to placebos in the context of pain and stress. He is interested in the operation of expectations and awareness in placebo effects and even more interested in resilience mechanisms--people's ability to mobilize a response, especially biologically, when they believe they are receiving or will receive a treatment that could be helpful. He and his team use positron-emission tomography, or PET (see image), to study the experiences of pain and pain relief (including from placebos) in the brain as they are occurring.
Dr. Zubieta highlighted some of his findings:
- He has seen an almost perfect match across people's responses to placebo treatment, between the release of substances called endogenous opioids (EOs) and lessened sensitivity to pain over time. Endogenous opioids are chemicals that occur naturally in the body and have characteristics similar to those of drugs like morphine.
- In "executive areas" of the brain (areas that integrate information, and also reduce pain through the release of EOs), there is "enormous individuality and variability" among study participants in terms of which regions are activated and how much.
- The brain chemical dopamine appears to be important in pain relief experienced from placebos. Dopamine and its pathways are known to be central in responses to reward and the prospect of reward. Dr. Zubieta thinks that they may also become activated by the prospect of pain relief, including from placebos. This, in turn, may drive systems like EOs that reduce both the pain experience and its unpleasantness.
- Cognitive influences such as thoughts and beliefs, emotions, gender, hormones, and genetics all appear to play a role in how people experience pain, stress, and the placebo response. For example, in preliminary work, Dr. Zubieta found gender differences in how much people's EOs respond to the administration of a placebo. He is trying to shed further light on this area by examining the influence of estrogen and progesterone.

Catherine Stoney and Jon-Kar Zubieta
When asked by an audience member, "Are there imperfections in the human brain that need to be remedied?" Dr. Zubieta answered, "There are perfections in the human brain that need to be exploited." Among other factors he hopes to study are individual variability in specific genes. "Then," he said, "our knowledge of the biology of the placebo effect can be examined in the context of disease states, including movement disorders, depression, and cardiovascular disease."
Selected References
Benedetti F, Mayberg HS, Wager TD, et al. Neurobiological mechanisms of the placebo effect. Journal of Neuroscience. 2005;25(45):10390-10402.
Guess HA, Kleinman A, Kusek JW, Engel L. The Science of the Placebo: Toward an Interdisciplinary Research Agenda. London: BMJ Publishing Group; 2002.
Kaptchuk TJ, Stason WB, Davis RB, et al. Sham device v inert pill: randomised controlled trial of two placebo treatments. BMJ. 2006;332(7538):391-397.
Kong J, Gollub RL, Rosman IS, et al. Brain activity associated with expectancy-enhanced placebo analgesia as measured by functional magnetic resonance imaging. Journal of Neuroscience. 2006;26(2):381-388.
Pickering TG, Gerin W, Schwartz AR. What is the white-coat effect and how should it be measured? Blood Pressure Monitoring. 2002;7(6):293-300.
Scott DJ, Stohler CS, Egnatuk CM, et al. Individual differences in reward responding explain placebo-induced expectations and effects. Neuron. 2007;55(2):325-326.
Wasan AD, Kaptchuk TJ, Davar G, et al. The association between psychopathology and placebo analgesia in patients with discogenic low back pain. Pain Medicine. 2006;7(3):217-228.
Zubieta JK, Yau WY, Scott DJ, et al. Belief or need? Accounting for individual variations in the neurochemistry of the placebo effect. Brain, Behavior, and Immunity. 2006;20(1):15-26.
