PUBLIC HEALTH PREPAREDNESS: MOBILIZING STATE BY STATE
Background

“When people ask me what’s the biggest challenge in public health, I
have an easy answer. For large-scale disasters and more routine threats
to health, the major problem we face in public health is complacency.
We’ve made a lot of progress in our preparedness efforts, but we’re
not done yet. We need long-term investment to really get us where we
want to be."
— Dr. Julie Gerberding, CDC Director -
Public health threats are inevitable. Being prepared can save lives and protect the health and safety of the public and emergency responders during disasters. A prepared public health system involves continual improvement of the system’s ability to prevent, protect against, respond to, and recover from the consequences of emergencies.
The Centers for Disease Control and Prevention (CDC) works to support public health preparedness for all hazards, including natural, biological, chemical, radiological, and nuclear events. This work falls under one of the agency’s overarching health protection goals: “People prepared for emerging health threats - people in all communities will be protected from infectious, occupational, environmental, and terrorist threats.” CDC has established nine preparedness goals to strategically direct resources towards achieving this overarching goal. These goals are associated with six public health preparedness activities: prevent, detect and report, investigate, control, recover, and improve (Table 1).
The events of September 11, 2001, and the subsequent anthrax attacks both highlighted the importance of public health during emergencies and showed weaknesses in public health’s ability to respond during a potential crisis. According to a 2002 Institute of Medicine report, the public health infrastructure suffered from “vulnerable and outdated health information systems and technologies, an insufficient and inadequately trained public health workforce, antiquated laboratory capacity, a lack of realtime surveillance and epidemiological systems, ineffective and fragmented communications networks, incomplete domestic preparedness and emergency response capabilities, and communities without access to essential public health services.
In 2002, Congress authorized funding for the Public Health Emergency Preparedness cooperative agreement (hereafter referred to as the cooperative agreement) to support preparedness nationwide in public health departments.2,3 Within each funded jurisdiction, public health departments at the state, local, tribal, and/or territorial levels work together to improve preparedness.
CDC administers the cooperative agreement and provides technical assistance to state, territorial, and major metropolitan public health departments. This technical assistance leverages CDC expertise in disease detection and investigation, public health laboratories, and response, including crisis communication. CDC’s longstanding working relationships with public health departments are critical to the success of this program.
Table 1: CDC Preparedness Goals
| Pre-Event | >Prevent | |
|---|---|---|
| Goal 1 | Increase the use and development of interventions known to prevent human illness from chemical, biological, radiological agents, and naturally occurring health threats. | |
| Event | Detect and Report | |
| Goal 2 | Decrease the time needed to classify health events as terrorism or naturally occurring in partnership with other agencies. | |
| Goal 3 | Decrease the time needed to detect and report chemical, biological, radiological agents in tissue, food or environmental samples that cause threats to the public’ health. | |
| Goal 4 | Improve the timeliness and accuracy of communications regarding threats to the public’s health. | |
| Investigate | ||
| Goal 5 | Decrease the time to identify causes, risk factors, and appropriate interventions for those affected by threats to the public’s health. | |
| Control | ||
| Goal 6 | Decrease the time needed to provide countermeasures and health guidance to those affected by threats to the public’s health. | |
| >Post-Event | Recover | |
| Goal 7 | Decrease the time needed to restore health services and environmental safety to pre-event levels. | |
| Goal 8 | Improve the long-term follow-up provided to those affected by threats to the public’s health. | |
| Improve | ||
| Goal 9 | Decrease the time needed to implement recommendations from after-action reports following threats to the public’s | |
| 2 The cooperative agreement funds 50 states, four metropolitan areas (Chicago, Los Angeles County, New York City, and Washington, DC), five territories (Puerto Rico, the Northern Mariana Islands, American Samoa, Guam, and the U.S. Virgin Islands), and three freely associated states (the Federated States of Micronesia, Palau, and the Marshall Islands). 3 CDC began funding selected public health departments in 1999, but the cooperative agreement’s support of 62 jurisdictions did not begin until 2002. | ||
Figure 1: Cooperative Agreement Allocated Funding, Fiscal Year 2002-2007 (in millions)
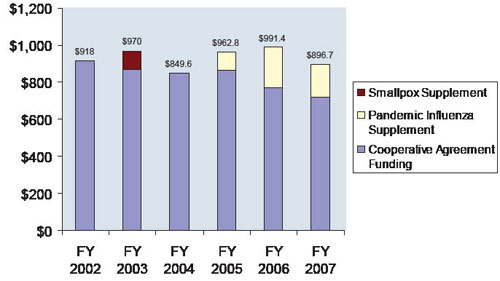
Source: HHS Press Releases; 2002-2007 – data for all 62 funded jurisdictions
As of 2007, the cooperative agreement has provided more than $5 billion to public health departments (Figure 1). Appendix 1 presents historical cooperative agreement funding levels for each funded public health department. The cooperative agreement supports:
- Collaboration among state, local, tribal, and territorial public health departments, research universities, and other responder agencies;
- Rapid identification of biological and chemical agents by public health laboratories across the country;
- Quick and accurate communication across local, state, and federal levels;
- Ongoing enhancement of state and local public health programs through a cycle of planning, exercising, and improvement plans;
- Protecting the health of the community and first responders during an emergency; and • Helping communities recover from emergencies.
Collaborating for preparedness. Local response agencies, including public health departments, are usually the first to respond during an emergency. For multi-state or severe emergencies, CDC may be asked to provide additional public health resources and coordinate response efforts across multiple jurisdictions. CDC monitors and often responds to major events that are potential nationwide health threats (Figure 2).
The National Preparedness Guidelines, published by the Department of Homeland Security (DHS), establish a vision, capabilities, and priorities for national preparedness. CDC preparedness goals support the target capabilities outlined in the National Preparedness Guidelines in areas such as detecting threats, public health laboratory testing, and communications. See Appendix 2 for more information on the National Preparedness Guidelines and DHS preparedness priorities.
CDC works under the strategic leadership of the Assistant Secretary for Preparedness and Response (ASPR) in the Department of Health and Human Services (HHS). Under the National Response Framework, HHS is responsible for coordinating federal assistance to supplement state, local, and tribal resources in response to public health and medical care needs for potential or actual emergencies. To achieve this, HHS works with other federal departments, including DHS, the U.S. Department of Agriculture (USDA), the Department of Defense, the Department of Veterans Affairs,the Department of Justice, and the Department of State. Appendices 3 and 4 detail how CDC and ASPR offices are currently working towards improving preparedness.
CDC and pubic health department partners include the American Public Health Association, the Association of Public Health Laboratories (APHL), the Association of Schools of Public Health, the Association of State and Territorial Health Officials, the Council of State and Territorial Epidemiologists (CSTE), and the National Association of County and City Health Officials (NACCHO). These organizations share best practices and lessons learned, conduct research, and provide training to public health professionals.

4 CDC, Division of Emergency Operations (DEO) Epi-Aid data; 2007
Local, state, and federal agencies must collaborate to effectively prepare for and respond to emergencies
Figure 2: Timeline of CDC Emergency Responses
| 2007 | XDR/MDR tuberculosis (May) Hurricane Dean (August) |
|---|---|
| 2006 | Mumps (April) Tropical storm Ernesto (August) E. coli in spinach (September) E. coli (December) |
| 2005 | Presidential inauguration (January) Marburg virus (March) Hurricane Katrina (August) Hurricanes Rita and Wilma (September) |
| 2004 | Avian influenza (January) BioWatch (February) Guam typhoon (February) Ricin domestic response (February) Cities Readiness Initiative (March) G8 Summit (June) Democratic National Convention (July) West Nile virus (August) Hurricanes Charley, Frances, Ivan, and Jean (August) Summer Olympics (August) Republican National Convention (August) Influenza vaccine shortage (October) Asian tsunami (December) |
| 2003 | Space shuttle Columbia disaster (February) SARS (March) Monkeypox (June) Northeast blackout (August) Hurricane Isabel (September) Ricin, tularemia, and anthrax (October) California wildfires (October) Domestic influenza (December) Mad cow disease (December) |
| 2002 | Ongoing monitoring of potential nationwide health threats |
| 2001 | World Trade Center attack (September) Anthrax attack (October) |
Get email updates
To receive email updates about this page, enter your email address:
Contact Us:
- Centers for Disease Control and Prevention
1600 Clifton Rd
Atlanta, GA 30333 - 800-CDC-INFO
(800-232-4636)
TTY: (888) 232-6348
24 Hours/Every Day - cdcinfo@cdc.gov

