Interim Guidance on Planning for the Use of Surgical Masks and Respirators in Health Care Settings during an Influenza Pandemic
October 2006 Contents
- Introduction
- Background: Influenza Transmission, Pathogenesis, and Control
Modes of Influenza Transmission
Droplet Transmission
Airborne Transmission
Aerosol-generating procedures
Contact Transmission (Direct and via Fomites) Pathogenesis of Influenza and Implications for Infection Control
Experience from Control of Seasonal Influenza Transmission
- Recommendations for Health Care Settings
Use of Surgical Masks and Respirators in Health Care Settings
Recommendations
Guidance for Correct Use
Appendix A Aerosol Science and Disease Transmission
Appendix B Types of Surgical Masks and Respirators Used in Health Care Settings
I. Introduction
Since the publication of the HHS Pandemic Influenza Plan (www.hhs.gov/pandemicflu/plan/) in November 2005, the U.S. Department of Health and Human Services (HHS) has received numerous comments and inquiries regarding infection control recommendations that relate to surgical mask and respirator use (e.g., N95 respirator[a]) during an influenza pandemic. Development of authoritative responses is hampered by the lack of definitive data about the relative contributions and importance of short-range inhalational exposure, large droplet mucosal exposure, and direct inoculation via hands or inanimate objects contaminated with virus (i.e., fomites) on influenza transmission There is only limited information on optimal interventions to prevent influenza transmission and the effectiveness of interventions on an individual basis. The lack of scientific consensus has led to conflicting recommendations by public health partners. Moreover, a large amount of incorrect, incomplete, and confusing information about surgical mask and respirator use has been disseminated on the Internet and by other popular media.
The Centers for Disease Control and Prevention (CDC) is aware of no new scientific information related to the transmission of influenza viruses since the drafting of the HHS Pandemic Influenza Plan (www.hhs.gov/pandemicflu/plan/). As stated in the plan, the proportional contribution and clinical importance of the possible modes of transmission of influenza (i.e., droplet, airborne, and contact) remains unclear and may depend on the strain of virus ultimately responsible for a pandemic. Nevertheless, in view of the practical need for clarification, CDC has re-reviewed the existing data, as described below, and has prepared interim recommendations on surgical mask and respirator use. The purpose of this document is to provide a science-based framework to facilitate planning for surgical mask and respirator use in health care settings during an influenza pandemic.
This document synthesizes traditional infection control and industrial hygiene approaches to enhancing protection of health care personnel during an influenza pandemic. It emphasizes that surgical mask and respirator use are components of a system of infection control practices to prevent the spread of infection between infected and non-infected persons. It also reflects concerns that additional precautions are advisable during a pandemic—beyond what is typically recommended during a seasonal influenza outbreak—in view of the lack of pre-existing immunity to a pandemic influenza strain, and the potential for the occurrence of severe disease and a high case-fatality rate. Extra precautions might be especially prudent during the initial stages of a pandemic, when viral transmission and virulence characteristics are uncertain, and medical countermeasures, such as vaccine and antivirals, may not be available.
The prioritization of respirator use during a pandemic remains unchanged: N95 (or higher) respirators should be worn during medical activities that have a high likelihood of generating infectious respiratory aerosols, for which respirators (not surgical masks) offer the most appropriate protection for health care personnel. Use of N95 respirators is also prudent for health care personnel during other direct patient care activities (e.g., examination, bathing, feeding) and for support staff who may have direct contact with pandemic influenza patients. If N95 or other types of respirators are not available, surgical masks provide benefit against large-droplet exposure and should be worn for all health care activities involving patients with confirmed or suspected pandemic influenza. Measures should be employed to minimize the number of personnel required to come in contact with suspected or confirmed pandemic influenza patients.
This document, Interim Guidance on Planning for the Use of Surgical Masks and Respirators in Health Care Settings during an Influenza Pandemic, augments and supersedes recommendations provided in Part 2 of the HHS Pandemic Influenza Plan (www.hhs.gov/pandemicflu/plan/#part2). This interim guidance document will be updated and amended as new information about the epidemiologic characteristics of the pandemic influenza virus becomes available.
Guidance documents on planning for surgical mask and respirator use in non-health care occupations and for the general community setting during an influenza pandemic are in preparation. Infection control recommendations related to seasonal influenza (www.cdc.gov/flu/professionals/infectioncontrol/) and avian influenza A (H5N1) (www.cdc.gov/flu/avian/professional/infect-control.htm) remain unchanged. The use of surgical masks by hospitalized patients and other symptomatic persons ("source control") is covered in the CDC’s Interim Guidance for the Use of Masks to Control Influenza Transmission (www.cdc.gov/flu/professionals/infectioncontrol/maskguidance.htm).
top of page
II. Background: Influenza Transmission, Pathogenesis, and Control
Modes of Influenza Transmission
Influenza is transmitted person to person through close contact. Transmission occurs through multiple routes, including large droplets and direct and indirect contact. Fine droplet inhalational transmission may also occur.
Most information on the modes of influenza transmission from person to person is indirect and largely obtained through analysis of outbreaks in health care facilities and other settings (e.g., cruise ships, airplanes, schools, and colleges). Although the knowledge base is limited, the epidemiologic pattern observed is consistent with transmission through close contact (i.e., exposure to large respiratory droplets, direct contact transfer of virus from contaminated hands to the nose or eyes, or exposure to small-particle aerosols in the immediate vicinity of the infectious individual [known as “short-range exposure to aerosols”]). The relative contributions and clinical importance of the different modes of influenza transmission are unknown. While some observational studies (1, 2) and animal studies (3, 4, 5) raise the possibility of short-range airborne transmission through small-particle aerosols, convincing evidence of airborne transmission of influenza viruses from person to person over long distances (e.g., through air-handling systems, or beyond a single room) has not been demonstrated. (6, 7, 8). However, one study in mice performed in a room outfitted with a slowly rotating fan to continuously agitate the air found that influenza virus sprayed into the room remained infective for some mice for extended periods (up to 24 hours) at room atmospheres of low humidity (17 to 24%). Room atmospheres with higher humidities into which virus suspension was sprayed were no longer infective in mice after one hour (3).
Droplet Transmission
Droplet transmission involves contact of the mucous membranes of the nose or mouth or the conjunctivae of a susceptible person with large-particle droplets containing microorganisms generated by an infected person during coughing, sneezing, or talking. Transmission via large-particle droplets requires close contact between source and recipient persons because these larger droplets do not remain suspended in the air and generally travel only short distances. Three feet has often been used by infection control professionals as a guide for “short distance” and is based on studies of respiratory infections (9, 10); however, for practical purposes, this distance may range from three to six feet. Special air handling and ventilation are not required to prevent droplet transmission.
On the basis of epidemiologic patterns of disease transmission, large droplet transmission—via coughing and sneezing—has traditionally been considered a major route of seasonal influenza transmission (7, 8).
>>Airborne Transmission
Airborne transmission occurs by dissemination of small particles or droplet nuclei[b] through the air (see Appendix A: Aerosol Science and Disease Transmission). Some organisms (e.g., Mycobacterium tuberculosis, measles virus, and varicella [chickenpox] virus) can remain infectious while dispersed over long distances by air currents, causing infection in susceptible individuals who have not had face-to-face contact (or been in the same room) with the infectious individual. Special air handling and ventilation systems (e.g., negative-pressure rooms or airborne isolation rooms) are used in health care settings to assist in preventing spread of agents that may be dispersed over long distances.
In contrast to tuberculosis, measles, and varicella, the pattern of disease spread for seasonal influenza does not suggest transmission across long distances (e.g., through ventilation systems); therefore, negative pressure rooms are not needed for patients with seasonal influenza (6, 8). However, localized airborne transmission may occur over short distances (i.e., three to six feet) via droplet nuclei or particles that are small enough to be inhaled. The relative contribution of short-range airborne transmission to influenza outbreaks is unknown.
Several often-cited papers raise concern about short-range aerosol transmission as a possible route of spread for influenza. These include laboratory studies in animals ( 3, 4, 5, 11), observational studies during the 1957-58 influenza pandemic (1), and an epidemiologic study of transmission on an airplane with an inoperative ventilation system (2). An experimental study in which the infectious dose of influenza virus was found to be as much as 100-fold lower for persons infected with small aerosols than with nasal drops (12) has further raised this concern. Although data are limited, the possibility remains that short-range aerosol transmission is a route of influenza transmission in humans and requires further study (13).
Aerosol-Generating Procedures
It is likely that some aerosol-generating medical procedures (e.g., endotracheal intubation, open suctioning, nebulizer treatment, bronchosocopy) could increase the potential for generation of small aerosols in the immediate vicinity of the patient. Although this mode of transmission has not been evaluated for influenza, given what is known about these procedures, additional precautions for health care personnel who perform aerosol-generating procedures on influenza patients are warranted.
Contact Transmission (Direct and via Fomites)
Contact transmission of influenza may occur through direct contact with contaminated hands, skin, or fomites followed by auto-inoculation of the respiratory mucosa. Influenza transmission via contaminated hands and fomites has been suggested as a contributing factor in some studies (14). There are insufficient data to determine the proportion of influenza transmission that is attributable to direct or indirect contact. However, it is prudent to reinforce recommendations for thorough and frequent handwashing, which is known to reduce the likelihood of contamination of the environment and to reduce transmission of respiratory infections (15, 16, 17). Surgical mask or respirator use may provide an additional benefit by discouraging facial contact and subsequent autoinoculation.
Pathogenesis of Influenza and Implications for Infection Control
Human influenza is a disease of the respiratory tract. Influenza virus infects respiratory epithelial cells via receptors found principally in non-ciliated cells of the upper respiratory tract; infection also can occur in the lower respiratory tract (18, 19). There is no natural or experimental evidence that human seasonal influenza virus infection of the gastrointestinal tract can occur.
While conjunctivitis may be associated with human infection with some avian influenza viruses (20, 21), ocular infection does not appear to be a primary route for transmission of human influenza viruses, although data are very limited. Nonetheless, it is prudent to prevent exposure of the eyes as well as the mucous membranes of the respiratory tract to possibly infectious material (e.g., as may occur when health care workers perform splash-generating procedures).
Experience from Control of Seasonal Influenza Transmission
Outbreaks of seasonal influenza in hospitals and long-term care facilities have been prevented or controlled through a set of well-established strategies that include the following:
- seasonal influenza vaccination of patients and health care personnel
- early detection of influenza cases in a facility
- antiviral treatment of ill persons and prophylactic treatment of particularly susceptible persons
- implementation of the following administrative measures
- restricting visitors
- educating patients and staff
- cohorting health care personnel assigned to an outbreak unit
- isolation of infectious patients in private rooms or cohorted units
- practicing and emphasizing the importance of good hand hygiene
- use of appropriate barrier precautions (e.g., masks, gloves, and gowns) during patient care, as recommended for Standard and Droplet Precautions (8). Respirators have not been routinely recommended for control of seasonal influenza outbreaks.
Used together, these measures have been successful in controlling outbreaks of seasonal influenza in health care settings; however, the relative contributions of each of the interventions listed above remain unknown, and their specific impact during a pandemic is difficult to predict.
top of page
III. Recommendations for Health Care Settings
Use of Surgical Masks and Respirators in Health Care Settings
Surgical mask and respirator use is one component of a system of infection control practices to prevent the spread of infection between infected and non-infected persons where pandemic influenza patients might receive health care services (e.g., hospitals, emergency departments, out-patient facilities, residential care facilities, emergency medical services, home health care delivery). During an influenza pandemic, surgical masks and respirators—along with other forms of personal protective equipment (e.g., gloves, gowns, and goggles)—should be used by health care personnel in health care settings in conjunction with Standard and Droplet Precautions, respiratory hygiene, cough etiquette, vaccination, and early diagnosis and treatment. Different types of surgical masks and respirators are described in Appendix B.
Recommendations
- National Institute for Occupational Safety and Health (NIOSH)-certified respirators (N95 or higher) are recommended for use during activities that have a high likelihood of generating infectious respiratory aerosols,[c] including the following high-risk situations:[d]
- Aerosol-generating procedures (e.g., endotracheal intubation, nebulizer treatment, and bronchoscopy) performed on patients with confirmed or suspected pandemic influenza
- Resuscitation of a patient with confirmed or suspected pandemic influenza (i.e., emergency intubation or cardiac pulmonary resuscitation)
- Providing direct care for patients with confirmed or suspected pandemic influenza-associated pneumonia (as determined on the basis of clinical diagnosis or chest x-ray), who might produce larger-than-normal amounts of respirable infectious particles when they cough
In the event of actual or anticipated shortages of N95 respirators:
- Other NIOSH-certified N-, R-, or P-class respirators should be considered in lieu of the N95 respirator.
- If re-useable elastomeric respirators are used, these respirators must be decontaminated according to the manufacturer’s instructions after each use.
- Powered air purifying respirators (PAPRs) may be considered for certain workers and tasks (e.g., high-risk activities). Loose-fitting PAPRs have the advantages of providing eye protection, being comfortable to wear, and not requiring fit-testing; however, hearing (e.g., for auscultation) is impaired, limiting their utility for clinical care. Training is required to ensure proper use and care of PAPRs.
- Use of N95 respirators for other direct care activities involving patients with confirmed or suspected pandemic influenza is also prudent. Hospital planners should take this into consideration during planning and preparation in their facilities when ordering supplies. In addition, several measures can be employed to minimize the number of personnel required to come in contact with suspected or confirmed pandemic influenza patients, thereby reducing worker exposure and minimizing the demand for respirators. Such measures include the following:
- Establishing specific wards for patients with pandemic influenza
- Assigning dedicated staff (e.g., health care, housekeeping, janitorial) to provide care for pandemic influenza patients and restricting those staff from working with non-influenza patients
- Dedicating entrances and passageways for influenza patients
Planning assumptions and projections suggest that shortages of respirators are likely in a sustained pandemic (22). Therefore, in the event of an actual or anticipated shortage, hospital planners must ensure that sufficient numbers of respirators are prioritized for use during the high-risk procedures described in Recommendation 1. This will require careful planning as well as real-time supply monitoring to ensure that excess respirators are not held in reserve while health care personnel are conducting activities for which they would otherwise be provided respiratory protection. Conversely, excessive use of respirators could result in their unavailability for high-risk procedures. Decision guidance for determining respirator wear should consider factors such as duration, frequency, proximity, and degree of contact with the patient. Occupational health and safety professionals can assist with making these site- and activity-specific decisions. For example, a nurse entering a room with a suspected or confirmed pandemic influenza patient to obtain vital signs should wear an N95 respirator. A housekeeper entering multiple rooms of confirmed or suspected influenza patients to mop floors or clean patient equipment should be similarly protected. Work activities such as those performed by a receptionist at the entrance of a hospital should be designed to prevent exposure of the worker to large numbers of potentially infected patients. In such situations, the use of transparent barriers or enclosures is preferable to the use of respirators.
If supplies of N95 (or higher) respirators are not available, surgical masks can provide benefits against large droplet exposure, and should be worn for all health care activities for patients with confirmed or suspected pandemic-influenza.
- Negative pressure isolation is not required for routine patient care of individuals with pandemic influenza. If possible, airborne infection isolation rooms should be used when performing high-risk aerosol-generating procedures. If work flow, timing, resources, availability, or other factors prevent the use of airborne infection isolation rooms, it is prudent to conduct these activities in a private room (with the door closed) or other enclosed area, if possible, and to limit personnel in the room to the minimum number necessary to perform the procedure properly.
Guidance for Correct Use
Respirator use should be in the context of a complete respiratory protection program in accordance with Occupational Safety and Health Administration (OSHA) regulations. Detailed information on respiratory protection programs, including fit test procedures, can be accessed at OSHA’s Respiratory Protection eTool (www.osha.gov/SLTC/etools/respiratory). Staff with responsibility for direct patient care should be medically cleared, trained, and fit-tested for respirator use. Training topics should include the following:
- Proper fit-testing, wearing, and use of respirators
- Safe removal of respirators
- Safe disposal of respirators
- Medical contraindications to respirator use
If a respirator that provides protection from splashes of blood or body fluids is needed, NIOSH-certified, FDA-cleared surgical N95 (or higher) respirators should be selected. Additional information on N95 respirators and other types of respirators may be found in Appendix B , at: NIOSH’s Respirator Fact Sheet (http://www.cdc.gov/niosh/npptl/topics/respirators/factsheets/respfact.html), and at FDA’s Masks and N95 Respirators (www.fda.gov/cdrh/ppe/masksrespirators.html) fact sheet.
Persons who wear surgical masks or respirators should be advised that:
- Surgical mask or respirator use should not take the place of preventive interventions, such as respiratory etiquette and hand hygiene.
- To offer protection, surgical masks and respirators must be worn correctly and consistently throughout the time they are used.
- Wearing a surgical mask or respirator incorrectly, or removing or disposing of it improperly, could allow contamination of the hands or mucous membranes of the wearer or others, possibly resulting in disease transmission.
- Proper surgical mask or respirator use and removal includes the following:
- Prior to putting on a respirator or surgical mask, wash hands thoroughly with soap and water or use an alcohol-based hand sanitizer to reduce the possibility of inadvertent contact between contaminated hands and mucous membranes.
- If worn in the presence of infectious persons, a respirator or surgical mask may become contaminated with infectious material; therefore, avoid touching the outside of the device to help prevent contamination of hands.
- Once worn in the presence of a patient with patient with pandemic influenza, the surgical mask or disposable N95 respirator should be removed and appropriately discarded.
- After the surgical mask or respirator has been removed and discarded, wash hands thoroughly with soap and water, or use an alcohol-based hand sanitizer.
- Further information can be found at http://www.cdc.gov/ncidod/sars/respirators.htm and http://www.cdc.gov/niosh/npptl/topics/respirators/factsheets/respsars.html#F.
References
- Jordan WS Jr. The mechanism of spread of Asian influenza. Am Rev Respir Dis 1961 83:29-40.
- Moser MR, Bender TR, Margolis HS, Noble GR, Kendal AP, Ritter DG. An outbreak of influenza aboard a commercial airliner. Am J Epidemiol 1979;110:1-6.
- Loosli CG, Lemon HM, Robertson OH, Appel E. Experimental airborne influenza infection. I. Influence of humidity on survival of virus in air. Proc Soc Exp Biol 1943;53:205-6.
- Schulman JL. Experimental transmission of influenza virus infection in mice. IV. Relationship of transmissibility of different strains of virus and recovery of airborne virus in the environment of infector mice. J Exp Med 1967;125:479-88.
- Schulman JL. The use of an animal model to study transmission of influenza virus infection. Am J Public Health Nations Health 1968;58:2092-6.
- Blumenfeld HL, Kilbourne ED, Louria DB, Rogers DE. Studies on influenza in the pandemic of 1957-1958. I. An epidemiologic, clinical and serologic investigation of an intrahospital epidemic with a note on vaccination efficacy. J Clin Invest 1959;38:199-212.
- Bridges CB, Kuehnert MJ, Hall CB. Transmission of influenza: implications for control in health care settings. Clin Infect Dis 2003;37:1094-1101.
- Salgado CD, Farr BM, Hall KK, Hayden FG. Influenza in the acute hospital setting. Lancet Infect Dis 2002;2:145-55.
- Hamburger M Jr, Robertson OH. Expulsion of Group A hemolytic streptococci in droplets and droplet nuclei by sneezing, coughing, and talking. Am J Med 1948; 4:690-701.
- Feigin RD, Baker CJ, Herwaldt LA, Lampe RM, Mason EO, Whitney SE. Epidemic meningococcal disease in an elementary school classroom. N Engl J Med 1982;307:1255-7.
- Andrews CH, Clover RE. Spread of infection from the respiratory tract of the ferret. 1. Transmission of influenza A virus. Br J Exp Pathol 1941;22:91-7.
- Alford RH, Kasel JA, Gerone PJ, Knight V. Human influenza resulting from aerosol inhalation. Proc Soc Exp Biol Med 1966;122:800-4.
- Tellier R. Review of aerosol transmission of influenza A virus. Emerg Infect Dis [serial on the Internet]. 2006 Nov (accessed September 29, 2006). http://www.cdc.gov/ncidod/EID/vol12no11/06-0426.htm
- Bean B, Moore BM, Sterner B, Peterson LR, Gerding DN, Balfour HH Jr. Survival of influenza viruses on environmental surfaces. J Infect Dis 1982;146:47-51
- World Health Organization Writing Group. Nonpharmaceutical public health interventions for pandemic influenza, national and community measures. Emerg Infect Dis 2006;12:88-94. www.cdc.gov/ncidod/EID/vol12no01/05-1370.htm
- Boyce JM, Pittet D. Guideline for hand hygiene in health-care settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Am J Infect Control 2002;30:S1-46.
- Ryan MA, Christian RS, Wohlrabe J. Handwashing and respiratory illness among young adults in military training. Am J Prev Med 2001;21:79-83.
- Matrosovich MN, Matrosovich TY, Gray T, Roberts NA, Klenk HD. Human and avian influenza viruses target different cell types in cultures of human airway epithelium. Proc Natl Acad Sci USA 2004;101:4620-4.
- Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. Influenza virus receptors in the human airway. Nature 2006;440:435-6.
- Du Ry van Beest Holle M, Meijer A, Koopmans M, de Jager C, van de Kamp EEHM, Wilbrink B, Conyn-van Spaendonck MAE, Bosman A. Human-to-human transmission of avian influenza A/H7N7, The Netherlands, 2003. Euro Surveill 2005;10:264-8.
- Tweed SA, Skowronski DM, David ST, Larder A, Petric M, Lees W, Li Y, Katz J, Krajden M, Tellier R, Halpert C, Hirst M, Astell C, Lawrence D, Mak A. Human illness from avian influenza H7N3, British Columbia. Emerg Infect Dis 2004;10:2196-9.
- Institute of Medicine. Reusability of facemasks during an influenza pandemic: facing the flu. Report of the Committee on the Development of Reusable Facemasks for Use During an Influenza Pandemic. Washington, D.C.: The National Academies Press, 2006. http://www.nap.edu/catalog/11637.html.
top of page
Appendix A
Aerosol Science and Disease Transmission
Pathogen-carrying particles (“infectious” or “contaminated”) of many different sizes are generated from various regions of the human airways and respiratory tract when a person with a respiratory infection talks, coughs, or sneezes (1). The smallest particles are generated in the pulmonary region, while larger particles are produced in the nasopharyngeal area. Although a particle’s size may determine its behavior and mode of transmission, its infectivity also is affected by host factors, environmental factors, and pathogen-related factors (1, 2, 3, 4, 5).
Airborne pathogens may be divided into three functional types: a) obligate airborne pathogens, like M. tuberculosis, b) preferential airborne pathogens that are sometimes transmitted via other routes (like measles virus and variola [smallpox] virus), and c) opportunistic airborne pathogens that can be transmitted through the air under special circumstances that produce a concentrated source of contaminated small particles (1). Influenza virus is thought to fall into the third category, as a pathogen transmitted via large droplets that may also be inhaled (6, 7) if infectious respirable aerosols are present (e.g., due to an aerosol-generating medical procedure and possibly also due to short-range aerosol transmission during other direct care activities, as discussed in Section II).
Particle Size and Routes of Disease Transmission
Conflicting definitions applied to particles, particularly “large droplets,” are a source of continuing confusion. Harmonized definitions and categorizations for these particles are needed to provide unambiguous and robust infection control recommendations. In discussing the relationship between the size of an infectious particle and routes of disease transmission, it may be useful to consider the characteristics of three size ranges (large, intermediate, and small):
- Large droplets (greater than 50 – 100 µm in diameter). Large droplets do not remain suspended in the air for significant periods of time, are affected primarily by gravity, have a ballistic trajectory, and travel no further than a few feet from the infected person (2). Disease transmission occurs by direct contact of contaminated large droplets with the mucous membranes of the mouth, eyes, and nasal passageways.
- Intermediate-size[e] particles (10 – 50 µm). The dispersion, settling, and respiratory-tract deposition of intermediate-size particles is affected by environmental factors such as temperature, humidity, air velocity, and air currents. As with large droplets, disease transmission via contaminated intermediate-size particles can occur by direct contact with mucous membranes if the particle is able to remain infective while suspended. Some intermediate-size particles may quickly decrease in diameter due to water loss, becoming “droplet nuclei” capable of causing airborne disease transmission (3).
- Small particles (less than 10 µm). This category includes small particle aerosols generated directly from a cough or sneeze, as well as droplet nuclei caused by desiccation and shrinkage of intermediate-size droplets. Particles that are five µm or less in diameter can remain airborne for an extended period (8) and may cause infection if the organism is able to maintain infectivity during desiccation and suspension in air. These particles reach the pulmonary region with variable efficiency and deposition properties. Their dispersion and deposition is principally affected by air currents.
Data on the proportions of different size particles expelled by an average cough or sneeze are limited (2, 3), and the proportions may change over time due to their desiccation and shrinkage. The point at which a shrinking particle moves out of droplet-transmission size-range and into the aerosol-transmission size-range is unclear. Moreover, the size ranges of the two populations of particles (capable of droplet or airborne transmission) might overlap or shift, depending on environmental conditions.
The characteristics of partially dried droplets and fully dried nuclei are similar to those of smaller particles that are expelled directly. However, infectivity or adherence properties may differ.
Factors That Influence a Particle's Infectivity
The size of a contaminated particle largely determines how quickly it will settle and whether it is likely to be inhaled into the lung (3). However, several other factors affect the likelihood that it will cause an infection, some directly, and some indirectly (2, 3).
Host factors include the following:
- The particle emission rate (frequency of coughing and sneezing)
- The concentration of aerosols in the cough or sneeze
- Susceptibility to infection of the person who comes into contact with the particle (e.g., immune status)
Pathogen-related factors may include the following:
- The initial concentration of the pathogen in the respiratory fluid
- The duration of infectivity of the pathogen suspended in air
- The number of pathogens that must be inhaled to cause infection (the infectious dose)
- Whether a certain size particle is required to carry a particular pathogen
Environmental factors , which can affect the rate of partial desiccation of intermediate size droplets into small respirable particles and the rate of complete desiccation of small respirable particles, include:
- Temperature and humidity
- Air currents
- Sunlight
- Electrostatic conditions
- The rate of removal of particles through exhaust ventilation
- The rate of removal of particles via air disinfection systems (e.g., ultraviolet light, filtration)
- Whether the susceptible person is downwind or upwind from the source
Factors That Influence the Infectivity of Influenza-Virus-Carrying Particles
The fact that M. tuberculosis, measles virus, and varicella virus are able to cause infection over long distances suggests that—as compared with influenza virus—they may have a lower infectious dose, may be present in higher concentrations in respiratory fluid, and/or can remain infective longer in air.
Research is needed to determine the pathogen-related capabilities and characteristics (e.g., persistence of infectivity, infectious dose,, and concentration in respiratory fluid) of an influenza-virus–carrying small particle or droplet nucleus under specific host-related and environmental conditions. This information will help in evaluating the potential efficacy of control measures to prevent infection.
Key Knowledge Gaps and Research Needs
The following research questions must be addressed to improve infection control strategies for influenza viruses:
- What is the role of localized airborne transmission of small particles and droplet nuclei in the spread of human influenza viruses?
- What are the relative contributions of large droplets versus small particles and droplet nuclei to disease transmission?
- What are the efficacy and effectiveness of the use of N95 respirators and surgical masks in preventing influenza transmission?
- What strategies are likely to be most effective in promoting adherence to infection control measures during a pandemic?
- Is there a risk to users from potentially contaminated surgical masks and respirators (e.g., does influenza virus persist in surgical mask/respirator materials)?
References
- Roy CJ, Milton DK. Airborne transmission of communicable infection—the elusive pathway. N Engl J Med 2004;350:1710-2.
- Papineni RS, Rosenthal FS. The size distribution of droplets in the exhaled breath of health human subjects. J Aerosol Med 1997;10:105-16.
- Nicas M, Nazaroff WW, Hubbard A. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. J Occup Environ Hyg 2005:2:143-54.
- Yu IT, Li Y, Wong TW, Tam W, Chan AT, Lee JH, Leung DY, Ho T. Evidence of airborne transmission of the severe acute respiratory syndrome virus. N Engl J Med 2004;350:1731-9.
- Tellier R. Review of aerosol transmission of influenza A virus. Emerg Infect Dis [serial on the Internet]. 2006 Nov (accessed September 29, 2006). http://www.cdc.gov/ncidod/EID/vol12no11/06-0426.htm
- Henle W, Henle G, Stokes J Jr, Maris EP. Experimental exposure of human subjects to viruses of influenza. J Immunol 1945;52:145 65.
- Alford RH, Kasel JA, Gerone PJ, Knight V. Human influenza resulting from aerosol inhalation. Proc Soc Exp Biol Med 1966;122:800-4.
- Lenhart SW, Seitz T, Trout D, Bollinger N. Issues affecting respirator selection for workers exposed to infectious aerosols: emphasis on healthcare settings. Applied Biosafety 2004;9:20-36.
top of page
Appendix B
Types of Surgical Masks and Respirators Used in Health Care Settings
Surgical masks and respirators may be used to protect the respiratory tract from viruses, bacteria, and fungi transmitted through direct contamination of the mucous membranes of the nose and mouth (and sometimes the eyes) or through inhalation of organisms in the air.
Surgical Masks
Masks that provide protection against pathogens carried by large respiratory droplets that can contaminate the mucous membranes are commonly known as surgical masks (Figure 1). These masks—which are sometimes also called procedure, isolation, or laser masks—are:
- Designed to cover the mouth and nose loosely
- Usually strapped behind the head
- Made of soft materials and are comfortable to wear
Surgical masks are worn by surgeons and other operating room personnel to prevent organisms in their noses and mouths from falling into the sterile field and potentially causing surgical site infections. Surgical masks also provide protection against body fluid splashes to the nose and mouth. Since surgical masks do not have a sealing surface and only fit loosely, they provide only minimal protection from respirable particles (1).
Respirators
Respiratory filtering devices that provide protection against inhalation of small and large airborne particles are called particulate respirators or air-purifying respirators . A particulate respirator is worn on the face and fits tightly to cover the nose and mouth.
Particulate respirators include the following:
- Disposable or filtering facepiece respirators are made of filter material designed to remove airborne particles. Disposable filtering facepiece respirators are discarded once they become unsuitable for further use because of soiling, contamination, or physical damage.
- Reusable or elastomeric respirators use replaceable filters. Elastomeric respirator facepieces can be cleaned, disinfected, and fitted with new filters for reuse. Such respirators typically have an exhalation valve and, when worn by an infected person, would not prevent transmission of virus to other persons.
- Powered air-purifying respirators (PAPRs) use a battery-powered blower to provide filtered breathing air. PAPRs can be cleaned, disinfected, and fitted with new filters for re-use.
The respirators most commonly used in hospitals are:
- The N95 filtering facepiece respirator (Figure 2)
- The powered air purifying respirator (PAPR) (Figure 3)
N95 respirators . An N95 respirator is one of nine classes of particulate respirators certified by NIOSH. NIOSH-certified disposable particulate respirators are rated—and named—according to their ability to filter out 95%, 99%, or 99.97% (essentially 100%) of small inhalable particles, as well as according to their resistance to filter degradation from oil. Respirators are rated “N” if they are not resistant to oil, “R” if they are somewhat resistant to oil, and “P” if they are strongly resistant (oil proof).[f] Types of NIOSH-certified respirators include N95, N99, and N100; R95, R99, and R100; and P95, P99, and P100.
N-95 respirators:
- Fit closely to form a tight seal over the mouth and nose
- Must be fit-tested and adjusted to one’s face
- Must be safely removed and discarded
Surgical N95 respirators are N95 respirators that are FDA-cleared as surgical masks, as well as NIOSH-certified as respirators. They have all of the qualities of NIOSH-certified N95 respirators and have been evaluated for fluid resistance, flammability, and biocompatibility (see Masks and N95 Respirators [www.fda.gov/cdrh/ppe/masksrespirators.html]).
Powered air purifying respirators (PAPRs). A powered air purifying respirator uses its own power source and a HEPA (high-efficiency particulate air) filter to provide the wearer with his or her own filtered air supply. Because a HEPA filter is as efficient as a P-100 filter—and because PAPRs have less face-seal leakage—a PAPR provides a higher level of respiratory protection than a filtering facepiece or a half-mask elastomeric respirator.
If a filtering facepiece respirator (N95 or higher) is not available or cannot be correctly fitted or safely worn, other appropriate alternatives include PAPRs and half-face or full-face elastomeric respirators. Care must be used to prevent exposure of the wearer to infectious material that may be on the outer surfaces of the face shield and shroud. The reusable parts of a PAPR should be cleaned and disinfected after use and the filters replaced in accordance with manufacturer’s recommendations. All used HEPA filters should be considered possibly contaminated with infectious material and must be safely discarded. An appropriate system should be in place to ensure that backpacks are recharged and maintained according to the manufacturer’s instructions.
Additional Information on Respirators
The NIOSH Certified Equipment List (www.cdc.gov/niosh/npptl/topics/respirators/cel/) includes all types of NIOSH-certified respirators. NIOSH has also posted a list of disposable particulate respirators (http://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/).
The Occupational Safety and Health Administration (OSHA) regulates the use of respirators in health care settings by setting standards for operation, maintenance, and care. Detailed information on respiratory protection programs, including fit test procedures, may be found at the Respiratory Protection eTool (www.osha.gov/SLTC/etools/respiratory/) site.
Reuse of Filtering Facepiece Respirators
An Institute of Medicine committee recently reported that disposable masks and respirators do not lend themselves to reuse because they work by trapping harmful particles inside the mesh of fibers of which they are made (2). This hazardous buildup cannot be cleaned out or disinfected without damaging the fibers or other components of the device, such as the straps or nose clip. Moreover, the committee could not identify any simple modifications to the manufacturing of the devices that would permit reuse, or any changes that would dispense with the need to test the fit of respirators to ensure a wearer is fully protected. However, the committee suggested that, if necessary, a disposable N95 respirator can be reused with the following precautions: 1) a protective covering such as a medical mask or a clear plastic face shield should be worn over the respirator to protect it from surface contamination; 2) the respirator should be carefully stored between uses; and 3) the wearer should wash his or her hands before and after handling the respirator and the device used to shield it. These steps are intended for reuse of a respirator by a single person.
References
- Lawrence RB, Duling MG, Calvert CA, Coffey CC. Comparison of performance of three different types of respiratory protection devices. J Occup Environ Hyg 2006:3: 465-74.
- Institute of Medicine. Reusability of facemasks during an influenza pandemic: facing the flu. Report of the Committee on the Development of Reusable Facemasks for Use During an Influenza Pandemic. Washington, D.C.: The National Academies Press, 2006. http://www.nap.edu/catalog/11637.html
Figure 1. Surgical Mask

Figure 2. N95 Filtering Facepiece Respirators (A-E)
A. Cup style N95 respirator:

Photo courtesy of Moldex
B. Duckbill N95 respirator
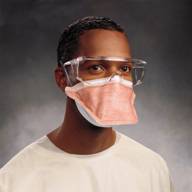
Photo courtesy of Kimberly-Clark
C. Fan fold N95 respirator

Photo courtesy of Alpha Pro Tech
D. Flat fold N95 respirator
Photo courtesy of 3M | |  Photo courtesy of NIOSH |
E. Pleated N95 respirator
Photos courtesy of Aearo | |  Photos courtesy of AO Safety |
Figure 3. Powered, Air-Purifying Respirators with Loose-fitting Hood

Photo courtesy of Bullard
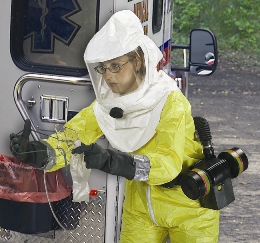
Photo courtesy of MSA
top of page
[a]Unless otherwise specified, throughout this document "N95 respirator" refers to a NIOSH-certified N95 filtering facepiece respirator.
[b]Droplet nuclei are formed by evaporation of droplets expelled by a cough or sneeze. See also Appendix A.
[c]If protection from splashes of blood or body fluids is also needed, NIOSH-certified, FDA-cleared surgical N95 (or higher) respirators should be selected. More information is available at www.fda.gov/cdrh/ppe/masksrespirators.html.
[d]Some of the high-risk activities or conditions listed may have a higher potential for generating infectious respiratory aerosols. Site-specific factors, including patient condition, history, experience, work environment, and activity duration, should be considered when assessing risk and priority
[e]Intermediate-size particles include inhalable or inspirable particles and can settle in the bronchi and the bronchioles of the lung but tend not to penetrate into the smaller airways found in the alveolar region. Respirable particles are sufficiently small to penetrate the alveolus, where gas is exchanged.
[f]Resistance to oil is an important quality for some industrial uses of respirators, but is not relevant for health care use.