|
|
|||||
|
|
In Palm Beach County, Florida, during the summer of 2003 a cluster of eight cases of malaria was detected. The background incidence is 60 cases per year (Florida) and 10 cases per year (Palm Beach County).
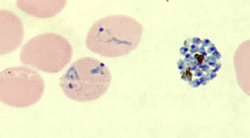
All patients were infected by the same parasite species shown in the figure. 1. What is that species? All patients were male. Their ages varied from 17-45 (median 37). None had a history of prior malaria infection, recent history of travel in a malaria-endemic area, blood transfusion or organ transplantation or intravenous drug use. They were from very diverse backgrounds, including one homeless man living near a drainage canal, two undocumented workers, and one affluent banker who liked to golf in the evening). All lived within 10 miles of Palm Beach International Airport.) 2. Among the modes of infection below, which one(s) need to be given the most serious consideration?
The dates of onset of symptoms, between July 12 and September 14, are shown in the epi curve above. 3. Based on that curve and what is known of the biology of P. vivax, the most likely occurrence is that all patients were infected by:
The microscopic diagnosis of P. vivax was confirmed by PCR. Parasite multilocus genotyping indicated that all parasites were the same strain, further supporting that the 8 infections originated from the same source. In that scenario, a person infected in an endemic country with P. vivax arrived in Palm Beach County and was bitten by local Anopheles mosquitoes, leading to the 2-3 cycles of local transmission in local residents ("autochtonous malaria"). 4. What would be the next steps of the epidemiologic investigation? (one or more answers may apply)
Surveys of local health facilities and hospital charts, and community canvassing did not identify any additional cases, or index case. Mosquito traps were set within a one-mile radius of the homes of the patients, and Anopheles quadrimaculatus and An. crucians, both potential vectors of malaria, were found near at least 3 homes (figure). None of the mosquitoes were positive for malaria (by sporozoite ELISA).
In addition to the investigations described above, the local health authorities:
Main points
1. In the United States, malaria has been eliminated but it can be reintroduced
because travelers and immigrants may have malaria and local Anopheles mosquitoes
can transmit malaria. This outbreak was published in Local Transmission of Plasmodium vivax Malaria --- Palm Beach County, Florida, 2003 Vol 52, No 38;908 09/26/2003 Page last modified : April 23, 2004 Content source: Division of Parasitic Diseases National Center for Zoonotic, Vector-Borne, and Enteric Diseases (ZVED)
|
|
||||||||||||||||||||||||||||
| Home | Policies and Regulations | Disclaimer | e-Government | FOIA | Contact Us | ||||||
|