|
|
|||||
|
|
Case 1A 44-year-old male is seen at a physician's office in the United States, during a week-end, for suspected malaria. The patient was born in Pakistan but has lived in the US for the past 12 years. He travels frequently back to Pakistan to visit friends and relatives. His last visit there was for two months, returning 11 months before the current episode. He did not take malaria prophylaxis then. Five weeks ago, he was diagnosed with malaria and treated at a local hospital. The blood smear at that time was reported by the hospital as positive for Plasmodium malariae (schizonts, trophozoites). He was then treated with 2 days of IV fluids (nature unknown) and tablets (nature unknown), and recovered. The patient now presents with a history of low grade fever for the past few days, with no other symptoms . A blood smear is taken and examined at a hospital laboratory by the technician (no pathologist is available on this week-end). Through a telephone discussion, the technician states that she sees 4 parasites per 1000 red blood cells, with rings, "other forms with up to four nuclei", and that some of the infected red blood cells are enlarged and deformed. Question 1. What is your most probable diagnosis? Question 2. What treatment approach would you recommend, based on this clinical history and on the fact that the microscopy findings will not be confirmed by a pathologist for at least 24 hours?
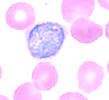
The diagnosis of P. vivax malaria is later confirmed by review of a blood smear available from the first episode (Figure), and by a PCR positive for P. vivax on blood collected during the current episode.
The
microscopic
diagnosis of P. vivax is based on the following: a) the infected
red cells are enlarged and deformed; b) the schizont shown contains 20
merozoites (schizonts of P. malariae and P. ovale have fewer
merozoites; and in P. falciparum schizonts are not usually seen
in the peripheral blood); c) the round gametocyte shown, contained in
an enlarged red cell. (In this case, the typical Schüffner's dots
were not visible, probably due to staining problems.) Question 3. To prevent further relapses from dormant liver stages, what would you recommend?
Question 4. Should this patient have taken preventive measures against malaria for his visit to Pakistan, considering that he was born there, and probably would have visited only cities? Main Points
Page last modified : April 23, 2004 Content source: Division of Parasitic Diseases National Center for Zoonotic, Vector-Borne, and Enteric Diseases (ZVED)
|
|
||||||||||||||||||||||||
| Home | Policies and Regulations | Disclaimer | e-Government | FOIA | Contact Us | ||||||
|