|
Insecticide-Treated Bed Nets
 |
A Nigerian
woman and her baby show their insecticide-treated bed
net. (Courtesy The Carter Center/E. Staub) |
Insecticide-treated
bednets (ITNs) decrease death and disease due to malaria,
and their mass distribution to children under five and to pregnant
women is now a major
intervention against malaria in Africa.
However, the distribution of ITNs can be costly and difficult
to organize, and these issues can prevent them from getting
to the remote populations who need them most. Public health
workers have improved coverage of ITNs by linking their distribution
with campaigns against other health problems such as measles,
polio, and intestinal worms. Recent experience in Nigeria
shows successful linkage with yet another disease, lymphatic
filariasis.
Lymphatic Filariasis
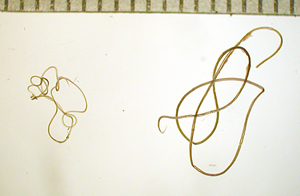 |
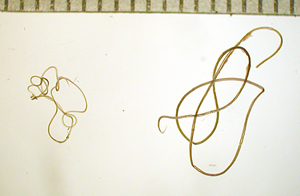
Wuchereria
bancrofti is the main agent of lymphatic filariasis
in Nigeria. Adult worms (shown here) clog and destroy
the lymphatic drainage system, leading to elephantiasis.
Female worms (right) measure up to 4 inches, while
males (left) are smaller. (CDC photo) |
Lymphatic
filariasis (LF), a parasitic infection transmitted by mosquitoes,
affects over 120 million people in more than 80
countries. The adult female worms generate young worms
(microfilariae),
which circulate in the blood and which, when picked up by
a mosquito, can result in the infection of another person.
LF is a leading cause of disability worldwide. The adult worms
live for years in the infected person’s lymphatic system, which
they clog and damage. This process can result in lymphedema and elephantiasis,
an incapacitating swelling in the legs, genital organs, or arms. The
affected parts are often secondarily infected by bacteria,
and the disease may persist a lifetime.
Global Campaign to Eliminate Lymphatic Filariasis
Following a 1993 report by the Carter
Center's International Task Force for Disease Eradication, the World
Health Organization in 1997 called for the elimination of LF.
This task is currently
 |
A
woman in Nigeria washes her left leg and foot, swollen
by lymphatic filariasis; more
advanced cases can be very
crippling; frequent washing with soap and water helps
prevent bacterial superinfection. (Courtesy The Carter
Center/F. Richards) |
coordinated by the Global
Alliance to Eliminate Lymphatic Filariasis. The alliance’s
strategy is to interrupt the transmission of LF by eliminating
the microfilariae through annual mass drug administration
(MDA), and to alleviate and prevent suffering caused by the disease.
MDAs aim to administer to entire populations in the affected areas
a single oral dose of diethylcarbamazine or ivermectin (Mectizan®,
donated by Merck & Co’s Mectizan
Donation Program)* combined with albendazole (donated by GlaxoSmithKline’s Global
Community Partnerships Lymphatic Filariasis Program).* The drugs
are not given to young children or to pregnant women.
Joining Efforts in Nigeria
In Africa, LF and malaria often occur in the same locales and are
transmitted by the same mosquitoes. Combining the health interventions
directed against these two diseases into a single bundle may prove beneficial.
Sharing the resources may reduce costs, and protection from the mosquito
vectors may reduce transmission of both diseases.
This is particularly
true when considering that children under five and pregnant
women do not receive the drugs during MDA campaigns but are the target
groups for receiving ITNs. Since 2000, the ministries of health of two
states in central Nigeria (Plateau and Nasarawa states), assisted by
the Nigerian Federal ministry of health, the
Carter Center’s Lymphatic Filariasis Program, and CDC, have
organized yearly MDAs to eliminate LF. These have evolved into
well-established systems for drug distribution, with more than 3.2 million
persons treated in 2004.
Going one step further, the states’ LF and malaria programs
developed a collaboration to fight both diseases simultaneously,
by piggybacking to the MDA campaign the distribution of ITNs
donated by the Roll
Back Malaria Partnership. In two demonstration districts, Kanke
and Akwanga (combined population approximately 218,000), the
two programs developed logistical systems, trained distributors,
and educated local communities in how to use ITNs.
Results
During a three-month period (July-September 2004), 38,600 ITNs were
distributed in 159 villages,
free of charge to children under five and
pregnant women, during the MDA process. About 148,000 persons
were treated with medicines for LF at the same time.
 |
Children
under five and pregnant women do not receive drugs against
lymphatic filariasis, but insecticide-treated bed nets
can protect them against both filariasis and malaria. (Courtesy
The Carter Center/A. Eigege) |
Preliminary data from an evaluation conducted eight months later showed
a nine-fold increase in ITN ownership among households with
a child under five or a pregnant woman, from 9 percent before
the distribution to 80 percent afterwards. The drug coverage for LF remained
as high as in years past (68 percent). Thus, the MDA rapidly
helped the malaria program reach high ITN coverage without adversely affecting
the drug distribution. This successful pilot strengthens findings from
other combined
health campaigns that ITN distribution can be successfully piggybacked
onto other health interventions. It shows, more specifically,
how two programs fighting two severe mosquito-borne diseases
can share their resources to achieve their goals faster, better, and
more cheaply.
This article contributed by the The
Carter Center.
* Drug brand names and manufacturers are mentioned for informational
purposes only and do not imply endorsement by CDC, the U.S.
Public Health Service, or the U.S. Department of Health and
Human Services.
Page last modified : August
18,
2005
Content source: Division of Parasitic Diseases
National Center for Zoonotic, Vector-Borne, and Enteric Diseases (ZVED)
|
 |
|