|
DOL Annual Report, Fiscal Year 2003
Outcome Goal 2.2
Protect Worker Benefits
Overview
DOL improves the economic security of America's working families through the administration of benefit programs dealing with unemployment insurance, expansion of private pension coverage, protection of Federal and certain other workers from the effects of work-related injuries and illness, and timely and uninterrupted payment of pension benefits. DOL's longstanding role in protecting worker benefits arose in response to specific concerns about the well-being of American workers and their families. The Department's Employment and Training Administration (ETA), Employee Benefits Security Administration (EBSA), Employment Standards Administration (ESA), and Pension Benefit Guaranty Corporation (PBGC) administer DOL programs that safeguard the economic security of the Nation's workers and retirees.
Serving The Public
The ETA-administered Unemployment Insurance (UI) program is a critical component of the Department's contribution to worker security. DOL provides administrative support to State-operated programs and maintains the Unemployment Trust Fund that serves as a buffer to volatile cycles in tax revenues and benefit claims. In FY 2003, system efficiency improved even as workloads increased, thanks in part to technical assistance provided by DOL.
The Employee Benefits Security Administration (EBSA) is responsible for the administration and enforcement of Title I of the Employee Retirement Income Security Act of 1974, as amended (ERISA), in both civil and criminal areas. EBSA currently oversees approximately 730,000 private pension plans and millions of private health and welfare plans that are subject to ERISA. The pension plans under our jurisdiction hold over $4 trillion in assets and cover approximately 150 million Americans. To achieve the Secretary's strategic goal of retirement security for the nation's workers and retirees, EBSA employs a comprehensive, integrated strategy encompassing programs for enforcement, participant assistance, compliance assistance, interpretive guidance, legislation and research. In FY 2003, the Department obtained monetary results of over $1 billion as a result of its investigative and participant assistance activities a record year.
ESA's Office of Workers' Compensation Programs (OWCP) administers four disability compensation programs that minimize the human, social, and financial burden on certain workers or their dependents or survivors resulting from work-related injury, disease, or death. OWCP accomplishes this through the provision of wage replacement and cash benefits, medical treatment, vocational rehabilitation, and other benefits. In FY 2003, case management and vocational rehabilitation services provided by the Federal Employees' Compensation program assisted more workers in returning to employment and shortened the average duration of paid disability for new cases. Administration of the Energy Employees Occupational Illness Compensation program continues to improve the timeliness of completing initial claims processing and issuing final decisions.
PBGC restores pension benefits to participants in defined benefit plans that have been terminated, usually due to the sponsoring employer's bankruptcy. Estimated benefits are paid to eligible retired participants while awaiting issuance of a final benefit determination. In the last five years, PBGC has cut in half the time it takes to complete benefit determinations. Over 83,000 participants received final determinations of their benefits in FY 2003, while another (record) 206,000 participants had their plans trusted by PBGC.
Program Costs
FY 2003 program costs of $57.7 billion supported ETA's unemployment insurance and foreign labor certification programs, EBSA efforts to ensure that individuals receive promised benefits, and ESA programs to reduce the consequences of work-related injuries.
Unemployment Insurance program costs, which rose by $2.5 billion over FY 2002, accounted for 98 percent of FY 2003 expenditures. UI Program costs are largely driven by average weekly insured unemployment (AWIU) - the average number of people filing claims for continuing UI benefits each week. The trend line in the chart shows the effect of changes in AWIU from FY 1999 to 2003 on program costs for Outcome Goal 2.2. The AWIU figure increased from 2.258 million in FY 1999 to an estimated 3.560 million in FY 2003. UI benefits paid increased from $20.9 billion in FY 1999 to an estimated $53.4 billion in FY 2003.
Other costs declined or rose minimally. For example, ESA's cost of providing assistance to Federal employees injured on the job fell from $1.35 billion to $1.06 billion. EBSA's costs of protecting health and retirement benefits went up, but only slightly; while the agency's share of total outcome goal costs rose from $42 million in FY 2002 to $146 million in FY 2003, almost all of the increase is due to transfer of its largest programs from Outcome Goal 2.1. PBGC is not included in the DOL Consolidated Statement of Net Costs, hence the costs of its programs are not reflected here.
DOL Challenges for the Future
Emerging workforce trends present a variety of challenges to the Department's goal of creating economic security for workers and their families. Protecting vulnerable populations and protecting and expanding pension and health care coverage will continue to be key issues on the planning horizon. These structural changes are not expected to remove or lessen workers' risk of experiencing unemployment in our dynamic market economy. The unemployment insurance system must therefore continue to adapt to the changing character of the workforce, the job market, and the nature of unemployment itself.
Our Nation is expected to have an older and more highly educated workforce, increasing our need for reliance on foreign workers to fill employment needs in lower-skilled, low wage occupations. These populations of workers are more vulnerable to exploitation, and protecting these workers will continue to be a key focus of our efforts. As longevity increases, needs for health care will rise, as well. Employment benefit packages have evolved toward increasing employees' responsibility for their own retirement savings and planning. In the future, pension and health care benefits will need to be flexible and portable.
To help American workers remain secure as they adapt to these changes, the Department will increase its use of compliance assistance and refine its use of technology and targeting of enforcement efforts.
Pay Unemployment Insurance Claims Accurately and Promptly
| Vanessa, of Alpharetta, GA files her Unemployment Insurance claim at the North Metro Atlanta Career Center's intranet workstation. Since 2001, the Georgia Department of Labor's 53 Career Centers have offered UI claimants the option of filing for benefits on the Department's intranet. The service allows claimants to complete their application for benefits quickly and frees staff to assist those who need personal assistance. |
 |
| Photo Credit: Ed Hall; Georgia Department of Labor |
Performance Goal 2.2A (Employment and Training Administration) - FY 2003
Make timely and accurate benefit payments to unemployed workers, facilitate the reemployment of unemployed insurance claimants, and set up Unemployment Insurance (UI) tax accounts promptly for new employers.
Indicators
Payment Timeliness: 91 percent of all intrastate first payments will be made within 14/21 days. Payment Accuracy: Establish for recovery at least 59 percent of all estimated detectable overpayments.
Facilitate Reemployment: A data source will be selected and baseline for the entered employment rate of UI claimants will be established during early FY 2004.
Establish Tax Accounts Promptly: 80 percent of new employer status determinations will be made within 90 days of the end of the quarter in which liability occurred.
Results
The goal was substantially achieved; two targets were reached and two were substantially reached.
-
Payment Timeliness: This target was substantially reached. For the year ending June 30, 2003, 89 percent of first payments were made within three weeks, versus a target of 91 percent. Performance was up from FY 2002's 88.7 percent.
-
Payment Accuracy: This target was substantially reached. For the year ending June 30, 2003, States established for recovery 56.1 percent of the estimated amount of overpayments they could detect and recover, versus a target of 59 percent.
-
Facilitate Reemployment: This target was reached. During the year, DOL developed a measure and a method to obtain re-employment information on UI claimants. Six States are pilot-testing the method, and their results will be used to establish a baseline in early FY 2004.
-
Establish Tax Accounts Promptly: This target was reached. For the year ending June 30, 2003, 83.7 percent of determinations that established employers as newly liable for filing UI reports and paying UI taxes were made within 90 days of the end of the quarter they first became liable, exceeding the target of 80 percent.
Program Description
By temporarily replacing part of lost wage income, the Federal-State UI system-one of the nation's most successful and enduring Federal-State partnerships-ameliorates personal financial hardship due to unemployment and stabilizes the economy during economic downturns. For both workers and employers, the program's success depends upon: timely payment of benefits; prevention or prompt detection of erroneous payments; timely establishment of new employers' tax accounts to ensure the reporting of workers' wages and payment of taxes to fund benefits; and the promotion and facilitation of workers' return to suitable work. Targets were selected by first assessing prior experience, and then projecting reasonable performance under anticipated labor market conditions.
Analysis of Results
The UI system performed extremely well, considering that claims workloads were much higher than forecasted. The number of beneficiaries, at 10.3 million, was only slightly lower than the previous year's 10.5 million. Benefit payments totaled $53.4 billion, an increase of $2.5 billion from FY 2002. Despite this, States not only maintained first payment timeliness at a high level, but also improved it to 89 percent from 88.7 percent. The timeliness of new employer status determinations continued to improve; 83.7 percent were made within 90 days. The sluggish economy, which depresses creation of new businesses, may have contributed to the improved new status timeliness. The decline in detection and establishment of recoverable overpayments may be due to the rise in payment volume and workload. Six States are pilot-testing the method for measuring entered employment, and those results will permit establishment of a baseline in early FY 2004.
Strategies
Timely Payments: The Department will work intensively with States to improve payment timeliness. Fourteen States will prepare Corrective Action Plans (CAPs) for FY 2004 for failing to meet the Secretary's Standard criterion of 87 percent.
Detection of Overpayments: The Department has instituted several payment integrity initiatives as part of its integrity work plan; taken as a whole, they establish a structure that will improve payment integrity over time. The most important of these initiatives is promoting and funding States' use of their own State Directories of New Hires databases to detect claimants who continued to claim benefits, despite having returned to work. This enables States to detect these violations in time to reduce the number of weeks erroneously claimed and to enhance establishment and recovery of overpayments. The Department has also funded State data exchanges with the Social Security Administration and other State agencies to help prevent overpayments.
Establish Tax Accounts Promptly: In late FY 2003, DOL provided grants to six States for Internet employer registration systems that speed the process of establishing tax accounts. State administrators are cooperating with the Department on raising timeliness standards.
Management Issues
In its recent PART review of the UI program, the Administration concluded that the UI program has "relatively few areas of vulnerability"...indicating that the UI program overall continues to be managed effectively. They noted that DOL's Office of Inspector General (OIG) and the General Accounting Office (GAO) encouraged DOL to make a "more concerted effort" to reduce the overpayment rate, and that the Department has increased efforts in this area. They agreed with DOL that the UI program was making progress toward its long-term and annual performance goals, acknowledging the effect of heavy workload increases on attaining the goals.
The OIG again included concerns about UI integrity and solvency in its 2003 report of Top Management Challenges to the Department. It recommended training State staff in fraud detection and investigative techniques, and sharing information on multi-claimant fraud schemes and best practices. One of the vehicles used for this purpose was the national UI integrity conference conducted in April 2003. This conference also addressed topics directly related to the payment accuracy indicator, such as use of New Hires data mentioned above.
Two additional OIG reports address the issues of Internal Revenue Service (IRS) administrative charges to the Unemployment Trust Fund (UTF) (see study 3 in Appendix 3) and detection of UI claimant overpayments (see study 8 in Appendix 3). In response to OIG recommendations regarding the UTF, ETA is working with the IRS on its new financial accounting system and methodology that will allocate costs among the trust funds. A Memorandum of Agreement between ETA and IRS is being pursued in FY 2004. Regarding OIG recommendations on overpayments, ETA has made overpayments a top priority by establishing overpayment detection as a performance measure for which states will be held accountable, and by exploring use of New Hires data in reducing overpayments.
During FY 2003, States engaged in an intensive effort to implement the UI Data Validation system, which will help ensure the accuracy of most key performance data by validating over half of all reported data. All but eight States were able to begin implementation by the end of FY 2003.
The Department is also conducting a pilot project to test the impact of resource increases on performance. Information obtained will inform a strategy for building performance improvement incentives into the UI resource management system. At least five States will participate; results are expected by June 2004.
Goal Assessment and Future Plans
Based on its experience of the past two years, DOL proposes for FY 2004 the following adjustments to its performance targets. It proposes lowering the target for intrastate first payments made within three weeks from 91.3 percent to 89.2 percent. This target is higher than FY 2003 performance and reflects workload estimates based on the administration's economic assumptions. A general improvement in performance can be expected with improvements in the economy. Also consistent with those economic assumptions and based on recent experience, the Department proposes raising from 80 percent to 82.2 percent the target for determinations about new employers' liability for UI taxes within 90 days of the quarter when they first become liable. Although this is below FY 2003 performance, it reflects the counter-cyclical nature of this indicator. The Department proposes lowering the FY 2004 target for establishing overpayments from 59 percent of estimated detectable recoverable overpayments to 57 percent, based on the Administration's economic assumptions. Although cyclical factors will eventually help raise this performance, in FY 2003 those factors lowered performance to 56.1 percent by raising benefit payments and estimated overpayments faster than States could increase overpayment detection efforts.
| Protecting workers' retirement benefits: Secretary Elaine L Chao announces the filing of a suit to recover losses that Enron employees suffered due to the mismanagement of two of Enron's main pension plans. |
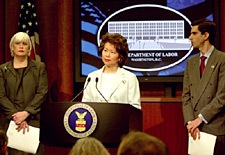 |
| Photo Credit: US DOL |
Provide for Secure Pension and Health Plans
Performance Goal 2.2B (Employee Benefits Security Administration) - FY 2003
Enhance pension and health benefits security
Indicators
Achieve greater than a 50 percent ratio of closed civil cases with corrected violations to civil closed cases.
Achieve greater than a 25 percent ratio of criminal cases referred for prosecution to total criminal cases.
Achieve a Customer Satisfaction Index of 59 (on a scale of 0 to 100), or comparable measurement, for participants and beneficiaries who have contacted EBSA for assistance.
Results
The goal was achieved. The Department achieved a civil ratio of 69 percent and a criminal ratio of 40 percent while receiving a customer satisfaction score of 59 percent.
Program Description
Integrity in the management and administration of pension and health funds is fundamental to the success of our voluntary employment-based benefits system. Participants in our voluntary benefits system trust that employers and plan officials will meet their responsibilities in the management of pension and health plans and expect the Government to enforce the law and take appropriate action against wrongdoers if they do not. The Employee Benefits Security Administration (EBSA) is responsible for enforcing the Employee Retirement Income Security Act (ERISA). Revelations of corporate and union malfeasance, combined with a quickly changing economy, have heightened American workers' and their families' concerns about health benefits and the security of their pensions. Our challenge is to maintain the trust and confidence in the employee benefits system by developing and implementing public programs that enhance the security of pension and health benefits. Achieving the targeted civil and criminal ratios is but one overarching performance measure that instills confidence that the Department is successfully targeting wrongdoers.
In addition to a proactive enforcement program, DOL combines an aggressive outreach and education program with a highly motivated and trained staff of customer assistance experts in the field of pension and health laws. By directly assisting plan participants and beneficiaries in understanding their rights and protecting their benefits, our education and customer assistance programs help to create knowledgeable consumers who can assist in monitoring their own benefit rights. DOL received over 170,000 written or telephone inquiries for assistance in FY 2003. Protecting workers' benefits requires a rapid and accurate response to customer inquiries, and the public's feedback and perception of our abilities, as described by The Gallup Organization's customer satisfaction survey, is therefore a meaningful measure of the Department's performance.
Analysis of Results
The Department measures the quality of its investigations by gauging the ratio of successful investigations to total investigations. A successful civil closed investigation is one in which rightful assets are protected or returned to plans and participants. A successful criminal investigation is one that is referred for prosecution. In FY 2003, the Department obtained monetary results of over $1 billion as a result of its investigative and participant assistance activities, a record year. Included in the above results is a single investigation that accounted for approximately $455 million in plan assets protected. Also included are enforcement referrals by the Benefits Advisors. Referrals led to 1,359 investigations being closed, resulting in $197 million in monetary results. Finally, Benefit Advisors recovered approximately $83 million on behalf of participants through informal resolution of benefit complaints- the highest amount ever recovered in a single year. Monetary results may fluctuate significantly and past performance cannot predict future performance in any given year, but monetary results have followed an upward trend over the past several years. During FY 2003, the Department investigated a number of high profile, resource intensive cases with far-reaching effects on the participant benefits community.
Benefit Advisors responded to 99.78 percent of all written inquiries within 30 days of receipt and responded to 99.95 percent of telephone inquiries by the close of the next business day. Our target to achieve a customer satisfaction score of 59% - the total percentage of the respondents who rated our overall services at least a 4 or 5 on a scale of 1 to 5 - was achieved. However, Gallup has advised EBSA that its long-term target to achieve a customer satisfaction goal of 75% by FY 2008 is unattainable based on their vast experience and other industry standards. Gallup has recommended that EBSA revise its long- term goal to a more realistic level. As Gallup continues to develop additional baseline data for government agencies, they will assist us in refining our future targets.
Strategies
During FY 2003, the Department continued to employ more effective targeting techniques to increase the number of cases converted from limited reviews to investigations in which possible fiduciary or criminal violations have been identified. These techniques aid in the Department's efforts to identify those cases which merit investigation. Examples of successful targeting techniques the Department uses include computer-aided analysis of data from reports that employee benefit plans and service providers are required to file with the Department, and working directly with financial institutions to assist them in identifying plans which may have a delinquent contribution problem or which responsible plan officials may have abandoned. In addition, the Department uses other strategies to improve its enforcement program, including sharing best practices and success stories from field investigations, and identifying quality cases and their sources through the Case Opening and Results Analysis.
The Department will continue the popular Retirement Savings Education Campaign and the Health Benefits Education Campaign; the Dislocated Worker Program; and participant assistance services that aid plan participants in understanding the employee benefits laws and procedures as well as help participants to obtain benefits that have been incorrectly withheld.
Management Issues
EBSA's Enforcement Management System (EMS) provides the data used to measure the enforcement ratios, and the Department has confidence in the accuracy and reliability of the data. EBSA's internal quality assurance processes require that individuals not directly involved with the investigation at hand or inputting data for the investigation approve all case openings. Cases with monetary results ultimately receive scrutiny throughout the management hierarchy up to and including national office oversight and review. In the participant assistance area, The Gallup Organization, an internationally renowned survey research firm, performed the customer satisfaction evaluation and provided the customer satisfaction score. EBSA has high confidence in the validity, reliability, and timeliness of the Gallup data.
External Evaluations and Audits: EBSA has implemented several ambitious initiatives that directly respond to recommendations from the the Administration's PART review. First, EBSA is making steady progress in its efforts, beginning in February 2003, to follow up on the FY 1995 study with respect to the quality of ERISA audits performed on pension plans to determine the level of compliance of the audits to professional accounting standards. Second, in FY 2004, EBSA will be conducting a baseline compliance study with respect to certain aspects of employee contribution plans. Third, EBSA will be receiving reports from The Gallup Organization and Mathematica Policy Research during the first quarter of FY 2004 for evaluation activities conducted during FY 2003 in its participant assistance and enforcement programs. EBSA has also been selected to receive funding during FY 2004 to conduct additional evaluation activities in its participant assistance program. Finally, EBSA is establishing a regulatory review program that will: (a) set forth a process for identifying initiatives for review, (b) provide for the evaluation of cost and benefits of identified regulations and exemptions; and (c) to the extent legally permissible, modify or eliminate those rules for which the costs and administrative burdens outweigh the benefits.
Goal Assessment and Future Plans
Developing a quantifiable, pure outcome goal to measure EBSA's success is extremely challenging. Externalities, such as the economy and tax policy, have a significant impact on whether employers opt to offer benefits and whether employees choose to participate and to what extent. In addition, EBSA oversees benefit security for approximately 6 million plans, 150 million participants and beneficiaries, and approximately $4.8 trillion in assets. EBSA strives to ensure that stakeholders (professional planners and participants) are empowered with knowledge to comply with the law and to make informed personal choices.
In the absence of having a pure outcome measure, describing success in enhancing the security of retirement benefits in this complex environment involves selecting key measures that provide an indication of or reasonable connection to our success. It is within this context that the Department will continue to utilize the performance indices we developed and implemented for the first time in FY 2003. With respect to the customer satisfaction target, EBSA will work with Gallup to refine its long-term target consistent with other industry standards and experience.
In developing these measures, EBSA intends to: (1) maintain maximum flexibility for the Secretary to make policy judgments regarding enforcement, compliance assistance, outreach and education; (2) demonstrate effectiveness in achieving these policy choices; (3) avoid creating unintended incentives (i.e. selecting monetary measures that might lead the Department to select investigations based on potential recovery alone and thus ignore small plans or health plan violations); and (4) measure a multitude of diverse activities (e.g. education/outreach, technical assistance, enforcement). By measuring these indices, coupled with additional statistical and internal management information, the effectiveness of our program can be determined and more importantly, we can develop strategies to more effectively enhance benefit and retirement security.
Reduce the Consequences of Work-Related Injuries
Performance Goal 2.2 C (Employment Standards Administration) - FY 2003
Minimize the human, social, and financial impact of work-related injuries for workers and their families.
Results
This goal was substantially achieved. Targets were reached for eight of 10 indicators.
Program Description
Employment Standards Administration's (ESA) Office of Workers' Compensation Programs (OWCP) administers four disability compensation programs that provide benefits to certain workers who experience work-related injury or disease, and survivors of employees who die from job-related injury or disease:
-
The Federal Employees' Compensation Act (FECA) program affords income and medical cost protection to civilian Federal Government employees and certain other groups.
-
The Longshore and Harbor Workers' Compensation Act program provides similar protection to private- sector workers engaged in certain maritime and related employment.
-
The Black Lung Benefits program provides protection to the nation's coal miners suffering from totally disabling pneumoconiosis.
-
The Energy Employees Occupational Illness Compensation Program Act of 2000 provides compensation and medical benefits to employees or survivors of employees of the Department of Energy (DOE) and of private companies under contract with DOE who suffer from a radiation-related cancer, beryllium-related disease, or chronic silicosis due to their work producing or testing nuclear weapons. DOL coordinates this program with DOE, the Department of Health and Human Services (HHS), and the Department of Justice.
Results, Strategies and Future Plans for each indicator are presented separately.
1. For FECA cases of the United States Postal Service, reduce the lost production days rate (LPD per 100 employees) by one percent from the FY 2002 baseline.
Results
The target of 129.7 days was not reached. LPD rose by nine percent to 143.3 days in FY 2003. Roughly half of the annual total of over two million LPD days for Federal employees is attributable to US Postal Service cases. The number of USPS wage-loss claims continues to increase. Employment reductions have resulted in losses in light-duty and other reemployment opportunities for injured Postal workers.
Strategies
To return more employees to work, ESA is improving Vocational Rehabilitation strategies, including increasing the number of placements with new employers and particularly focusing on Postal Service cases.
2. For FECA cases of All Other Government Agencies, reduce the lost production days rate (LPD per 100 employees) by three percent from the FY 2001 baseline.
Results
The target for this indicator was not reached. In FY 2003, LPD for All Other Government Agencies rose by 2.6 percent to 55.2 days. The increase in LPD reflects an increase in non-Postal Federal employment, particularly in the security field, exposing additional workers to potential injuries; an increase in new FECA injury claims of 6 percent over FY 2002; continuing increases in the number of wage-loss (severe) claims (up 30 percent since FY 2000); and, significantly, an increase of 22 percent in total disability days during the continuation-of-pay period (immediately following injury and before OWCP takes jurisdiction over the case).
Despite these negative external factors, the total increase in LPD was kept modest by efforts to manage FECA wage-loss claims. Through FECA's Quality Case Management (QCM) program, average time loss in those cases was reduced to 162 days per case, a reduction of an average of 27 wage-loss days since 1997, saving $26 million in annual compensation costs for affected cases.
Strategies
Under the QCM strategy, ESA assigns nurses to new injury cases to facilitate communications between the physician, the injured employee and the employer. Nurses screen cases for appropriateness of medical and pharmacological treatment, and encourage injured workers to recover and return to work.
Future Plans
DOL's OSHA and ESA are reinvigorating their joint program to improve Federal workplace safety, facilitate recovery, and promote speedy returns to work. This effort will better publicize and focus Federal employers on workplace injuries, set government-wide performance goals, and track and report results. DOL is also exploring ways to provide more timely data and assist Federal employers in interpreting injury and time loss results.
3. Increase FECA Vocational Rehabilitation placements with new employers for injured USPS employees by five percent over FY 2002.
Results
The target was reached. This was a new indicator for FY 2003. Performance exceeded expectations with an increase of 14 percent (to 56 placements) despite a slow start-up and lengthy required lead times.
Strategies
DOL seeks increases in new employer placements, since light duty and other reemployment opportunities have decreased within the Postal Service. DOL will expand outreach to employers to target occupational or skills types and teaming employers to identify cross-agency opportunities.
Future Plans
The FY 2004 target is to increase new employer placements of USPS employees by 15 percent over baseline.
4. Through use of Periodic Roll Management, produce $20 million in first-year savings in the FECA program.
Results
The target was reached. Disability status reviews improved services to disabled beneficiaries, resulting in first-year savings of $24.6 million.
Strategies
Future PRM reviews will focus on newer disability cases and continue addressing those cases with significant potential for vocational rehabilitation services.
Future Plans
The FY 2004 goal is to produce $18 million in first-year savings.
5. The trend in the indexed cost per case of FECA cases receiving medical treatment will remain below the comparable measure for nationwide health care costs.
Results
The target was reached. In the last 12 months, FECA average medical treatment case costs remained stable, while the Milliman Health Cost Index (MHCI) rose by 10 percent. This indicator assesses whether FECA program costs are comparable to nationwide health care cost trends as measured by MHCI. Since FY 2000, nationwide costs have risen 36 percent on average, while FECA average costs have only risen 19 percent, due to several successful cost containment strategies.
Strategies
Because early FY 2001, implementation of various cost containment strategies has significantly moved FECA's cost curve well below the average Milliman Index.
Future Plans
Since average medical costs continue to rise, DOL will continue implementing new cost containment strategies.
6. Establish or complete baselines in Key customer service areas.
Results
The target was reached. ESA established baselines for five communications performance indicators measuring availability, access, responsiveness, effectiveness, and quality:
-
Increase use of FECA program electronic services
-
Reduce average caller wait times
-
Reduce average time to return calls
-
Increase calls resolved on the first try
-
Increase calls handled according to program quality standards
| On April 23, 2003, Deputy Secretary of Labor D. Cameron Findlay (pictured below) and Deputy Secretary of Energy Kyle McSlarrow presented one of the first checks for a dose reconstructed claim in the amount of $150,000 to Thomas, who worked at Hanford as a chemical operator from 1947-1982. The radiation dose estimate produced by the dose reconstruction process validated the probability that the exposure to radiation experienced on the job caused Thomas' cancer. "Today's event is a symbol of our commitment to people like Thomas who worked for years on behalf of our country," said Deputy Secretary of Labor Findlay. |
 |
| Photo Credit: US DOL |
Strategies
ESA seeks to increase FECA program customer satisfaction by producing better results in communications services. ESA will develop and train FECA phone bank personnel in professional techniques, standardize call-handling procedures, add desk-top tools for call handlers, and monitor call quality.
Future Plans
ESA plans incremental improvements in each of the five communication indicators to achieve optimally effective levels by FY 2008.
7. Reduce by two percent over the FY 2002 baseline the average time required to resolve disputed issues in Longshore and Harbor Workers' Compensation Program contested cases.
Results
The target was reached. For FY 2003, the average number of days to resolve disputed issues was 266 days, thirteen days below the target of 279 days. This indicator assesses the speedy resolution of disputed issues, enabling earlier benefit delivery and reducing litigation costs. ESA revised last year's baseline and reset the FY 2003 target.
Strategies
The Longshore program has instituted reforms focusing on timeliness objectives, improving amicability in contested case proceedings, ensuring proper data collection and reporting, and improving communications and outreach to injured workers, employers and insurers.
Future Plans
Although results well exceeded target in FY 2003, we continue to project average resolution time reductions from the baseline of two percent annually. Because this is a relatively new performance indicator, we will continue to carefully monitor the performance trend and adjust out-year targets as appropriate.
8. Increase by four percent over the FY 2001 established baseline the percentage of Black Lung benefit claims filed under the revised regulations for which, following an eligibility decision by the district director, there are no requests for further action from any party pending one year after receipt of the claim.
Results
This target was reached. 86.6 percent of claims subject to the new regulations had no pending requests for further action one year after receipt of claim. Target performance was 70.5 percent. Revised regulations, effective in 2001, were implemented and the program increased the number of stakeholders who decided not to pursue the claim further after accepting the district director's eligibility decision.
Strategies
Strategies include outreach and technical assistance with stakeholder communities, work with Black Lung's authorized diagnostic provider community to emphasize the need for complete and accurate medical reports, improving data access, providing new controls that ensure correct payments, evaluating service delivery to maintain timeliness and quality standards, and training staff. ESA will revisit its performance targets for to ensure that they remain challenging.
Future Plans
These extraordinary results were due largely to factors that will diminish greatly in FY 2004. Cohorts of re-filed and marginal cases subsequently withdrawn during the initial processing period under the revised regulations should decrease or disappear during FY 2004 and beyond. The reduction or elimination of these cohorts will bring performance in line with projected targets.
9. 75 percent of Initial Claims for benefits in the Energy Program are processed within standard timeframes.
Results
This target was reached. Seventy nine percent of initial Claims for benefits in the Energy Program were processed within standard timeframes. Program evaluations and workload adjustments implemented in response to performance lessons learned in FY 2002 contributed to achievement of this goal in FY 2003.
Strategies
The Division of Energy Employees Occupational Illness Compensation (DEEOIC) will transition to the OWCP Medical Bill Processing System, conduct extensive outreach to reach additional potential claimants, and establish improved methodologies for distributing workloads created by dose reconstructions returned from the National Institute of Occupational Safety and Health (NIOSH). DOL will also offer claimants the option to transmit forms electronically.
Future Plans
Although ESA exceeded its FY 2003 target, ESA will retain the target to improve claims processing time by two percent annually. In FY 2004 ESA anticipates an increased workload based on a large volume of dose reconstruction cases and new claims resulting from increased outreach activities to potential claimants.
10. 75 percent of Final Decisions in the Energy Program are processed within standard timeframes.
Results
This target was reached, with an overall performance result of 76 percent. Performance against this indicator reflects prompt handling of uncontested cases (including payment of approved cases), and timely provisions of appeal decisions. The program anticipates a much larger volume of appeals in future years.
Strategies
ESA continually monitors and assesses its processes for issuing final decisions, including reviews of the written record and formal hearings, and will continue to prioritize case handling and enhance the process of issuing formal denials of specific medical bills.
Future Plans
DEEOIC's FY 2004 goal is to increase performance to 77 percent. More appellate process resources will be devoted to address NIOSH's increasing volumes of dose reconstruction cases. ESA will continue developing automated tools to enhance decision quality and timeliness, benefit delivery and case management, and provide information to the public.
Management Issues
Data: ESA performance data are extracted from the automated case management or benefit payment systems of the four individual disability programs. Production quality information is derived from internal managerial accountability audits or other performance reviews. Injury time-loss data is also obtained from Federal employers and national medical cost data, from Milliman, USA, an independent consultant and actuarial firm. Federal employing agencies derive their data from multiple data systems, and although the Department specifies the type of data required, DOL has no oversight over these data systems.
Performance data are compiled in separate operations within OWCP and distributed to field managers and national office reviewers. Senior managers review final performance reports for issuance in formal reporting. DOL maintains strict management oversight and control of the data entry process, including regular on-site review by district directors to ensure data accuracy, and periodic accountability and management reviews that sample and assess data quality and accuracy.
Management Challenges: In the FECA program, DOL must find ways to better enlist Federal employers to play a greater role in reducing injuries and lessening their severity, report new injuries more quickly, better assist claimants immediately following injury, and improve return-to-work opportunities.
Economic trends, workplace modernization, and restructuring are changing the types of new injuries incurred and are reducing the number of Federal jobs available to recovering injured workers. The modern workplace demands that workers retrain and upgrade skills, and the average age of Federal workers is rising, all factors making return-to-work and time loss reduction more challenging for the FECA program.
Customer demands continue to challenge FECA's processing capabilities. The program handles over 5.5 million pieces of mail and approximately three million telephone calls, faxes, and e-mails annually.
In both the Longshore and Black Lung programs, customer/stakeholder attitudes regarding fairness continue to be a challenge. These programs strive to provide clear and balanced recommendations and decisions in accordance with existing law. However, people who do not receive the desired outcome may feel that the resolution is not fair.
The relatively new Energy Program will continue to experience near-term and hard-to-predict workload fluctuations. The complexity of the authorizing statute and the DOE nuclear weapons industry, and the difficulty identifying potential claimants intensify these challenges. DOL coordinates basic claims activities with three other Cabinet-level departments, and works with these departments to alleviate potential workload imbalances and inefficiencies in claims processing.
External Program Evaluations and Audits: The FECA Program Assessment Rating Tool (PART) review finds that FECA has clear, ambitious, outcome-oriented goals, and low erroneous payments. The program was also recognized for its progress in containing medical costs. However, the PART also noted that FECA does not have cost-effectiveness measures or goals.
The Department has initiated several reforms:
- Re-proposing legislation to update the benefit structure, improve benefit equity, and adopt best practices of state workers' compensation systems;
- Undertaking an evaluation of FECA's disability management and wage-loss compensation payment strategies and reviewing State/industry best practices.
- Exploring the efficacy of cost-effectiveness performance goals, and developing a cost-accounting system.
- Developing a customer service performance goal focused on FECA communications.
Provide Accurate and Timely Benefit Payments
Performance Goal 2.2D (Pension Benefit Guaranty Corporation) - FY 2003
PBGC will provide accurate and timely payments to the beneficiaries and businesses it serves.
Indicators
Reducing to 3.0 years the average timeframe to send benefit determinations to participants in defined benefit pension plans taken over by PBGC.
Minimizing the number of erroneous benefit payments.
Refunding pension insurance premium overpayments to businesses within 90 days of a request.
Results
The goal was substantially achieved. PBGC reduced to 2.2 years the average timeframe to send benefit determinations to participants in defined benefit pension plans taken over by PBGC. Based on a review of benefit payment determinations, PBGC was able to issue a Statement of Reasonable Assurance of Accuracy, which reports findings of the audit of benefit determinations conducted. PBGC improved on the FY 2002 rate on insurance premium overpayments to businesses within 90 days of a request by refunding 82 percent within 90 days in FY 2003. This fell short of PBGC's target of 85 percent.
Program Description
The Secretary of Labor serves as Chairman of the Board of the Pension Benefit Guaranty Corporation, which provides timely and uninterrupted payment of pension benefits to participants whose defined benefit pension plans were terminated. Plan termination most frequently results from the sponsoring employer's bankruptcy. Benefit determinations tell participants in plans for which PBGC has become the trustee what pension benefits they will receive. PBGC pays estimated benefits to all eligible participants retiring prior to the issuance of a benefit determination, thus ensuring that retirees receive their benefits when due and without interruption.
Analysis of Results
For indicator (1) of this goal, 2.2 years represents the average lapsed time to provide plan participants with final benefit determinations, surpassing the three-year target. This is the shortest benefit determination time period reported in PBGC history and is part of a continuing trend. As the chart indicates, over the last five years PBGC has cut in half the time it takes to complete benefit determinations. Over 83,000 participants were issued benefit determinations during 2003. The Corporation achieved this milestone while managing a record intake of 206,000 participants in newly trusteed plans. For indicator (2), to monitor the accuracy of benefit determinations, PBGC has instituted a formal internal review program. This review supports the PBGC issuance of a Statement of Reasonable Assurance of Accuracy that benefit determinations issued during this period are accurate.
For indicator (3), PBGC refunded 82 percent of pension insurance premium overpayments to businesses within 90 days of a request, against a target of 85 percent, and as compared to the FY 2002 rate of 41 percent.
Strategies
To further accelerate the benefit determination process, PBGC is implementing a Knowledge Management Portfolio. This tool provides the ability to capture electronically best practice scenarios, information, and discussion for on-demand use by staff with benefit processing responsibility. This will result in short-term and long-term business process improvements, further reducing benefit determination processing time. Also, legislative changes under consideration will result in a more simplified benefit valuation process and further reduce benefit determination processing time.
PBGC has developed a system of tighter management controls and reports that will enable it to accelerate premium refund processing. PBGC will develop and test a redesigned Premium Accounting System to provide more accurate and timely financial information. This new system, to be implemented in FY 2005, will support more accurate processing of premium payments and premium refunds, and will complement online premium filing. As a result, the new system will further the President's Management Agenda goal to improve financial performance and shorten the year-end closing cycle.
Management Issues
For indicators (1) and (2), data are collected from the Participant Record Information System Management (PRISM). For indicator (3), data are collected from the Premium Accounting System (used to determine the refund) and the Performance Accounting System (used to issue the refund). All are internal systems, subject to rigorous internal controls and audit by PBGC's Inspector General.
As mentioned above, PBGC continues to face an unprecedented influx of terminated plans. Meanwhile, participants' and practitioners' expectations for speed and accuracy of services continue to rise, specifically in the demand for electronic transactions and information.
In FY 2003, PBGC conducted its own internal Program Assessment Rating Tool (PART) review, which addressed the effectiveness of strategies and reliability of performance data pertaining to the performance goal.
Goal Assessment and Future Plans
For FY 2004 and beyond, PBGC has revised its outcome goals to align with its two lines of business: pension insurance and plan termination. PBGC will improve its customer satisfaction, as measured by the American Customer Satisfaction Index (ACSI) for pension plan practitioners to 78 percent by FY 2008 (71 percent in FY 2004), and its ACSI for participants in trusteed plans to 80 percent by FY 2008 (77 percent in FY 2004).
|



