
|
Physical Activity Guidelines Advisory Committee Report
Part G. Section 11: Understudied Populations
List of Figures
List of Tables
Introduction
The charge to the Physical Activity Guidelines Advisory Committee
(PAGAC) was to review existing scientific literature to identify where
sufficient evidence exists to develop comprehensive public health physical
activity recommendations for all Americans and to target them as necessary for
specific segments of the population. The higher levels of chronic disease risk
and burden in racial/ethnic and/or lower socioeconomic status (SES)
communities, and the growing cultural diversity of the United States, make
these population segments a priority in considering such targeting. The primary
focus of the PAGAC scientific review was research on primary prevention and
health/fitness promotion, not research on the delivery of exercise as a therapy
or treatment for specific disease conditions (e.g., physical therapy for
musculoskeletal disease or injury, cardiac rehabilitation). However, the PAGAC
recognized that many of the health benefits of physical activity for the
general population also pertained to many people who have some health condition
that typically excludes them from physical activity and health research.
Included in these populations are people with various disabilities, women
during pregnancy and the postpartum period, and races and ethnicities other
than non-Hispanic whites. Therefore, the PAGAC decided to conduct a separate
review of the scientific literature focusing on these three populations.
The first part of this chapter reviews the science published since
1995 evaluating the general health and fitness benefits of increased activity
in persons with selected physical and cognitive disabilities. The second part
provides a brief review of the science regarding physical activity performed by
women during pregnancy and the postpartum period. The last section provides an
overview of the science addressing the question, "Is there evidence that the
physical activity dose for improving health and fitness should differ for
people depending upon race or ethnicity?" Each PAGAC subcommittee was asked to
consider this question in its review of the literature, but committee members
agreed that it would help in better understanding this issue if the available
evidence was summarized in this section of the report.
Review of the Science: Health Outcomes
Associated With Physical Activity in People With Disabilities
Introduction
The lack of participation in beneficial physical activity is a serious
public health concern for all Americans, but it is even more acute for people
with disabilities, who are demonstrably at much greater risk of developing the
types of serious health problems associated with a sedentary lifestyle.
Healthy People 2010 outlines current levels of physical activity and
exercise for various subpopulations in the United States based on
cross-sectional surveys, as well as goals for the year 2010 (1). As shown in Table G11.1,
individuals with disabilities are currently much less active than their
non-disabled counterparts and participate in less regular and less vigorous
physical activity. They also report substantially more secondary conditions
that are directly or indirectly associated with their disability but are
considered preventable (e.g., fatigue, weight gain, deconditioning, pain) (2).
Table G11.1. Healthy People 2010 (HP 2010)
Goals for Increasing Physical Activity in Adults
|
With Disabilities |
Without Disabilities |
HP 2010 Target |
| No leisure-time physical activity |
56% |
36% |
20% |
| 30 Minutes activity 5+ days per week |
12% |
16% |
30% |
| 20 Minutes vigorous physical activity for cardiorespiratory
fitness 3+ days per week |
13% |
25% |
30% |
Patterns of low physical activity reported
among people with disabilities raise serious concern about their health and
well being, particularly as they enter their later years, when the effects of
the natural aging process are compounded by years of sedentary living and
severe deconditioning (3). Although substantial public
health initiatives strive to prevent disease, injury, and disability,
a growing recognition among public policy experts is the need to address people
with disabilities as a target population who can benefit from health promotion
activities, including increased participation in physical activity (4;5). Recognizing that people with
disabilities are less physically active than the general population (6;7), have poorer health status (8), and in particular, are more likely to experience chronic
and secondary conditions such as obesity, pain, fatigue, and depression (2), an examination of the existing evidence associated with
the effects of physical activity in people with disabilities is urgently needed
(9). A first step in this process is to (a) determine
whether people with disabilities receive similar cardiovascular,
musculoskeletal , metabolic, mental and functional health benefits as people
without disabilities, and (b) understand if these benefits outweigh the risks
of physical activity in these populations.
Overview of the Questions Asked
Eight categories of physical disability, 3 categories of cognitive
disability, and 1 group of combined disabilities are the focus of this review
(Table G11.2). These groups were selected because
of the higher volume of research identified on these populations compared to
other groups, such as spina bifida and polio, where very few research studies
were identified.
Table G11.2. Categories of
Disability
| Physical Disabilities |
Cognitive Disabilities |
Combined Disabilities |
- Lower limb loss
- Cerebral palsy
- Multiple sclerosis
- Muscular dystrophy
- Parkinson's disease
- Spinal cord injury
- Stroke
- Traumatic brain injury
|
- Alzheimer's disease
- Intellectual disability including Down syndrome
- Mental illness
|
- Two or more disability groups in same study
|
For these categories, the following questions were asked:
- What is the evidence that physical
activity improves cardiorespiratory fitness in people with
disabilities?
- What is the evidence that physical
activity improves lipid profiles in people with disabilities?
- What is the evidence that physical
activity improves musculoskeletal health in people with disabilities?
- What is the evidence that physical
activity improves functional health in people with disabilities?
- What is the evidence that physical
activity reduces secondary conditions in people with disabilities?
- What is the evidence that physical
activity helps maintain healthy weight and improves metabolic health in people
with disabilities?
- What is the evidence that physical
activity improves mental health in people with disabilities?
Following these discussions, the chapter addresses the safety concerns
and complications associated with physical activity in people with physical and
cognitive disabilities.
Data Sources and Process Used To Answer
Questions
The Physical Activity Guidelines for Americans Scientific
Database (see Part F: Scientific
Literature Database Methodology for a detailed description of
the Database and its development) included only a few manuscripts that
evaluated the effects in populations with disabilities. Thus, a comprehensive
literature review was conducted using the MEDLINE and CINAHL databases. Two
abstractors combined several keywords associated with disability and physical
activity or exercise. Reference lists in each individual article were also
reviewed for additional articles, including meta-analytic articles and
systematic review articles. The articles were included if they met the
following inclusion criteria:
- Written in English;
- Publication date between January 1995 and November 2007;
- Subjects had one of the 11 disabilities listed in
Table G11.2;
- Physical activity was the primary exposure variable;
- Covered the health outcomes listed in the preceding questions;
and
- Peer-reviewed.
Studies were excluded if they: (1) involved therapeutic exercise
modalities available primarily at a medical facility, such as body weight
supported treadmill training or functional electrical stimulation, as the main
exposure variable; (2) used single bouts of exercise; or (3) were conducted
using qualitative methods or case study.
Each of the identified studies was classified into 3 types of study
design: Randomized controlled trial (RCT), non-randomized trial with control
group, and pre/post-test with no control group. RCT is listed as the highest
level of evidence; non-randomized trials with a control group as middle level
of evidence; and pre/post designs with no control group as the lowest level of
evidence (10). No cross-sectional, retrospective
observational, or prospective observational studies were included in the
review.
Data Extraction
A total of 139 articles published between 1995 and 2007 and that met
all inclusion criteria were identified and reviewed for this report. Data were
independently extracted by 2 reviewers who have backgrounds in disability and
rehabilitation using the following categories:
- Participants/Subjects: Number recruited; number
analyzed; age; disability type; disability characteristics; number of years of
disability before intervention.
- Interventions: Type of training (i.e., aerobic,
strength, flexibility); exercise mode; training frequency; training duration;
length of intervention; program progression; attendance and/or compliance;
description of control condition.
- Setting: Supervised or unsupervised; home or
community.
- Outcome Measures: Health outcomes associated with
the intervention and divided into six categories: cardiorespiratory,
musculoskeletal , metabolic including body weight, mental, functional, and
secondary conditions.
Figure G11.1 illustrates the number and
design type of reviewed trials by disability group. Trials investigating the
effects of exercise on people with Stroke had the most number of
intervention-related exercise articles (n=23), while lower limb loss had the
lowest number of identified articles (n=2).
Types of Evidence
The type of available evidence used in this report to determine the
effects of exercise on health outcomes in people with physical or cognitive
disabilities was based on a modification of the criteria used by the US Agency
for Healthcare Research and Quality (AHRQ, formerly known as the US Agency for
Health Care Policy and Research) (11). We did not review
the quality of each study (i.e., power, intent-to-treat , different testers on
pre/post outcomes, etc.) as recommended by AHRQ and we also changed the
categories of evidence to parallel the work of the Committee. Non-randomized
trials were collapsed under the category of Pre/Post Studies with no Control
Group (i.e., Non-RCT).
Level of Evidence
Type 1: Two or more RCTs with positive results and no
studies reported significant negative effects.
Type 2a: One RCT with positive results and no studies
reported significant negative effects.
Type 2b: At least one Non-RCT with positive results
and no studies with significant negative effects.
Type 3a: Well designed prospective cohort studies and
case-control studies.
Type 3b: Other observational studies – weak
prospective cohort studies or case-control studies; cross-sectional studies or
case series.
Type 4: Non-significant findings or no studies
investigating the effects of exercise on people with disabilities.
Figure G11.1. Number of Articles
Identified by Disability Group and Design (N=139)
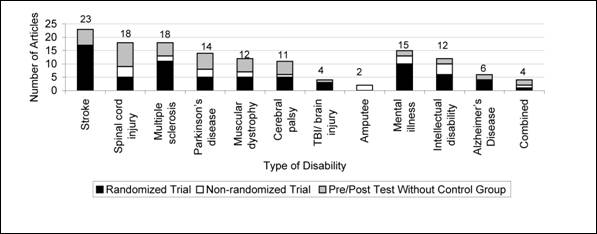
Figure G11.1. Data Points
| Categories |
Type of Disability |
Randomized Trial |
Non-Randomized Trial |
Pre/Post Test
Without Control
Group |
| Neuromuscular |
Stroke |
17 |
0 |
6 |
| Neuromuscular |
Spinal cord injury |
5 |
4 |
9 |
| Neuromuscular |
Multiple sclerosis |
11 |
2 |
5 |
| Neuromuscular |
Parkinson's disease |
5 |
3 |
6 |
| Neuromuscular |
Muscular dystrophy |
5 |
2 |
5 |
| Neuromuscular |
Cerebral palsy |
5 |
1 |
5 |
| Neuromuscular |
TBI/brain injury |
3 |
0 |
1 |
| Neuromuscular |
Amputee |
0 |
2 |
0 |
| Cognitive |
Mental illness |
10 |
3 |
2 |
| Cognitive |
Intellectual disability |
6 |
4 |
2 |
| Cognitive |
Alzheimer's Disease |
4 |
0 |
2 |
| Mixed |
Combined |
1 |
1 |
2 |
| Total |
– |
72 |
22 |
45 |
Question 1. What Is the Evidence That
Physical Activity Improves Cardiorespiratory Fitness in People With
Disabilities?
Conclusions
Type 1 evidence indicates that cardiorespiratory fitness can be
improved in people with Lower Limb Loss, Multiple Sclerosis, Spinal Cord
Injury, Stroke, and Mental Illness. Type 2a evidence provides the same findings
for people with Traumatic Brain Injury and Intellectual Disability, type 2b
evidence provides these findings in persons with Cerebral Palsy, Muscular
Dystrophy, and Alzheimer's Disease, and type 4 is indicative of no data or
non-significant findings on Parkinson's Disease. Overall, the evidence is
highly supportive of the use of physical activity in improving
cardiorespiratory fitness among people with physical and cognitive
disabilities.
Rationale
Twenty-one RCTs targeted improvements in cardiorespiratory fitness in
persons with physical and cognitive disabilities (Table G11.3). Of these 21 RCTs, 18 (86%) reported
significant favorable cardiorespiratory fitness outcomes. Of 25 non-RCTs, 21
(84%) reported significant favorable cardiorespiratory fitness outcomes.
Table G11.3. Physical Activity and
Cardiorespiratory Fitness in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical:Lower Limb Loss |
2(12;13) |
– |
– |
– |
● |
– |
– |
– |
| Physical: Cerebral Palsy |
– |
– |
1(14) |
– |
– |
– |
● |
– |
| Physical: Multiple Sclerosis |
4(15-18) |
1(19) |
1(20) |
1(21) |
● |
– |
– |
– |
| Physical: Muscular Dystrophy |
– |
– |
4(22-25) |
1(26) |
– |
– |
● |
– |
| Physical: Parkinson's Disease |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Spinal Cord Injury |
2(27;28) |
– |
7(29-35) |
2(36;37) |
● |
– |
– |
– |
| Physical: Stroke |
6(38-43) |
– |
1(44) |
– |
● |
– |
– |
– |
| Physical: Traumatic Brain
Injury |
1(45) |
– |
1(46) |
– |
– |
● |
– |
– |
| Cognitive: Alzheimer's Disease |
– |
– |
2(47;48) |
– |
– |
– |
● |
– |
| Cognitive: Intellectual
Disability |
1(49) |
1(50) |
2(51;52) |
– |
– |
● |
– |
– |
| Cognitive: Mental Illness |
2(53;54) |
1(55) |
– |
– |
● |
– |
– |
– |
| Combined |
– |
– |
2(56;57) |
– |
– |
– |
● |
– |
a S, Significant findings; b NS,
Non-significant findings; c Major depression disorder
Question 2. What Is the Evidence That
Physical Activity Improves Lipid Profiles in People With Disabilities?
Conclusions
The evidence on the use of physical activity for cardiovascular risk
reduction is less clear than it is for cardiorespiratory fitness. Two RCTs and
2 non-RCTs reported significant reductions in total cholesterol and
triglycerides, and two non-RCTs found no differences in cholesterol reduction
after the exercise intervention.
Rationale
Health outcomes targeted in these studies included triglycerides and
total cholesterol. Among persons with physical disabilities, 3 (75%) of 4
studies showed reduction in cholesterol (spinal cord injury) and triglycerides
(multiple sclerosis) (Table G11.4). Among persons
with cognitive disability, 1 (50%) of 2 studies reported reduction in
triglycerides (mental illness). In 3 of the 4 studies, subjects had high
cholesterol and triglycerides at baseline.
Table G11.4. Physical Activity and
Lipid Profiles in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Multiple
Sclerosisc |
1(17) |
– |
1(58) |
– |
– |
● |
– |
– |
| Physical: Muscular Dystrophy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Parkinson's Disease |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Spinal Cord
Injuryd |
– |
– |
1(33) |
1(30) |
– |
– |
● |
– |
| Physical: Stroke |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Traumatic Brain
Injury |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Alzheimer's Disease |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Intellectual
Disabilityd |
– |
– |
– |
1(59) |
– |
– |
– |
● |
| Cognitive: Mental
Illnessc |
1(60) |
– |
– |
– |
– |
● |
– |
– |
| Combined |
– |
– |
– |
– |
– |
– |
– |
● |
a S, Significant findings; b NS,
Non-significant findings; c Triglycerides; d Total cholesterol
Question 3. What Is the Evidence That
Physical Activity Improves Musculoskeletal Health in People With
Disabilities?
Conclusions
Type 1 evidence indicates that resistance exercise, aerobic exercise,
or a combination of resistance and aerobic exercise all increase muscle
strength in various subgroups with physical and cognitive disabilities.
Although less evidence exists on flexibility interventions for the 11
population subgroups, in the 4 RCTs conducted on individuals with Parkinson's
disease (n=1), Stroke (n=2) and Traumatic Brain Injury (n=1), findings were
significant for each disability group. Of the 4 non-RCTs on flexibility
training, 2 studies, which involved subjects with Spinal Cord Injury and
Combined Disabilities (i.e., physical and intellectual disabilities), were
found to be significant. The other two non-RCTs were not significant in persons
with Multiple Sclerosis and Intellectual Disability. Type 1 evidence finds that
flexibility can be improved in persons with Stroke, and type 2a evidence finds
that it can be improved in persons with Parkinson's disease and Traumatic Brain
Injury.
Type 2a evidence exists on the use of exercise in improving bone
mineral density (BMD) in people with physical and cognitive disabilities. Only
2 studies were identified that used an exercise exposure to improve BMD, one in
youth with Cerebral Palsy and the other study on adults with unilateral Stroke.
Both studies supported the use of exercise in improving BMD in these
populations, but more evidence is needed to determine whether these findings
will be supported by further studies.
Rationale
Muscle Strength
Table G11.5 summarizes the 37 exercise
interventions addressing improvements in muscle strength. Of the 17 RCTs, 14
(82%) studies reported significant positive effects. Of the 20 non-RCTs, 19
(95%) trials reported significant improvements in muscle strength.
Flexibility
Table G11.6 summarizes the intervention
research on flexibility. Four RCTs targeted improvements in flexibility in
persons with physical disabilities. All 4 (100%) studies reported significant
positive findings. Of the 4 non-RCTs, 2 (50%) reported significant improvements
in flexibility.
Bone Mineral Density
Two studies found in the literature used exercise to improve BMD in
people with disabilities. In the first study (RCT), children with cerebral
palsy were exposed to a program of various types of upper and lower extremity
exercises. The program consisted of 1 hour-long session per week for 8 weeks,
which was increased to 3 sessions per week for the next 24 weeks. The program
showed significant improvement in BMD compared to controls (61). In the second RCT, researchers concluded that exercise
can slow the decline in bone loss in the affected femoral neck of people with
unilateral Stroke (41).
Table G11.5. Physical Activity and
Muscle Strength in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
1(62) |
1(63) |
5(64-68) |
– |
– |
● |
– |
– |
| Physical: Multiple Sclerosis |
2(17;69) |
– |
1(70) |
– |
● |
– |
– |
– |
| Physical: Muscular
Dystrophyc |
1(71) |
1(72) |
1(73) |
– |
– |
● |
– |
– |
| Physical: Parkinson's Disease |
1(74) |
– |
1(75) |
– |
– |
● |
– |
– |
| Physical: Spinal Cord Injury |
1(76) |
– |
5
(20;34;
36;40;77) |
– |
– |
● |
– |
– |
| Physical: Stroke |
5
(38;41;
43;78;79) |
– |
3(80-82) |
– |
● |
– |
– |
– |
| Physical: Traumatic Brain
Injury |
– |
1(83) |
– |
– |
– |
– |
– |
● |
| Cognitive: Alzheimer's Disease |
– |
– |
1(47) |
– |
– |
– |
● |
– |
| Cognitive: Intellectual
Disability |
3(49;84;85) |
– |
– |
1(86) |
● |
– |
– |
– |
| Cognitive: Mental Illness |
– |
– |
– |
– |
– |
– |
– |
● |
| Combined |
– |
– |
2(57;87) |
– |
– |
– |
● |
– |
aS, Significant findings; bNS,
Non-significant findings; cNS in Myotonic Dystrophy group, S in
Charcot-Marie-Tooth group; reference was counted only one time.
Table G11.6. Physical Activity and
Flexibility in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Multiple Sclerosis |
– |
– |
– |
1(88) |
– |
– |
– |
● |
| Physical: Muscular Dystrophy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Parkinson's Disease |
1(89) |
– |
– |
– |
– |
● |
– |
– |
| Physical: Spinal Cord Injury |
– |
– |
1(37) |
– |
– |
– |
● |
– |
| Physical: Stroke |
2(43;90) |
– |
– |
– |
● |
– |
– |
– |
| Physical: Traumatic Brain
Injury |
1(45) |
– |
– |
– |
– |
● |
|
|
| Cognitive: Alzheimer's Disease |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Intellectual
Disability |
– |
– |
– |
1(86) |
– |
– |
– |
● |
| Cognitive: Mental Illness |
– |
– |
– |
– |
– |
– |
– |
● |
| Combined |
– |
– |
1(57) |
– |
– |
– |
● |
– |
a S, Significant findings; b NS,
Non-significant findings
Question 4. What Is the Evidence That
Physical Activity Improves Functional Health in People With Disabilities?
Conclusions
Functional health has a broad association with several performance
measures associated with basic and instrumental activities of daily living (ADL
and IADL). This includes walking speed, walking distance, quality of life,
functional independence, and balance. Evidence from a variety of studies
supports the use of exercise to improve walking speed and distance and other
measures of functional health across a range of disabilities.
A total of 74 interventions targeted one or more measures of
functional health under the categories of walking speed, walking distance,
quality of life/well-being, functional independence, and balance. These studies
provided type 1 evidence (Table G11.7) for the use
of exercise in improving walking speed in persons with Multiple Sclerosis,
Stroke, and Intellectual Disability, type 2a evidence for the use of exercise
in persons with Parkinson's disease and Alzheimer's disease, and type 2b
evidence for the use of exercise in persons with Cerebral Palsy and Spinal Cord
Injury (where the propulsion speed of pushing a wheelchair is used as an
equivalent to walking speed). The studies provided type 1 evidence that walking
distance can be improved in persons with Multiple Sclerosis, Stroke, and
Intellectual Disability (Table G11.8) and type 2a
evidence that walking speed can be improved in people with Parkinson's disease.
On Quality of Life (Table G11.9), the studies
provided type 1 evidence to support exercise for people with Multiple
Sclerosis, Spinal Cord Injury, and Stroke and type 2a evidence to support
exercise in people with Muscular Dystrophy, Alzheimer's disease, Intellectual
Disability, and Mental Illness. For Functional Independence (Table G11.10), the studies provided type 1 evidence
supporting the use of exercise in people with Stroke and type 2a evidence
supporting exercise in people with Multiple Sclerosis, Parkinson's disease,
Traumatic Brain Injury, and Alzheimer's disease. For Balance (Table G11.11), the studies provided type 1 evidence
supporting the use of exercise in improving balance only in people with
Parkinson's disease and Stroke. The studies had type 2b or 4 evidence for the
other disability subgroups.
Rationale
Walking Speed
Table G11.7 summarizes the 35
intervention studies that used walking speed as a health outcome. Of the 19
RCTs, 13 (68%) reported significant increases in walking speed. Of the 16
Non-RCTs, 10 (63%) reported significant increases in walking speed.
Table G11.7. Physical Activity and
Walking Speed in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
– |
1(91) |
2(64;66) |
2(65;67) |
– |
– |
● |
– |
| Physical: Multiple Sclerosis |
3
(18;92;93) |
1(69) |
1(94) |
3
(70;88;95) |
● |
– |
– |
– |
| Physical: Muscular Dystrophy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Parkinson's Disease |
1(96) |
– |
2(97;98) |
– |
– |
● |
– |
– |
| Physical: Spinal Cord
Injuryc |
– |
– |
1(77) |
– |
– |
– |
● |
– |
| Physical: Stroke |
6
(38;39;
79;99-101) |
3
(78;102;103) |
3
(80;104;105) |
1(82) |
● |
– |
– |
– |
| Physical: Traumatic Brain
Injury |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Alzheimer's Disease |
1(106) |
– |
– |
– |
– |
● |
– |
– |
| Cognitive: Intellectual
Disability |
2(107;108) |
– |
1(109) |
– |
● |
– |
– |
– |
| Cognitive: Mental Illness |
– |
– |
– |
– |
– |
– |
– |
● |
| Combined |
– |
1(110) |
– |
– |
– |
– |
– |
● |
a S, Significant findings; b NS,
Non-significant findings; c Specific to propulsion speed pushing a
wheelchair
Walking Distance
Table G11.8 summarizes the 18
interventions that used walking distance as an outcome. Of the 13 RCTs, 10
(77%) reported significant increases in walking distance. Of the five Non-RCTs,
four (80%) reported significant increases in walking distance.
Table
G11.8. Physical Activity and Walking Distance in People With
Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Multiple Sclerosis |
2(18;111) |
– |
1(94) |
– |
● |
– |
– |
– |
| Physical: Muscular Dystrophy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Parkinson's Disease |
1(96) |
– |
1(112) |
– |
– |
● |
– |
– |
| Physical: Spinal Cord Injury |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Stroke |
4
(39;41;
99;100) |
1(101) |
1(104) |
1(105) |
● |
– |
– |
– |
| Physical: Traumatic Brain
Injury |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Alzheimer's Disease |
– |
1(113) |
1(47) |
– |
– |
– |
● |
– |
| Cognitive: Intellectual
Disabilityc |
3
(50;107;108) |
– |
– |
– |
● |
– |
– |
– |
| Cognitive: Mental
Illnessd |
– |
1(114) |
– |
– |
– |
– |
– |
● |
| Combined |
– |
– |
– |
– |
– |
– |
– |
● |
a S, Significant findings; b NS,
Non-significant findings; c Down syndrome; d
Schizophrenia
Quality of Life and Well-Being
Table G11.9 summarizes the 27
interventions on quality of life/well-being. Of the 19 RCTs, 13 studies (68%)
reported significant positive findings. Seven (88%) of the eight non-RCTs (n=8)
demonstrated significant improvements in quality of life or well-being.
Table G11.9. Physical
Activity and Quality of Life in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Multiple
Sclerosisc |
3
(18;19;115) |
3
(15;18;84) |
1(21) |
1(88) |
● |
– |
– |
– |
| Physical: Muscular Dystrophy |
1(116) |
1(117) |
1(25) |
– |
– |
● |
– |
– |
| Physical: Parkinson's Disease |
– |
1(118) |
3
(98;119;120) |
– |
– |
– |
● |
– |
| Physical: Spinal Cord Injury |
2(76;121) |
– |
– |
– |
● |
– |
– |
– |
| Physical: Stroked |
4
(79;90;
103;122) |
1(90) |
– |
– |
● |
– |
– |
– |
| Physical: Traumatic Brain
Injury |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Alzheimer's Disease |
1(123) |
– |
– |
– |
– |
● |
– |
– |
| Cognitive: Intellectual
Disability |
1(124) |
– |
1(109) |
– |
– |
● |
– |
– |
| Cognitive: Mental Illness |
1(125) |
– |
1(126) |
– |
– |
● |
– |
– |
| Combined |
– |
– |
– |
– |
– |
– |
– |
● |
a S, Significant findings; b NS,
Non-significant findings; cOne RCT(18) showed a
significant finding in well-being (measured by the emotional well-being
subscore in the Multiple Sclerosis Quality of Life-54 scale) but a
non-significant finding in quality of life (measured by the overall score in
the Multiple Sclerosis Quality of Life-54); dOne RCT(89) reported a significant finding in well-being measured by
the Profile of Mood States instrument) but a non-significant finding in quality
of life (measured by the Stroke Specific Quality of Life Scale).
Functional
Independence
Table G11.10 summarizes the 35
interventions on functional independence, which was primarily measured by an
assessment of ADL, and IADL or motor function (i.e., motor control, function of
upper/lower extremity, motor skills). A total of 17 RCTs targeted improvements
in functional independence primarily in people with physical disabilities
(14 of the 17 RCTs). Out of these 17 RCTs, 9 (53%) reported significant
outcomes. In addition, 18 non-RCTs targeted people with physical disabilities,
and 14 (82%) of these studies reported significant findings on functional
independence.
Table G11.10. Physical
Activity and Functional Independence in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
– |
1(62) |
5(14;64-
66;68) |
1(67) |
– |
– |
● |
– |
| Physical: Multiple Sclerosis |
1(17) |
– |
– |
– |
– |
● |
– |
– |
| Physical: Muscular Dystrophy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Parkinson's
Diseasec |
1(127) |
1(89) |
5
(98;120;
128-130) |
1(129) |
– |
● |
– |
– |
| Physical: Spinal Cord Injury |
– |
– |
2(36;77) |
– |
– |
– |
● |
– |
| Physical: Stroked |
5
(78;100;
101;103;131) |
4
(78;99;
101;102) |
2(104;105) |
2(80;82) |
● |
– |
– |
– |
| Physical: Traumatic Brain
Injury |
1(83) |
– |
– |
– |
– |
● |
– |
– |
| Cognitive: Intellectual
Disability |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Mental Illness |
– |
– |
– |
– |
– |
– |
– |
● |
| Combined |
– |
1(110) |
– |
– |
– |
– |
– |
● |
a S, Significant findings, b NS
, Non-significant findings, c one Non-RCT (129) showed a significant finding in motor function but a
non-significant finding in functional independence; d two RCTs (77;101) reported a significant finding
in motor function in the lower extremity but a non-significant finding on
functional independence.
Balance
Table G11.11 summarizes the 21exercise
interventions on balance. Of the 13 RCTs, 6 (46%) reported significant
findings. Of the 8 non-RCTs, 6 (75%) reported significant positive findings.
The majority of studies were conducted on Parkinson's disease and Stroke.
Table G11.11. Physical Activity and
Balance in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
– |
– |
1(64) |
– |
– |
– |
● |
– |
| Physical: Multiple Sclerosis |
– |
1(69) |
– |
– |
– |
– |
– |
● |
| Physical: Muscular Dystrophy |
– |
1(116) |
– |
– |
– |
– |
– |
● |
| Physical: Parkinson's
Diseasec |
4
(74;89;
96;118) |
1(118) |
1(98) |
1(129) |
● |
– |
– |
– |
| Physical: Spinal Cord Injury |
– |
– |
– |
1(132) |
– |
– |
– |
● |
| Physical: Stroke |
2
(39;133) |
3
(38;41;101) |
3
(82;104;105) |
– |
● |
– |
– |
– |
| Physical: Traumatic Brain
Injury |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Alzheimer's Disease |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Intellectual
Disability |
– |
– |
1(109) |
– |
– |
– |
● |
– |
| Cognitive: Mental Illness |
– |
– |
– |
– |
– |
– |
– |
● |
| Combined |
– |
1(110) |
– |
– |
– |
– |
– |
● |
a S, Significant findings; b NS,
Non-significant findings; c One RCT (118)
under Parkinson's disease indicated a lower prevalence of falls among the
exercise group compared to the control group but also reported a
non-significant finding on the Berg Balance Score.
Question 5. What Is the Evidence that
Physical Activity Reduces Secondary Conditions in People With
Disabilities?
Introduction
Individuals with disabilities are likely to be at increased risk for a
number of preventable health problems referred to as secondary
conditions. According to Chapter 6 of the Healthy People 2010
report (1), secondary conditions are defined as
"...physical, medical, cognitive, emotional, or psychosocial consequences to
which persons with disabilities are more susceptible by virtue of an underlying
impairment, including adverse outcomes in health, wellness, participation and
quality of life (p. 163)." Several secondary conditions are prominent among
people with disabilities, and pain and fatigue are reported to be two of the
most common secondary conditions observed in people with physical and cognitive
disabilities (9).
Conclusions
Type 1 evidence exists for the use of exercise in reducing fatigue in
people with Multiple Sclerosis, type 2a evidence supports exercise in persons
with Muscular Dystrophy, and type 4 evidence supports exercise in the remaining
subgroups. In addition, type 1 evidence indicates that pain can be reduced in
people with Spinal Cord Injury, type 2a evidence based on one study has similar
findings for people with Down syndrome, and type 4 evidence exists that
exercise can reduce pain on the other subgroups.
Rationale
Fatigue
Table G11.12 summarizes the 10
interventions on fatigue. Of the 8 RCTs, 4 (50%) reported significant positive
health outcomes. Of the 2 non-RCTs, both (100%) showed significant positive
reductions in fatigue. The major target subgroup was persons with Multiple
Sclerosis.
Table
G11.12. Physical Activity and Fatigue Reduction in People With
Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Multiple Sclerosis |
3
(17;115;134) |
3
(18;19;135) |
2
(21;70) |
– |
● |
– |
– |
– |
| Physical: Muscular Dystrophy |
1(117) |
– |
– |
– |
– |
● |
– |
– |
| Physical: Parkinson's Disease |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Spinal Cord Injury |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Stroke |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Traumatic Brain
Injury |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Alzheimer's Disease |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Intellectual
Disability |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Mental Illness |
– |
– |
– |
– |
– |
– |
– |
● |
| Combined |
– |
– |
1(136) |
– |
– |
– |
– |
● |
a S, Significant findings; b NS,
Non-significant findings
Pain
Table G11.13 summarizes the evidence on 5
exercise interventions targeting musculoskeletal pain. Two RCTs and 2 non-RCTs
indicated significant reductions in pain in people with Spinal Cord Injury.
Three studies targeted reduction in shoulder pain in persons with Spinal Cord
Injury, and the other study evaluated general pain. Only one RCT involving
individuals with cognitive disabilities was identified, and this study reported
significant reductions in pain associated with intermittent claudication in
persons with Down syndrome.
Table G11.13. Physical Activity and
Pain Reduction in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
– |
| Physical: Cerebral Palsy |
– |
– |
– |
– |
– |
– |
– |
– |
| Physical: Multiple
Sclerosisc |
– |
– |
– |
– |
– |
– |
– |
– |
| Physical: Muscular Dystrophy |
– |
– |
– |
– |
– |
– |
– |
– |
| Physical: Parkinson's Disease |
– |
– |
– |
– |
– |
– |
– |
– |
| Physical: Spinal Cord Injury |
2
(76;121) |
– |
2
(34;137) |
– |
● |
– |
– |
– |
| Physical: Stroke |
– |
– |
– |
– |
– |
– |
– |
– |
| Physical: Traumatic Brain
Injury |
– |
– |
– |
– |
– |
– |
– |
– |
| Cognitive: Alzheimer's Disease |
– |
– |
– |
– |
– |
– |
– |
– |
| Cognitive: Intellectual
Disabilityc |
1(108) |
– |
– |
– |
– |
● |
– |
– |
| Cognitive: Mental Illness |
– |
– |
– |
– |
– |
– |
– |
– |
| Combined |
– |
– |
– |
– |
– |
– |
– |
– |
a S, Significant findings; b NS,
Non-significant findings; People with Down syndrome who suffered from
intermittent claudication
Question 6. What Is the Evidence That
Physical Activity Helps Maintain Healthy Weight and Improve Metabolic
Health?
Conclusions
Type 2a evidence indicates that exercise can improve body composition
in persons with Stroke, Intellectual Disability, Mental Illness, Traumatic
Brain Injury, and a combined group of individuals with different types of
physical disabilities. Type 4 evidence suggests the same finding for the
remaining disability subgroups. On metabolic factors, type 2a evidence exists
for improvements in fasting glucose and insulin sensitivity in two disability
subgroups (Stroke and Mental Illness) and type 4 evidence shows the same result
for the remaining subgroups.
Rationale
Body Composition
Table G11.14 summarizes the 19
interventions on body composition including those focused on body weight, body
fat, body mass index (BMI), and waist circumference. Of the 10 RCTs, 5
studies (50%) reported significant positive effects in decreasing body weight.
Of the 9 non-RCTs, 2 (22%) reported significant positive findings on body
composition.
Table G11.14. Physical Activity and
Body Composition in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Multiple
Sclerosisc |
– |
1(17) |
– |
1(58) |
– |
– |
– |
● |
| Physical: Muscular Dystrophy |
– |
– |
– |
1(138) |
– |
– |
– |
● |
| Physical: Parkinson's Disease |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Spinal Cord Injury |
– |
– |
– |
3
(33;77;139) |
– |
– |
– |
● |
| Physical: Stroke |
1(43) |
1(40) |
– |
– |
– |
● |
– |
– |
| Physical: Traumatic Brain
Injury |
1(45) |
– |
– |
1(46) |
– |
● |
– |
– |
| Cognitive: Alzheimer's Disease |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Intellectual
Disabilityc |
1(49) |
1(50) |
– |
– |
– |
● |
– |
– |
| Cognitive: Mental
Illnessd |
1(60) |
2(114) |
2(140;141) |
1(136) |
– |
● |
– |
– |
| Combined |
1(110) |
– |
– |
– |
– |
● |
– |
– |
a S, Significant findings; b NS,
Non-significant findings; Down syndrome; Schizophrenia
Metabolic Health
Three RCTs also targeted improvements in metabolic factors (fasting
glucose, insulin sensitivity, fasting insulin, and insulin-like growth
factor-binding protein-3). Two (67%) of these 3 studies reported significant
positive findings in people with Stroke (40) and
Schizophrenia (60) while one study (33%) reported
non-significant findings in people with Spinal Cord Injury (27).
Question 7. What Is the Evidence That
Physical Activity Improves Mental Health in People With Disabilities?
Conclusions
Type 1 evidence indicates that exercise can reduce depression in
people with Alzheimer's disease and Mental Illness. Type 2a evidence shows the
same result in persons with Multiple Sclerosis, Spinal Cord Injury, Stroke, and
Intellectual Disability, as does type 4 evidence in the remaining subgroups.
The highest level of evidence was reported in people with Mental Illness (6
RCTs reporting significant outcomes). Physical activity also appears to have
beneficial effects on several other mental health outcomes including
self-esteem, quality of sleep, interpersonal relationships, disruptive
behavior, negative symptoms, and anxiety. No type 1 studies were identified for
any of these outcomes. However, type 2a evidence was reported for beneficial
effects of self-esteem (Muscular Dystrophy, Traumatic Brain Injury, and
Intellectual Disability), quality of sleep (Spinal Cord Injury and Alzheimer's
disease), interpersonal relationships (Stroke and Mental Illness), and negative
symptoms (Mental Illness).
Rationale
Depression
Table G11.15 summarizes the 20
interventions targeting reduction in depression. Out of the 17 RCTs, 12 studies
(71%) reported significant reductions in depression. Three non-RCTs (100%) also
reported significant reductions in depression.
Table G11.15. Physical Activity and
Depression in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Cerebral Palsy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Multiple Sclerosis |
1(17) |
– |
1(21) |
– |
– |
● |
– |
|
| Physical: Muscular Dystrophy |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Parkinson's Disease |
– |
– |
– |
– |
– |
– |
– |
● |
| Physical: Spinal Cord Injury |
1(121) |
1(76) |
– |
– |
– |
● |
– |
– |
| Physical: Stroke |
1(122) |
– |
– |
– |
– |
● |
– |
– |
| Physical: Traumatic Brain
Injury |
– |
– |
– |
– |
– |
– |
– |
● |
| Cognitive: Alzheimer's Disease |
2
(123;142) |
1(106) |
– |
– |
● |
– |
– |
– |
| Cognitive: Intellectual
Disabilityc |
1(124) |
– |
– |
– |
– |
● |
– |
– |
| Cognitive: Mental Illness |
6
(54;55;
143-146) |
2
(53;125) |
1(126) |
– |
● |
– |
– |
– |
| Combined |
– |
1(110) |
1(56) |
– |
– |
– |
● |
|
a S, Significant findings; b NS,
Non-significant findings
Other Major Mental Health Outcomes
Table G11.16 summarizes the evidence on
12 exercise interventions targeting other mental health outcomes in persons
with disabilities, including self-esteem, quality of sleep, interpersonal
relationships, negative psychiatric symptoms, anxiety, and disruptive behavior.
In people with Muscular Dystrophy, Traumatic Brain Injury, and Intellectual
Disability, the improved health outcome was self-esteem. In people with Spinal
Cord Injury and Alzheimer's disease, quality of sleep improved; people with
Mental Illness had reduced negative psychiatric symptoms and increased
interpersonal relationships; and people with Stroke reported improvements in
interpersonal relationships.
Table G11.16. Physical Activity and
Other Major Mental Health Outcomes in People With Disabilities
| Disabilities |
Number of Studies
[reference]
RCT
Sa |
Number of Studies
[reference]
RCT
NSb |
Number of Studies
[reference]
Non-RCT
S |
Number of Studies
[reference]
Non-RCT
NS |
Type of
Evidence
1 |
Type of
Evidence
2a |
Type of
Evidence
2b |
Type of
Evidence
4 |
| Physical: Lower Limb Loss |
– |
– |
– |
– |
– |
– |
– |
– |
| Physical: Cerebral Palsy |
– |
– |
– |
– |
– |
– |
– |
– |
| Physical: Multiple Sclerosis |
– |
– |
– |
– |
– |
– |
– |
– |
| Physical: Muscular
Dystrophyc |
1(116) |
– |
1(24) |
– |
– |
● |
– |
– |
| Physical: Parkinson's Disease |
|
|
|
– |
– |
|
– |
– |
| Physical: Spinal Cord
Injuryd |
1(147) |
– |
– |
– |
– |
● |
– |
– |
| Physical: Strokee |
1(90) |
– |
– |
– |
– |
● |
– |
– |
| Physical: Traumatic Brain
Injuryc |
1(83) |
– |
– |
– |
– |
● |
– |
– |
| Cognitive: Alzheimer's
Diseased |
1(142) |
– |
– |
– |
– |
● |
– |
– |
| Cognitive: Alzheimer's
Diseasef |
– |
1(106) |
– |
– |
– |
– |
|
● |
| Cognitive: Intellectual
Disabilityc |
1(124) |
– |
– |
– |
– |
● |
– |
– |
| Cognitive: Mental
Illnessg |
1(145) |
– |
– |
– |
– |
● |
– |
– |
| Cognitive: Mental
Illnesse |
1(145) |
– |
1(148) |
– |
– |
● |
– |
– |
| Combined |
– |
1(110) |
– |
– |
– |
– |
– |
● |
a S, Significant findings; b NS,
Non-significant findings; c self-esteem; d quality of
sleep; e interpersonal relationships; f disruptive
behavior; g negative symptoms; h anxiety
Exercise Doses in the Studies
The majority of studies reviewed in this report included doses of
exercise that are typically used in studies targeting the general population.
Intensity of cardiorespiratory exercise was set at 50% or higher of target
heart rate reserve or VO2peak. Frequency of exercise ranged from 3
to 5 days a week and duration lasted from 30 to 60 minutes per session. The
precise quantitative characteristics of the dose-response relationship between
improvements in various health outcomes, however, still requires additional
research before certain conclusions can be made regarding what doses effect
what outcomes in targeted disability groups.
Question 8. What Do We Know About the
Safety of Exercise in People With Disabilities?
Introduction
Among some health care professionals, an underlying perception exists
that exercise may present an increased risk of injury for certain
individuals with disabilities. This section provides an overview of the
available literature describing issues associated with safety of exercise in
people with physical and cognitive disabilities from the 139 articles that the
Understudied Populations subcommittee reviewed for this chapter. The 139
exercise trials included 2,961 subjects exposed to an exercise intervention and
1,832 control subjects. The duration of the trials ranged from 1 week to 52
weeks.
Two abstractors carefully reviewed the Methods, Results, and
Discussion sections of each article to identify reported side effects or
adverse events. In particular, the abstractors focused on the reasons, when
available, that the subject withdrew from the study, to determine whether it
was related to the exercise exposure. The data are reported in frequencies and
percentages and separated by exercise and control groups. The information
contained in this section includes the most commonly reported complications or
adverse events reported for each disability subgroup.
To determine whether a reported event was considered a complication
(not serious) or adverse event (serious), we considered the following criteria
from the Office for Human Research Protections (OHRP, 2007) (149): event was (1) undesirable in nature; (2) related or
possibly related to the intervention; and (3) harmful to the participant either
physically or psychologically. For the purpose of this review, the subcommittee
modified these criteria to classify health complications associated with the
intervention as not serious adverse events and serious adverse
events. Serious adverse events frequently caused participants to drop out
of the study.
What Is the Frequency of Reported Adverse
Events Among People With Disabilities in the Exercise and Control Groups?
Adverse events were reported for 53 exercise subjects and 11 control
subjects (Table G11.17). The percentage of
exercise subjects (1.8%) and control subjects (0.6%) with any reported adverse
event was not substantially different. Similarly, the percentage of exercise
subjects (1.1%) and control subjects (0.6%) reported to have an adverse event
serious enough to cause them to drop out of the study also were not
substantially different.
Table G11.17. Number and Percentage
of Subjects With Adverse Events by Seriousness of Event and Exposure Group
| Exposure Group |
Seriousa |
Non-serious |
Total |
| Exercise Groups (n=2961) |
34 (1.1%) |
19 (0.6%) |
53 (1.8%) |
| Control Groups (n=1832) |
11 (0.6%) |
0 (0.0%) |
11 (0.6%) |
a Serious adverse events involved those in
which the subject dropped out of the study.
What Were the Commonly Reported Adverse
Events in Exercise Trials Among People With Disabilities?
This review of evidence identified very few reported adverse events
associated with exercise in people with physical and cognitive disabilities.
Disability-related risks and activity-related risks are two common issues
related to exercise training interventions in people with disabilities (150).
We reviewed all the reported serious and non-serious adverse events and
arranged them into 4 categories: (a) progression or recurrence of disease
(i.e., disability-dependent risks) including recurrent Stroke or Multiple
Sclerosis exacerbation, and/or worsening of conditions associated with the
disability such as elevated spasticity, bladder spasms, mild seizure,
recurrence of inguinal hernia, and increased depression; (b) cardiovascular
problems including angina symptoms, dizziness, drop in blood pressure, acute
myocardial infarction, and abnormal electrocardiogram; (c) falls; and (d)
exercise-related musculoskeletal problems, including muscle soreness, pain, and
increased fatigue.
Among the total number of adverse events [serious + non-serious]
reported in the exercise group (n=53) (Table
G11.18), musculoskeletal problems were the most commonly reported adverse
event (n=24, 45%). Falls, cardiovascular problems, and increased fatigue were
the other adverse events reported but occurred at a much lower rate.
Table G11.18 also illustrates that recurrent
Stroke, exacerbation in persons with Multiple Sclerosis, and cardiovascular
problems were the major reported adverse events in the control group. A
detailed overview of complications for each specific disability group can be
found in Table
G11.A1 [PDF - 114 KB].
Table G11.18. Classification,
Number, and Percentage of Serious/Non-Serious Adverse Events in Exercise and
Control Groups
| Classification of Adverse Events |
Exercise Group Percent (n/N) |
Control Group Percent (n/N) |
Progression or Recurrence of Disease:
Recurrent
strokea |
1.1% (6/538) |
0.6% (2/335) |
Progression or Recurrence of Disease:
Mild
seizurea |
0.2 % (1/538) |
0.0% (0/335) |
Progression or Recurrence of Disease:
Recurrence of inguinal herniaa |
0.2 % (1/538) |
0.0% (0/335) |
Progression or Recurrence of Disease:
Exacerbations of multiple sclerosisb |
1.1% (4/363) |
1.9% (5/266) |
Progression or Recurrence of Disease:
Increased
spasticityb |
0.6% (2/363) |
0.0% (0/266) |
Progression or Recurrence of Disease:
Increased
depressionc |
0.2% (1/522) |
0.0% (0/210) |
Progression or Recurrence of Disease:
Bladder
spasmsd |
0.5 (1/208) |
0.0% (0/75) |
| Falls |
0.2% (5/2961) |
0.0% (0/1832) |
| Cardiovascular Problems |
0.1% (4/2961) |
0.1% (2/1832) |
| Musculoskeletal Problem: Soreness or pain |
0.8% (24/2961) |
0.05% (1/1832) |
| Musculoskeletal Problem: Fatigue |
0.1% (4/2961) |
0.05% (1/1832) |
aIncludes only subjects in studies of
persons with a history of stroke; bIncludes only subjects in studies
of persons with multiple sclerosis; cIncludes only subjects in
studies of persons with mental illness; dIncludes only subjects in
studies of persons with spinal cord injury.
What Adverse Events or Complications Are
Concerns for Individuals With Stroke Who Want To Participate in a Physical
Activity Program?
People with Stroke can exercise safely without serious adverse events
by performing a careful prescreening exam and being supervised during exercise.
No data indicate that exercise will increase the rate of recurrent Stroke if
the appropriate monitoring and precautions are taken.
Among the 23 reviewed trials in which 538 Stroke survivors
participated in some type of exercise intervention, 6 participants (1.1%)
experienced a recurrent Stroke (39;103). In controls (n=335), recurrent Stroke occurred in 2
participants (0.6%) (102). The incidence of recurrent
Stroke in the exercise group was lower than the incidence rate (2.9% to 6.0%)
reported among individuals 3 to 6 months after their Stroke who are not
involved in an exercise intervention (101).
Angina symptoms, dizziness, mild seizure, and drop in blood pressure
during exercise or VO2peak testing were reported in 2 studies (43;78). All reported side effects
improved and all participants, with the exception of one individual who had a
drop in post-exercise blood pressure and was removed from the study, received
medical clearance to complete the exercise trial. Complications occurred in 2
Stroke participants who reported excess fatigue and dropped out of the study
(41;131). Three other participants
experienced back or knee pain but were able to complete the intervention (82).
Does Exercise Increase the Incidence of
Exacerbation in Individuals With Multiple Sclerosis?
Although it is important to closely monitor any changes in disease
symptoms for people with Multiple Sclerosis during and after the exercise
training sessions, the concern of potential worsening symptoms related to the
exercise exposure does not appear to be justified based on this literature
review. This finding is in agreement with a recent report by Ginis and Hicks
(7), who were charged with the development of a physical
activity guide for Canadians with physical disabilities. In particular, there
is no scientific evidence to support the notion that individuals with certain
forms of Multiple Sclerosis may have worsening symptoms related to increased
core temperature during/after exercise (7).
A total of 16 exercise trials involving persons with Multiple
Sclerosis were reviewed. Among the participants in the exercise groups (n=363),
4 experienced musculoskeletal problems (1.1%), 2 reported elevated spasticity
(0.6%), and 4 had an exacerbation (1.1%). In terms of the total number of
subjects in the control groups (n=266), 1 subject experienced knee pain (0.4%)
and 5 subjects had an exacerbation (1.9%). More specifically, 3 RCTs indicated
no difference in relapse symptoms between the exercise and control groups (15;18;19). One
trial reported that 2 participants in the exercise group experienced
exacerbations while none did in the control group (115).
However, 2 other trials reported that only participants in the control group
(n=3) had an exacerbation of symptoms compared to no relapse in the exercise
groups (16;68). Two studies indicated
adverse events related to the exercise exposure. Two subjects in the
intervention group experienced elevated spasticity of the lower extremity after
completing the exercise test (16), and a few participants
reported temporary low back muscle soreness (n=1) and leg muscle soreness (n=3)
during the initial training period (69). Based on this
literature review, there is currently no evidence to support the notion that
exercise imposes a higher risk of exacerbation or harm in people with Multiple
Sclerosis. This finding is consistent with a recent report published in Canada
(7) that concluded that exercise has no effect on disease
progression and should be an important component of disease management.
Is It Safe for People With Muscular
Dystrophy to Exercise?
Back pain, muscle soreness, and feelings of fatigue were the most
commonly reported adverse events associated with exercise in subjects with
Muscular Dystrophy. Among 230 subjects in the exercise groups of 12 examined
studies, 7 participants reported musculoskeletal problems (3.0%), compared to
no reported adverse events in the control groups (n=155). Specifically, 2
subjects withdrew from the exercise intervention due to training-related back
pain (73;151). Some subjects
complained of transient muscle strength reduction (n=3) at the beginning of the
exercise program (25;71;151) or expressed worsening fatigue (n=2) (22;23), but all subjects were able to
complete the intervention.
What Types of Adverse Events Were
Associated With Exercise Interventions in People With Spinal Cord Injury?
Muscle pain was the most commonly reported adverse event in people
with Spinal Cord Injury who participated in an exercise intervention. Among 208
subjects, 4 (1.9%) experienced muscle pain during the aerobic training sessions
(77) or after isokinetic testing (31). None of these complications affected their ability to
complete the exercise program. One study (77) noted that
exercise did not worsen the skin health of people with Spinal Cord Injury, and
in 2 of 4 subjects who had pressure sores not associated with the exercise
intervention, they healed by the completion of the study. One RCT reported that
exercise using an arm ergometer in the supine position caused one participant
(0.5%) to have bladder spasms (28).
What Types of Complications Were
Associated With Exercise Interventions in People With Cerebral Palsy?
In the 11 reviewed studies involving 123 subjects in the exercise
group and 69 subjects in the control group, no studies reported any
complications in individuals with Cerebral Palsy, and only one study reported
that a 6-week strengthening exercise intervention had negatively affected
self-concept in children with Cerebral Palsy, but the reasons behind the
unexpected reduction were unclear (152).
Is It Safe for Older Adults With
Alzheimer's Disease To Exercise?
The major concern regarding exercise interventions for older persons
with Alzheimer's disease is risk of falls. Among 229 individuals with
Alzheimer's disease in 6 different exercise trials in which the primary
exercise mode was walking, one study reported that there was no difference in
the incidence of falls over a one year period between the exercise and control
group referred to as the routine medical care group (139
versus 136) (106).
Is It Safe for People With Parkinson's
Disease To Exercise?
In the 14 exercise interventions reviewed consisting of 287 subjects
in the exercise condition and 183 subjects in the control condition, no adverse
events related to the exercise exposure in people with Parkinson's disease
occurred. In one study that was conducted to determine whether high-force
eccentric resistance exercise caused subjects with Parkinson's disease muscle
damage to their lower extremity, the researchers noted that the exercise
exposure did not have a negative impact on muscle damage or function (75).
Is It Safe for People With Mental Illness
or Intellectual Disability/Down Syndrome To Exercise?
Mental Illness
In the 15 studies that addressed the effects of exercise in
participants with major depression disorder (n=335), only 2 RCTs reported
adverse events related to the exercise exposure. These included musculoskeletal
injuries (n=8, 2.4%), chest pain (n=1, 0.3%), and increased severity of
depressive symptoms (n=1, 0.3%) (54;144). One study concluded that compared to medication use,
subjects in a treadmill exercise program experienced a lower incidence of
diarrhea or loose stools (21% for those exercising at home and 10% in
supervised exercise group) compared to those in the antidepressant group (31%)
(53). Further, no adverse events related to exercise
training were reported in 135 participants who were diagnosed with
schizophrenia and bipolar disorder (n=11). Among all control group participants
(n=210), no reported adverse events occurred.
Intellectual Disability
In the 12 exercise trials involving persons with Intellectual
Disability including Down syndrome, none of the studies reported any physical
complications. Only one trial reported that swimming in an integrated
environment caused negative effects on perceived athletic competence for youth
with intellectual disability compared to a segregated swimming class, although
the swimming performance of subjects in the integrated setting increased (153).
Overall Summary and Conclusions
This report systematically evaluated published evidence regarding the
effects of physical activity on people with physical and cognitive
disabilities. Table G11.19 presents the findings
in aggregate form, collapsing all physical disabilities into one group and
cognitive disabilities into another group. Aggregating these data allows for a
summary of the changes associated with exercise by health outcome and
disability group (physical versus cognitive).
To determine the strength of evidence, each health outcome across the
6 categories evaluated in this report was identified and categorized by level
of evidence according to the following criteria: Strong: 75% or more of
reviewed trials had significant findings; Moderate: 50% to 74% of reviewed
trials had significant findings; Limited: less than 49% of reviewed trials had
significant findings. Two or more studies with significant findings on the
identified health outcome were required for classification into strong or
moderate level of evidence. Based on this classification scheme, for people
with physical disabilities there was strong evidence that exercise can increase
cardiorespiratory, musculoskeletal and mental health outcomes; moderate
evidence to improve a variety of functional health outcomes and reduce the
effects of certain types of secondary conditions (i.e., pain and fatigue
associated with the primary disability); and limited evidence in improving
healthy weight and metabolic health. For people with cognitive disabilities,
there was strong evidence that exercise can improve musculoskeletal health,
select functional health and mental health outcomes; moderate evidence for
improving cardiorespiratory, musculoskeletal, and healthy weight and metabolic
health; and limited evidence for reducing secondary conditions.
Table G11.19. Summary Table on Level
of Evidence by Health Outcome Aggregated by Physical and Cognitive
Disabilities
| Health Outcome: |
Significant Number of
Trials |
Significant
Percent |
Non-Significant Number
of Trials |
Non-Significant
Percent |
Level of Evidence
Strong |
Level of Evidence
Moderate |
Level of Evidence
Limited |
Level of Evidence No
Evidence |
|
Physical Disability:
Cardiorespiratory Health |
33 |
84.6% |
6 |
15.4% |
● |
– |
– |
– |
| Physical Disability:
Musculoskeletal Health |
33 |
89.2% |
4 |
10.8% |
● |
– |
– |
– |
| Physical Disability: Functional
Health |
50 |
63.3% |
29 |
36.7% |
– |
● |
– |
– |
| Physical Disability: Secondary
Conditions |
10 |
71.4% |
4 |
28.6% |
– |
● |
– |
– |
| Physical Disability: Healthy
Weight and Metabolic Health |
4 |
30.8% |
9 |
69.2% |
– |
– |
● |
– |
| Physical Disability: Mental
Health |
10 |
83.3% |
2 |
16.7% |
● |
– |
– |
– |
| Cognitive Disability:
Cardiorespiratory Health |
8 |
72.7% |
3 |
27.3% |
– |
● |
– |
– |
| Cognitive Disability:
Musculoskeletal Health |
4 |
80% |
1 |
20% |
● |
|
– |
– |
| Cognitive Disability: Functional
Health |
10 |
83.3% |
2 |
16.7% |
● |
– |
– |
– |
| Cognitive Disability: Secondary
Conditions |
1 |
100% |
0 |
0% |
– |
– |
● |
|
| Cognitive Disability: Healthy
Weight and Metabolic Health |
4 |
50% |
4 |
50% |
– |
● |
– |
– |
| Cognitive Disability: Mental
Health |
11 |
78.6% |
3 |
21.4% |
● |
– |
– |
– |
In summary, since the publication of the Surgeon General's Report
on Physical Activity and Healthin 1996 (154), a
growing volume of research, including a number of RCTs, supports the use of
physical activity to improve health and function among people with
disabilities. With appropriate screening procedures, physical activity is
considered to be a relatively safe, effective, and very important health
recommendation for people with physical and cognitive disabilities. Data on
select disability groups show improvements in various health outcomes including
cardiorespiratory, musculoskeletal , functional, metabolic, and mental health,
in addition to reducing certain secondary conditions associated with the
primary disability such as pain and fatigue. An important caveat in
interpreting these findings is that each study had its own prescreening
evaluation for entrance into the study, which may have limited the sample to a
select group of individuals within a certain range of health and function.
Within this limitation, however, the consistency of the findings suggest that
exercise training is an effective intervention for promoting health at a low
risk of complications/adverse events in individuals with physical and cognitive
disabilities.
This report also provides a framework for continuing to build an
evidence base that can identify specific doses of physical activity in relation
to key health outcomes in people with a variety of physical and cognitive
disabilities. New studies and other disability groups can be added to the
database as more research is published. In the future, in areas where data are
lacking, researchers will be able to review the evidence and develop
interventions that target key health outcomes in underserved groups of
individuals with disabilities.
The development of appropriate inclusion/exclusion criteria is an
important approach to ensuring that exercise is safe for a specific subgroup of
people with disabilities. In all of the studies reviewed, screening and
specific inclusion/exclusion criteria were important in terms of distinguishing
individuals who were or were not appropriate for the intervention, usually
based on level of current health or functional limitations. With younger, less
disabled groups, risks associated with exercise appear to be typical of the
general population. Given the high rate of physical inactivity reported among
people with disabilities, it is critical for policymakers to promote physical
activity guidelines among professional groups and associations that have
regular contact with people who have disabilities (e.g., rehabilitation
providers, fitness professionals, health care professionals, public health
programs, service providers), and to support efforts to increase access to
physical activity venues including indoor and outdoor sports, recreation and
fitness facilities.
Safety of Exercise
This review also provides strong evidences that the benefits of
physical activity for people with physical and cognitive disabilities far
outweigh the risks. Very few reported serious adverse events (n=34, 1.15%).
Although most of the studies were done in a controlled setting and may have
excluded severely disabled subjects, the existing evidence supports the use of
physical activity as a recommended health promoting activity among people with
disabilities, including those with progressive disorders (i.e., multiple
sclerosis) or more severe conditions (i.e., muscular dystrophy).
Limitations
This report does not account for differences in methodological
quality. In the future, it would be helpful to qualify the RCTs based on
selection criteria such as adequate sample size, equal groups (control and
experimental) at baseline, blinding of study staff (i.e., different assessors
for pre- and post-testing), recording of participant completion and dropout,
and intention to treat. Studies were evaluated by their level of significance
and not according to their effect sizes. We focused on 11 key disability groups
only and did not include other disabled populations, such as those with
rheumatoid arthritis, and populations in which disabilities occur at low
incidences, such as those with spina bifida and polio, where not enough studies
were available to include in this review.
All of the studies reviewed in this report had several outcomes (e.g.,
physical and emotional well being, reduced fatigue, increased fitness, etc.),
and used a variety of interventions and doses of exercise (length of training,
frequency, duration, intensity, modality). Several studies included individuals
with a wide range of function and age, which may have attenuated the potential
effects of the training regimen on certain subgroups within the larger sample
(e.g., younger versus older subjects). Although heterogeneous populations make
it easier to recruit subjects (e.g., using individuals with para- and
tetraplegia in the same study) and obtain higher levels of statistical power,
generalizability to the entire population (i.e., Spinal Cord Injury or
Multiple Sclerosis) may be limited because of variations in health and function
among the different subjects.
Another limitation was that the studies did not necessarily represent
individuals with severe forms of the disability (i.e., tetraplegia vs.
paraplegia, severe cerebral palsy versus mild cerebral palsy; advanced types of
multiple sclerosis). Therefore, it is not possible to generalize the findings
to various subgroups within each disability who may have had an advanced
condition. Data on certain subgroups (i.e., lower limb loss, cerebral palsy)
also were limited, which reduced their generalizability.
Although we identified all the complications/adverse events reported
in the 139 studies that were reviewed, it is possible that some of the studies
did not report certain complications or adverse events.
Research Needs
It is important to identify optimal doses of exercise based on
evidenced-based outcomes that delineate the safety of the activity and the
specific health outcomes achieved by various exercise regimens for various
disabled populations. The lack of data pertaining to the frequency, intensity,
duration, and modality components of an exercise prescription for persons with
disabilities has made it difficult to recommend specific training regimens to
improve certain health outcomes or reduce the severity of certain secondary
conditions associated with the disability (e.g., pain, fatigue).
The questions posed for this review suggest several lines of research
to understand the dose-response effects of exercise in the treatment and
management of targeted health outcomes. In order to establish a focused
research agenda, studies should have an acceptable level of homogeneity (i.e.,
age, health status, functional level), and a consistent methodology, training
dose and targeted outcome(s).
The very low exercise participation rate observed among people with
disabilities may be associated with the gap between an individual's needs,
interests and functional level, and the barriers that are often present in the
environment. Environmental factors also can have a significant role in a
person's ability to exercise, including access to exercise equipment or
programs/classes, available transportation to and from the facility, and cost
of the program. Collectively, these factors can make it extremely difficult for
someone with a disability to participate in regular exercise. Health
professionals must increase their awareness of the personal and environmental
barriers that can have a substantial negative effect on participation in people
with different types and severities of disabilities.
Specific Research Recommendations
- There are no prospective cohort studies on people with
disabilities. These studies should be conducted to determine the frequency,
intensity, or duration of physical activity associated with key health
outcomes, including reduction in certain secondary conditions associated with
the specific disability subgroup (e.g., pain in spinal cord injury, fatigue in
multiple sclerosis, deconditioning in intellectual disability). Studies should
be stratified by age, functional level, and severity of disability.
- The heterogeneity between and within disability groups and the low
incidence of many disabilities make it extremely difficult to obtain an
adequate sample size when recruiting from one setting. Multi-center clinical
exercise trials are recommended to achieve adequate statistical power and to be
able to generalize findings to certain subgroups within the targeted disability
(e.g., young adults with paraplegia). A high level of intervention fidelity
must be established that employs the same testing instruments, procedures and
training regimen.
- RCTs are needed to examine the effects of various types of
exercise in addition to the actual training volume (frequency, intensity,
duration). Group exercise such as tai chi or yoga may have the additional
social benefit, which may improve outcomes but may also confound the benefit of
the specific dose of exercise. Future studies should control for the social
aspect of exercise in order to obtain accurate data on the exercise regimen
itself versus the social benefits associated with exercising in a group.
- Numerous self-report assessment tools have been developed to
measure changes in health. It is difficult to make comparisons between studies
when instruments are not the same or not explained well enough to make critical
comparisons between them. Given the small sample of many disabled subgroups, it
would be helpful to have a recommended set of instruments for each targeted
outcome with good psychometric properties so that data from various studies can
be compared to each other.
- Innovative strategies for recruiting individuals who generally do
not volunteer for research studies must become a high priority. Because most
experimental research is conducted with volunteers, it is difficult to
generalize the study's findings to the entire subgroup. People who volunteer
for exercise-related research may generally be younger and/or have a higher
functional level. This is a common problem in experimental research but may be
an even greater issue among people with disabilities because sample selection
is limited to a small subset of the population and barriers such as
transportation limit opportunities for participation in clinical research.
- Several studies emphasized the unique aspects of improving social
integration and/or quality of life. These measures are often obtained from
self-report measures. It would be helpful to better understand how these
measures are associated with objective measures, such as quantifying an
increase in community participation (i.e., increased number of outdoor and/or
social activities, greater amount of time outside the home for social events,
increased employment). The fact that physical activity can improve mental
health and quality of life is an intriguing concept that should be examined in
future research with objective measurement of these outcomes.
- Given the difficulty in identifying and recruiting subjects from
certain populations with disabilities that have low incidence (e.g., spina
bifida, muscular dystrophy, cerebral palsy), categorizing subjects by function
rather than disability may be an alternative approach to increasing recruitment
size and identifying key health outcomes that generalize across disability
groups. Use of the International Classification of Functioning Disability and
Health (ICF) (155) model would allow researchers to
identify specific eligibility criteria by impairments (e.g., lower extremity
paralysis) and/or activity limitations (e.g., unable to walk) rather than by
disability.
Review of the Science: Physical Activity
During Pregnancy and the Postpartum Period
Introduction
Early studies on physical activity and pregnancy were concerned more
with harm to the mother and fetus than with potential benefits. Most studies
used animal models, though some human studies examined cardiorespiratory
responses and thermoregulation in the mother, fetal heart rate, and pregnancy
outcomes such as birth weight, gestational length, and adverse events.
The American College of Obstetricians and Gynecologists (ACOG)
developed the first exercise guidelines for pregnant women in 1985 (156). Those guidelines were based on limited data and were
conservative. They included upper limits of 140 beats per minute for maternal
heart rate and recommended that sessions of strenuous activity be limited to 15
minutes. The guidelines also noted the potential need to individualize physical
activity recommendations.
Between 1985 and 1994, nearly 600 relevant studies were published,
most of which focused on doing no harm. Many studies were laboratory
investigations with small sample sizes, and most involved acute maternal
responses to exercise. The data suggested no detrimental effects of the
targeted exercise to mother or fetus, possible reduced length of labor,
possible improvement in gestational diabetes, and relatively little loss of
fitness by chronic exercisers. The use of a target heart rate was found to be
quite problematic. ACOG updated its guidance for exercise during pregnancy in
1994 (157) and again 8 years later (158). Currently, ACOG recommends that pregnant women
participate in 30 minutes of moderate-intensity physical activity on most days
of the week in the absence of medical/obstetrical complications (158). Although this recommendation does not endorse
participation in vigorous activities for all (for which information is scarce),
it does not recommend against women being strenuously active during
pregnancy.
Overview of Questions Asked
This part of the Understudied Populations section
addresses 3 questions:
- What does recent research indicate about
the possible risks of moderate- or vigorous-intensity physical activity by
women who are pregnant?
- Does being physically active while
pregnant provide any health benefits?
- Does being physically active during the
postpartum period provide any health benefits?
Data Sources and Process Used To Answer
Questions
The evidence presented here was based on references included in the
review of the literature for the 2006 Institute of Medicine report on physical
activity and health (159) and an updated search of the
Cochrane Library and MEDLINE for published RCTs, meta-analyses, and review
articles. Search terms included exercise, physical activity, pregnancy,
postpartum, the names of experts in the field and/or a combination of these
terms. Search limits included human studies in women published in the English
language from 1996 onward. Relevant articles were reviewed and the
subcommittee's conclusions were summarized and presented here.
Question 1. What Does Recent Research
Indicate About the Possible Risks of Moderate- or Vigorous-Intensity Physical
Activity by Women Who Are Pregnant?
Moderate-intensity leisure-time physical activity is not associated
with an increased risk of low birth weight, preterm delivery, or early
pregnancy loss (160;161). A recent
review concluded that moderate-intensity leisure-time physical activity during
pregnancy normally does not affect birth weight. However, participation in
vigorous activities has been associated with small reductions (about 200 to 400
grams) in birth weight compared to birth weights of babies born to less active
women (160). Similar results were reported in a
meta-analysis published in 2003 (162).
Information on strenuous activity during pregnancy is very limited. A
prospective study in the United States found that participation in vigorous (6
or more METs) activities in the first and second trimesters was associated with
non-significant risk reductions for preterm delivery (163). Similarly, a prospective Australian study found no
significant effects of vigorous physical activity during pregnancy on
gestational age at birth or birth weight (164). Results
from these studies must be applied cautiously as only a select subset of
pre-trained women chose to continue vigorous activity during pregnancy.
Question 2. Does Being Physically Active
While Pregnant Provide Any Health Benefits?
In 2005, an expert panel was assembled to examine the impact of
physical activity during pregnancy and the postpartum period on maternal
chronic disease risk (165). The panel also addressed the
association of physical activity with the risk of preeclampsia and gestational
diabetes mellitus (GDM). Regular physical activity in early pregnancy has been
found to be associated with a reduced risk of preeclampsia in 2 case-control
studies (166;167) and one cohort
study (168). The evidence is not strong, but is
consistent. A more recent Cochrane Review of RCTs found a non-significant
reduction in risk of preeclampsia associated with moderate physical activity
during pregnancy; although only two trials with a combined sample size of 45
women met review criteria (169). A Cochrane Review for
GDM also showed no significant effect of physical activity (170). However, reviews of observational studies consistently
show a reduced risk of GDM associated with moderate physical activity
participation before and/or during early pregnancy (160;171). Although conclusions from
these reviews along with data from a large population-based prospective study
(172) confirm that leisure-time physical activity reduces
risk and helps to treat GDM, data are insufficient to develop specific optimal
physical activity guidelines for GDM prevention.
Investigators also have evaluated maternal physical activity in
relation to health-related fitness, psychological health, and the course of
labor and delivery. The evidence clearly supports that maternal physical
activity of any kind helps to maintain fitness levels, which normally decrease
during pregnancy (161;173). Fewer
studies have considered maternal mood during pregnancy, yet available evidence
suggests that maternal physical activity improves mood and is associated with
increased self-esteem (161;174).
Conflicting results exist relating maternal physical activity to the course of
labor and delivery. Some studies report easier and shorter deliveries, others
find no effect, and some show that induction of labor is used more often among
women who exercise (161). Variances in methodology and
activity definitions make these studies difficult to summarize and compare. A
recent study (175) showed that women who exercised during
pregnancy were less likely to have preterm delivery compared to their sedentary
counterparts. However, the authors were not able to clearly separate the role
of moderate versus vigorous activity on this effect.
Question 3. Does Being Physically Active
During the Postpartum Period Provide Any Health Benefits?
Available evidence has shown maternal physical activity during the
postpartum period is associated with enhanced mood (165;176;177),
increased cardiovascular fitness (177;178), and obesity prevention (179).
Larson-Meyer (177) reviewed approximately 60
cross-sectional studies and RCTs on postpartum weight reduction, specifically,
looking at postpartum exercise. When compared to no physical activity, moderate
physical activity did not appear to increase postpartum weight reduction unless
caloric restriction was included. Studies also have showed that moderate
intensity aerobic exercise did not adversely affect milk volume, composition,
or infant growth (165;177;180). Some longitudinal data on future disease risk come
from Rooney and colleagues (179) who examined nearly 800
women immediately postpartum and again 15 years later. Disease and risk factor
development (diabetes, heart disease, dyslipidemia, and hypertension) were
directly related to weight gain over 15 years. Women who continued to perform
aerobic exercise postpartum were less likely to become obese than those who did
not. In summary, in the absence of medical complications, physical activity
during the postpartum period is beneficial to the overall health of the mother
(both in the short- and long-term) while not adversely affecting her newborn's
development.
Overall Summary and Conclusion
Although the benefits of maternal physical activity have clearly been
demonstrated, prospective, randomized intervention studies in diverse
populations are greatly needed. Based on current evidence, unless there are
medical reasons to the contrary, a pregnant woman can begin or continue a
regular physical activity program throughout gestation, adjusting the
frequency, intensity, and time as her condition warrants. Very little evidence
exists for the dose of activity that confers the greatest health benefits to
women during pregnancy and the postpartum period. In the absence of data, it is
reasonable for women during pregnancy and the postpartum period to follow the
moderate-intensity physical activity recommendations set for adults unless
specific medical concerns warrant a reduction in activity. Habitual exercisers
with high fitness levels undergoing a healthy pregnancy need not drastically
reduce their activity levels, provided that they remain asymptomatic and
maintain open communication with their health care providers so that
adjustments can be made if necessary. This same communication should be
continued into the postpartum period, where the time needed before a woman
returns to performing regular physical activity should be governed by medical
safety concerns, rather than a set time period.
Review of the Scientific Evidence: Racial
and Ethnic Diversity
Introduction
The charge to the PAGAC by the Secretary of Health and Human Services
was to review the science pertaining to physical activity and public health,
including the literature that would help ensure that new federal physical
activity guidelines and policy statements would apply to all Americans and, as
best possible, also meet the needs of specific subgroups of the population.
Chronic disease risk and disease burden in the United States are
higher in racial/ethnic minority communities than in non-Hispanic whites. Thus,
special attention to the particular physical activity needs and requirements of
these groups is warranted. To summarize the science addressing racial/ethnic
specific health-related responses to various doses of physical activity, each
subcommittee identified and reported data for specific racial/ethnic groups.
The objective was to determine whether such responses significantly differed
from those observed for non-Hispanic white men and women.
Compared to the large number of studies published since 1995
investigating the role of physical activity in disease prevention and health
promotion, quite limited data exist on race-ethnic specific responses (181-185). Many studies have included only non-Hispanic white
participants, or have included small sub-samples of other racial and ethnic
groups, precluding meaningful sub-group analyses by race/ethnicity. Also
limiting a comprehensive review of this issue is the failure of some authors to
include (and editors to require) precise information on the racial/ethnic
characteristics of the study populations (186). A few,
mostly observational, studies have included data on several racial/ethnic
populations or on one population other than non-Hispanic whites. Most of the
latter have been studies conducted in countries other than the United States.
The contexts for the physical activity-disease association in other countries
may differ for similar populations living in the United States. However,
studies in other countries provide a broader and more diverse perspective than
may be obtained from US data alone.
Background
The public health burden imposed by physical inactivity may be
disproportionately high in ethnic minority and lower SES communities (187-192). African Americans, American Indians/Alaska
Natives, Asian Americans, Pacific Islanders, and Latinos have significantly
lower levels of regular physical activity, and significantly higher levels of
inactivity than do whites (6;193).
Though Asian Americans and Pacific Islanders have traditionally been merged
together in most data sets, disaggregation of these groups is critical because
they tend to be at the opposite ends of the spectrum of body weight, which
influences and is influenced by physical activity (Asian Americans have less,
and Pacific Islanders, more obesity, compared to other population groups).
Growing but smaller ethnic minority populations who are not always separately
identified (e.g., South Asian and Middle Eastern), also likely experience
challenges in achieving adequate physical activity participation (194). These differences are magnified by the recent data
documenting the extremely low levels of objectively measured
moderate-to-vigorous physical activity, and high levels of sedentariness,
across the entire United States population, but especially among ethnic
minorities (195;196).
Disparities exist in most physical activity-related chronic diseases
and conditions. For example, overweight and obesity rates vary substantively by
ethnicity, even taking into account SES (e.g., (197); (198), (199)). Despite the public
health consensus that physical inactivity is an important determinant in a host
of health disparities across population segments, racial/ethnic differences in
the contribution of physical activity to various health outcomes have rarely
been systematically investigated. Several reasons for possible differences have
been postulated. There may be modest differences in the energy cost of physical
activity, for example, as a result of racial anthropomorphic variations (see
Part G. Section 4: Energy Balance
for additional discussion). Alternatively, the dose response of
physical activity on health outcomes may be similar across racial/ethnic
populations, while cultural and contextual factors may lead to differences in
the achieved effective dose of a particular intervention (implementation) or in
the accuracy of a particular measure in capturing the dose delivered
(evaluation).
The marked skewing of racial-ethnic minority populations toward lower
SES compared with whites complicates interpretation of these observations of
racial/ethnic differences in public health surveillance (200). SES explains some, but usually not all, racial/ethnic
differences. In some studies, ethnicity was no longer significant when other
sociodemographic variables reflecting SES were included in multivariate
analyses of physical activity (185;201). In others, the magnitude of physical activity
variation by ethnicity was statistically significant but much less substantive
than variations related to other socio-demographic and health status
characteristics (193;202).
This skewing makes it difficult, if not impossible, to examine the
influence of SES independent of race/ethnicity on physical activity-related
outcomes. In fact, because the data are so scant, heterogeneity between and
within racial/ethnic groups generally limits extrapolation between studies.
Inter-ethnic, and even intra-ethnic comparisons are further complicated because
of the substantial confounding of race/ethnicity and SES. Lower SES
non-Hispanic whites comprise a relatively low proportion of the white
population overall, and are underrepresented in public health research. In
contrast, substantial numbers and in some cases a majority of African American,
Latino, Pacific Islander and American Indian study participants are of lower
SES. As a result, inadequate sub-samples of lower income non-Hispanic whites or
higher income ethnic minority participants hinder analytical disaggregation by
race/ethnicity and SES. Therefore, we will focus on racial/ethnic differences,
recognizing that race/ethnicity is, in part, a proxy measure for SES.
Overview of Questions Asked
This portion of the Understudied Populations
section addresses one major question:
- Is there evidence that the physical
activity dose for improving health should vary for people depending on race or
ethnicity?
Data Sources and Process Used To Answer
Questions
A search of the Physical Activity Guidelines for
Americans Scientific Database identified research articles on the
effect of physical activity on racially/ethnically diverse groups. These
articles were not readily identifiable within the database, as many articles
retrieved using racial- or ethnic-specific keywords had very small minority
samples and mention of racial/ethnic variations in outcomes were rare. Because
so few relevant studies were available in the Database, pertinent reviews
available through a MEDLINE search were considered, as were recently published
and "in press" journal articles identified through reference lists of articles
cited and through expert consultation.
Question 1. Is There Evidence That the
Physical Activity Dose for Improving Health Should Vary by Race or
Ethnicity?
Conclusions
Data addressing race- and ethnicity-specific responses to physical
activity are still extremely limited. Very few subgroup analyses were reported
that permitted direct comparisons between racial/ethnic groups. No clinically
significant differences were identified in the review of studies comparing
responses to physical activity between different racial or ethnic groups or in
analyses adjusting for race and ethnicity. Data on various health outcomes in
prospective observational studies involving populations other than non-Hispanic
white men and women do not suggest any race- or ethnicity-specific responses to
physical activity. However, too little evidence is available to draw firm
conclusions. While additional data are being generated, the available evidence
suggests that the major health benefits of physical activity are not race- or
ethnicity-specific.
Rationale
Provided below is a brief summary of published research addressing the
issue of race- and ethnicity-specific health-related responses to physical
activity. For additional information about the health outcomes described here
and for information about race/ethnicity data for other outcomes, the reader is
referred to the remaining chapters in Part G: The Science Base. In general
for these outcomes, data are insufficient to draw any conclusions regarding
race- or ethnicity-specific effects or dose response.
All-Cause Mortality
Three studies included nationally representative samples of
participants (203-205) and another comprised 48.3% blacks
(206). In addition, 2 studies specifically enrolled
Hispanics (207) and Japanese-American men (208). Five studies were conducted in Asia enrolling Chinese
and Japanese subjects (209-213). No inter-ethnic/racial
differences in the effect of physical activity on all-cause mortality were
apparent.
Cardiorespiratory Health
Few studies conducted in the US have had an adequate sample size and
clinical outcomes to evaluate the association between physical activity and
cardiovascular disease (CVD) clinical events in race-ethnic groups other than
non-Hispanic whites. An analysis of this issue in data from the Women's Health
Initiative Observational Study (214) included 61,574
white women and 5,661 black women with a mean follow-up of 3.2 years. The
relation between physical activity level (quintiles of MET-hours per week) and
CVD clinical events was significant for both groups of women with relative risk
(RR) for the highest versus lowest quintile of activity for white women being
0.56 (P for trend <0.001) and for black women 0.48 (P for
trend = 0.02). In contrast to these results, a report on the Atherosclerosis
Risk in Communities (ARIC) study population indicated that although there was a
significant inverse relation between activity level and CVD clinical events in
white men and women, no such relation was found for either black men or women
(215). The authors suggest that this lack of association
in blacks may be due to the limited number of blacks reporting vigorous
physical activity (5% in black men versus 15% in white men). The different
geographic locations of the black (primarily Mississippi) and white (Washington
State, Minnesota, and North Carolina but not Mississippi) cohorts in ARIC may
be relevant here. However, outside the United States where the relation between
physical activity level and CVD clinical events has been evaluated in
racial/ethnic populations other than whites, no indication exists that the
favorable association frequently reported for non-Hispanic white men and women
is absent. For example, physically active Japanese men and women living in
Japan (216) and older Japanese men living in Hawaii (208) had lower CVD mortality rates than their least active
counterparts. Similar results have been reported for Chinese women living in
Shanghai (212) and Chinese men and women living in Hong
Kong (210). In a case-control study that included men and
women, conducted in New Delhi and Bangalore India, the RR for myocardial
infarction of 145 or more MET-minutes per day of LTPA versus no activity was
0.44 (95% CI 0.27-0.41) and time spent in non-work sedentary activity also was
directly associated with risk of myocardial infarction (RR for at least 215
minutes per day versus less than 70 minutes per day = 1.58 [95% CI:
1.05-2.36]). In an aerobic exercise training study lasting 20 weeks that
included African-American and non-Hispanic white men and women, no
racial-ethnic differences were observed in the percent increase in
VO2max (217).
Cancer
Within the United States, associations between increased physical
activity and decreased breast cancer incidence have been observed in
multiethnic populations (218-220) as well as in
investigations in specific racial/ethnic minorities: black (219;221), Hispanic (220;222), and Asian American women (223). No differences in the magnitude or quality of this
association were apparent.
Energy Balance
Twenty-four articles that included data on various racial-ethnic
groups were identified during the systematic literature review. Half reported
on studies conducted outside of the United States, including 9 in Asia/Pacific
Islands, 2 in Africa, and 1 in Central America. Fourteen were cross-sectional
studies (185;202;224-235), 3 were longitudinal cohort studies (201;231;236),
and 7 were interventions (192;237-242). Only one of the intervention studies included a
direct comparison between two racial-ethnic groups, whites and blacks (239). The actual body weight lost during the 20 weeks of
exercise was the same for both groups – 0.2 kilogram – and
this loss was statistically significant in whites but not blacks, most likely
because of a lower statistical power for the blacks due to their much smaller
sample size. It should also be noted that this was designed as an exercise
training study and not a weight loss study. Also, adjustments for subtle
racial/ethnic anthropomorphic variations that might explain any racial/ethnic
differences (e.g., shorter trunk length in blacks), identified in experimental
exercise physiology studies (243) were not reported (239).
Metabolic Disorders
Preventing the Metabolic Syndrome
The majority of studies with large sample sizes was either conducted
in Europe or was composed of whites of American or European descent. Though
some of the better studies were conducted in populations composed of both
African Americans and non-Hispanic whites, no studies examined the physical
activity-metabolic syndrome association in an African-American or Hispanic
population only (244-246). Thus, limited data are
available on the relation between physical activity or fitness and preventing
metabolic syndrome in populations other than non-Hispanic whites. It should be
noted that studies that used populations composed of both whites and African
Americans, such as NHANES (cross‑sectional) and CARDIA (prospective),
showed a strong dose response between activity (or fitness) and prevention of
metabolic syndrome (245;246).
Preventing Type 2 Diabetes
In observational studies that included women only, 3 large US cohort
studies (247-250) all found that greater physical
activity was associated with a lower incidence of diabetes. However, in one
study, this relation was present only in white women and not in women of
African-American, Hispanic or Asian descent (250). These
findings await confirmation because the study may not have been powered to
detect differences across all racial/ethnic groups. Results were based on
self-report of diabetes diagnosis in the total population but were confirmed in
a subset using blood samples and physician reports. Data from RCTs as well as
observational studies suggest clearly that, overall, women and men benefit from
increased levels of physical activity in terms of preventing type 2 diabetes.
In the Diabetes Prevention Program (251), treatment
effects did not differ significantly according to either sex or racial/ethnic
group. Although participant numbers became too small for clear results when
grouped by ethnicity, it appears that risk reduction compared with placebo was
greater for the lifestyle group (both diet and physical activity were parts of
this intervention) than for the group taking the common diabetes drug,
Metformin in whites (50% versus 12%, respectively) and Hispanics (57% versus
2%, respectively) (252). In African Americans (42% versus
29%) and Native Americans (43% versus 42%), the lifestyle and Metformin groups
showed more similar efficacy. For Asian Americans, Metformin showed a
non-significantly greater reduction than intensive lifestyle intervention (62%
versus 30%).
Overall Summary and Conclusions
Given the paucity of outcome-specific studies providing useful
information about racial/ethnic minority populations, evidence of physical
activity influences across content areas was assessed
generally.
- Across studies, results indicate that physical activity is related
to a host of health outcomes in racial/ethnic minority populations. The
direction of the association is the same in all racial/ethnic groups for which
data were examined, with physical activity generally exerting a protective
effect.
- Across studies, findings suggest that no minimum threshold of
effect exists, especially for chronically inactive people (i.e., the majority
of American adults). The lack of minority racial/ethnic inclusiveness of the
physical activity promotion research literature may actually underestimate
effects of a given dose, as more advantaged participants may have less capacity
to benefit from preventive interventions (ceiling effects) (253). Recently reported data support that engaging in some
amount of physical activity is better than doing nothing, and higher amounts of
physical activity are associated with greater benefits and a broader spectrum
of benefits.
- Subgroup analyses permitting head-to-head inter-racial/-ethnic
comparisons of the influence of physical activity were rare. The very limited
data available provide no indication that dose response differs between
racial/ethnic groups.
Research Needs
- An increased number of federally-funded studies should be powered
to include sufficient representation of at least one racial/ethnic minority or
lower SES population, with sufficient sample size to permit subgroup analyses
by race/ethnicity or SES. Adequate sampling of at least one understudied group
should take precedence over achieving population representative samples, which
usually have inadequate sample sizes for inter-group comparisons. The latter
requirement has been enforced by review committees for more than a decade, with
little progress in identifying racial/ethnic variations in the spectrum or
level of benefit of a given dose of physical activity. Requests to be excused
from this requirement should have strong scientific justification. Strict
exemption criteria should be established in advance, and then rigorously
applied by scientific review committees as a part of their scrutiny of
racial/ethnic group inclusion overall.
- Cultural proficiency of recruitment and retention approaches and
adequacy of resources directed toward recruitment and retention should be
scrutinized by grant review committee members with special expertise in this
area, similar to the separate assessments of adequacy of study methods and
analytical approaches by review committee statisticians.
- Federal program officers should manage and balance their portfolios
to ensure that racial/ethnic differences in PA-related exposures and outcomes
are under active investigation, using RFAs and other mechanisms to direct
funding toward disparities examination and elimination.
- Journals should require reporting of race/ethnicity, sex and SES of
samples in the abstract as well as the body of the text.
- Subgroup analyses should be requested by journal editors and
reviewers when sample size is sufficient, and further data disaggregation
encouraged, to examine interactions between sociodemographic characteristics,
e.g., sex-ethnicity, SES‑ethnicity.
- Abstraction databases should include search criteria that permit
ascertainment of inclusiveness, i.e., subgroup analyses by race/ethnicity or
SES.
- Specific research questions deserve particular emphasis, such as
the precise role in weight maintenance of racial anthropomorphic variations in
resting or activity-related energy metabolism (as opposed to or in concert with
age or sex-related differences) or in body composition.
Reference List
- United States.Dept.of Health and Human Services.
Healthy people 2010 : understanding and improving health. Washington, DC: U.S.
Dept. of Health and Human Services : For sale by the U.S. G.P.O., Supt. of
Docs.; 2000.
- Field MJ, Jette AM, Institute of Medicine (. The
future of disability in America. Washington, DC: National Academies Press;
2007.
- Rimmer JH. Exercise and physical activity in
persons aging with a physical disability. Phys.Med.Rehabil.Clin.N.Am. 2005
Feb;16(1):41-56.
- Centers for Disease Control and Prevention. The
imperative of public health in the lives of people with disabilities.
Forthcoming.
- United States.Dept.of Health and Human
Services.Office of the Surgeon General. The Surgeon General's call to action to
improve the health and wellness of persons with disabilities. Rockville, MD:
United States. Office of the Surgeon General; 2005.
- Prevalence of regular physical activity
among adults--United States, 2001 and 2005. MMWR Morb.Mortal.Wkly.Rep. 2007 Nov
23;56(46):1209-12.
- Ginis KA, Hicks AL. Considerations for the
development of a physical activity guide for Canadians with physical
disabilities. Can.J.Public Health 2007;98 Suppl 2:S135-S147.
- Centers for Disease Control and Prevention (,
National Center on Birth Defects and Developmental Disabilities (Centers for
Disease Control and Prevention). Disability and health state chartbook, 2006 :
profiles of health for adults with disabilities. Atlanta, GA: U.S. Dept. of
Health & Human Services, Centers for Disease Control and Prevention,
National Center on Birth Defects and Developmental Disabilities; 2006.
- Iezzoni LI, Freedman VA. Turning the disability
tide: the importance of definitions. JAMA 2008 Jan 23;299(3):332-4.
- Getz M, Hutzler Y, Vermeer A. Effects of
aquatic interventions in children with neuromotor impairments: a systematic
review of the literature. Clin.Rehabil. 2006 Nov;20(11):927-36.
- Haskell W. Physical Activity Guidelines
Advisory Committee, Washington, D.C. 2008.
- Chin T, Sawamura S, Fujita H, Nakajima S, Ojima
I, Oyabu H, Nagakura Y, Otsuka H, Nakagawa A. Effect of endurance training
program based on anaerobic threshold (AT) for lower limb amputees.
J.Rehabil.Res.Dev. 2001 Jan;38(1):7-11.
- Chin T, Sawamura S, Fujita H, Nakajima S, Oyabu
H, Nagakura Y, Ojima I, Otsuka H, Nakagawa A. Physical fitness of lower limb
amputees. Am.J.Phys.Med.Rehabil. 2002 May;81(5):321-5.
- Williams H, Pountney T. Effects of a static
bicycling programme on the functional ability of young people with cerebral
palsy who are non-ambulant. Dev.Med.Child Neurol. 2007 Jul;49(7):522-7.
- Bjarnadottir OH, Konradsdottir AD, Reynisdottir
K, Olafsson E. Multiple sclerosis and brief moderate exercise. A randomised
study. Mult.Scler. 2007 Jul;13(6):776-82.
- Mostert S, Kesselring J. Effects of a
short-term exercise training program on aerobic fitness, fatigue, health
perception and activity level of subjects with multiple sclerosis. Mult.Scler.
2002 Apr;8(2):161-8.
- Petajan JH, Gappmaier E, White AT, Spencer MK,
Mino L, Hicks RW. Impact of aerobic training on fitness and quality of life in
multiple sclerosis. Ann.Neurol. 1996 Apr;39(4):432-41.
- Rampello A, Franceschini M, Piepoli M,
Antenucci R, Lenti G, Olivieri D, Chetta A. Effect of aerobic training on
walking capacity and maximal exercise tolerance in patients with multiple
sclerosis: a randomized crossover controlled study. Phys.Ther. 2007
May;87(5):545-55.
- Schulz KH, Gold SM, Witte J, Bartsch K, Lang
UE, Hellweg R, Reer R, Braumann KM, Heesen C. Impact of aerobic training on
immune-endocrine parameters, neurotrophic factors, quality of life and
coordinative function in multiple sclerosis. J.Neurol.Sci. 2004 Oct
15;225(1-2):11-8.
- Rodgers MM, Mulcare JA, King DL, Mathews T,
Gupta SC, Glaser RM. Gait characteristics of individuals with multiple
sclerosis before and after a 6-month aerobic training program.
J.Rehabil.Res.Dev. 1999 Jul;36(3):183-8.
- Rasova K, Havrdova E, Brandejsky P, Zalisova M,
Foubikova B, Martinkova P. Comparison of the influence of different
rehabilitation programmes on clinical, spirometric and spiroergometric
parameters in patients with multiple sclerosis. Mult.Scler. 2006
Apr;12(2):227-34.
- Olsen DB, Orngreen MC, Vissing J. Aerobic
training improves exercise performance in facioscapulohumeral muscular
dystrophy. Neurology 2005 Mar 22;64(6):1064-6.
- Orngreen MC, Olsen DB, Vissing J. Aerobic
training in patients with myotonic dystrophy type 1. Ann.Neurol. 2005
May;57(5):754-7.
- Taivassalo T, De SN, Argov Z, Matthews PM, Chen
J, Genge A, Karpati G, Arnold DL. Effects of aerobic training in patients with
mitochondrial myopathies. Neurology 1998 Apr;50(4):1055-60.
- Taivassalo T, De SN, Chen J, Karpati G, Arnold
DL, Argov Z. Short-term aerobic training response in chronic myopathies. Muscle
Nerve 1999 Sep;22(9):1239-43.
- Wright NC, Kilmer DD, McCrory MA, Aitkens SG,
Holcomb BJ, Bernauer EM. Aerobic walking in slowly progressive neuromuscular
disease: effect of a 12-week program. Arch.Phys.Med.Rehabil. 1996
Jan;77(1):64-9.
- de Groot PC, Hjeltnes N, Heijboer AC, Stal W,
Birkeland K. Effect of training intensity on physical capacity, lipid profile
and insulin sensitivity in early rehabilitation of spinal cord injured
individuals. Spinal Cord. 2003 Dec;41(12):673-9.
- McLean KP, Skinner JS. Effect of body training
position on outcomes of an aerobic training study on individuals with
quadriplegia. Arch.Phys.Med.Rehabil. 1995 Feb;76(2):139-50.
- Bougenot MP, Tordi N, Betik AC, Martin X, Le
FD, Parratte B, Lonsdorfer J, Rouillon JD. Effects of a wheelchair ergometer
training programme on spinal cord-injured persons. Spinal Cord. 2003
Aug;41(8):451-6.
- El-Sayed MS, Younesian A. Lipid profiles are
influenced by arm cranking exercise and training in individuals with spinal
cord injury. Spinal Cord. 2005 May;43(5):299-305.
- Jacobs PL, Nash MS, Rusinowski JW. Circuit
training provides cardiorespiratory and strength benefits in persons with
paraplegia. Med.Sci.Sports Exerc. 2001 May;33(5):711-7.
- Le Foll-de Moro D, Tordi N, Lonsdorfer E,
Lonsdorfer J. Ventilation efficiency and pulmonary function after a wheelchair
interval-training program in subjects with recent spinal cord injury.
Arch.Phys.Med.Rehabil. 2005 Aug;86(8):1582-6.
- Midha M, Schmitt JK, Sclater M. Exercise effect
with the wheelchair aerobic fitness trainer on conditioning and metabolic
function in disabled persons: a pilot study. Arch.Phys.Med.Rehabil. 1999
Mar;80(3):258-61.
- Nash MS, van dV, I, van EN, Johnson BM. Effects
of circuit resistance training on fitness attributes and upper-extremity pain
in middle-aged men with paraplegia. Arch.Phys.Med.Rehabil. 2007
Jan;88(1):70-5.
- Tordi N, Dugue B, Klupzinski D, Rasseneur L,
Rouillon JD, Lonsdorfer J. Interval training program on a wheelchair ergometer
for paraplegic subjects. Spinal Cord. 2001 Oct;39(10):532-7.
- Hjeltnes N, Wallberg-Henriksson H. Improved
work capacity but unchanged peak oxygen uptake during primary rehabilitation in
tetraplegic patients. Spinal Cord. 1998 Oct;36(10):691-8.
- Rodgers MM, Keyser RE, Rasch EK, Gorman PH,
Russell PJ. Influence of training on biomechanics of wheelchair propulsion.
J.Rehabil.Res.Dev. 2001 Sep;38(5):505-11.
- Chu KS, Eng JJ, Dawson AS, Harris JE, Ozkaplan
A, Gylfadottir S. Water-based exercise for cardiovascular fitness in people
with chronic stroke: a randomized controlled trial. Arch.Phys.Med.Rehabil. 2004
Jun;85(6):870-4.
- Duncan P, Studenski S, Richards L, Gollub S,
Lai SM, Reker D, Perera S, Yates J, Koch V, Rigler S, et al. Randomized
clinical trial of therapeutic exercise in subacute stroke. Stroke 2003
Sep;34(9):2173-80.
- Ivey FM, Ryan AS, Hafer-Macko CE, Goldberg AP,
Macko RF. Treadmill aerobic training improves glucose tolerance and indices of
insulin sensitivity in disabled stroke survivors: a preliminary report. Stroke
2007 Oct;38(10):2752-8.
- Pang MY, Eng JJ, Dawson AS, McKay HA, Harris
JE. A community-based fitness and mobility exercise program for older adults
with chronic stroke: a randomized, controlled trial. J.Am.Geriatr.Soc. 2005
Oct;53(10):1667-74.
- Potempa K, Lopez M, Braun LT, Szidon JP, Fogg
L, Tincknell T. Physiological outcomes of aerobic exercise training in
hemiparetic stroke patients. Stroke 1995 Jan;26(1):101-5.
- Rimmer JH, Riley B, Creviston T, Nicola T.
Exercise training in a predominantly African-American group of stroke
survivors. Med.Sci.Sports Exerc. 2000 Dec;32(12):1990-6.
- Macko RF, Smith GV, Dobrovolny CL, Sorkin JD,
Goldberg AP, Silver KH. Treadmill training improves fitness reserve in chronic
stroke patients. Arch.Phys.Med.Rehabil. 2001 Jul;82(7):879-84.
- Driver S, O'connor J, Lox C, Rees K. Evaluation
of an aquatics programme on fitness parameters of individuals with a brain
injury. Brain Inj. 2004 Sep;18(9):847-59.
- Bhambhani Y, Rowland G, Farag M. Effects of
circuit training on body composition and peak cardiorespiratory responses in
patients with moderate to severe traumatic brain injury. Arch.Phys.Med.Rehabil.
2005 Feb;86(2):268-76.
- Arkin SM. Student-led exercise sessions yield
significant fitness gains for Alzheimer's patients. Am.J.Alzheimers.Dis.Other
Demen. 2003 May;18(3):159-70.
- Heyn P. The effect of a multisensory exercise
program on engagement, behavior, and selected physiological indexes in persons
with dementia. Am.J.Alzheimers.Dis.Other Demen. 2003 Jul;18(4):247-51.
- Rimmer JH, Heller T, Wang E, Valerio I.
Improvements in physical fitness in adults with Down syndrome.
Am.J.Ment.Retard. 2004 Mar;109(2):165-74.
- Varela AM, Sardinha LB, Pitetti KH. Effects of
an aerobic rowing training regimen in young adults with Down syndrome.
Am.J.Ment.Retard. 2001 Mar;106(2):135-44.
- Cluphf D, O'connor J, Vanin S. Effects of
aerobic dance on the cardiovascular endurance of adults with intellectual
disabilities. Adapt.Phys.Activ.Q. 2001;18(1):60-71.
- Halle JW, Gabler-Halle D, Chung YB. Effects of
a peer-mediated aerobic conditioning program on fitness levels of youth with
mental retardation: two systematic replications. Ment.Retard. 1999
Dec;37(6):435-48.
- Blumenthal JA, Babyak MA, Doraiswamy PM,
Watkins L, Hoffman BM, Barbour KA, Herman S, Craighead WE, Brosse AL, Waugh R,
et al. Exercise and pharmacotherapy in the treatment of major depressive
disorder. Psychosom.Med. 2007 Sep;69(7):587-96.
- Blumenthal JA, Babyak MA, Moore KA, Craighead
WE, Herman S, Khatri P, Waugh R, Napolitano MA, Forman LM, Appelbaum M, et al.
Effects of exercise training on older patients with major depression.
Arch.Intern.Med. 1999 Oct 25;159(19):2349-56.
- Knubben K, Reischies FM, Adli M, Schlattmann P,
Bauer M, Dimeo F. A randomised, controlled study on the effects of a short-term
endurance training programme in patients with major depression. Br.J.Sports
Med. 2007 Jan;41(1):29-33.
- Coyle CP, Santiago MC. Aerobic exercise
training and depressive symptomatology in adults with physical disabilitie.
Arch.Phys.Med.Rehabil. 1995 Jul;76(7):647-52.
- Fragala-Pinkham MA, Haley SM, Goodgold S.
Evaluation of a community-based group fitness program for children with
disabilities. Pediatr.Phys.Ther. 2006;18(2):159-67.
- White LJ, Castellano V, Mc Coy SC. Cytokine
responses to resistance training in people with multiple sclerosis. J.Sports
Sci. 2006 Aug;24(8):911-4.
- Eberhard Y, Eterradossi J, Debu B. Biological
changes induced by physical activity in individuals with Down's syndrome.
Adapt.Phys.Activ.Q. 1997;14(2):166-75.
- Wu MK, Wang CK, Bai YM, Huang CY, Lee SD.
Outcomes of obese, clozapine-treated inpatients with schizophrenia placed on a
six-month diet and physical activity program. Psychiatr.Serv. 2007
Apr;58(4):544-50.
- Dodd KJ, Taylor NF, Graham HK. A randomized
clinical trial of strength training in young people with cerebral palsy.
Dev.Med.Child Neurol. 2003 Oct;45(10):652-7.
- Patikas D, Wolf SI, Armbrust P, Mund K,
Schuster W, Dreher T, Doderlein L. Effects of a postoperative resistive
exercise program on the knee extension and flexion torque in children with
cerebral palsy: a randomized clinical trial. Arch.Phys.Med.Rehabil. 2006
Sep;87(9):1161-9.
- Andersson C, Grooten W, Hellsten M, Kaping K,
Mattsson E. Adults with cerebral palsy: walking ability after progressive
strength training. Dev.Med.Child Neurol. 2003 Apr;45(4):220-8.
- Blundell SW, Shepherd RB, Dean CM, Adams RD,
Cahill BM. Functional strength training in cerebral palsy: a pilot study of a
group circuit training class for children aged 4-8 years. Clin.Rehabil. 2003
Feb;17(1):48-57.
- Damiano DL, Abel MF. Functional outcomes of
strength training in spastic cerebral palsy. Arch.Phys.Med.Rehabil. 1998
Feb;79(2):119-25.
- Morton JF, Brownlee M, McFadyen AK. The effects
of progressive resistance training for children with cerebral palsy.
Clin.Rehabil. 2005 May;19(3):283-9.
- Taylor NF, Dodd KJ, Larkin H. Adults with
cerebral palsy benefit from participating in a strength training programme at a
community gymnasium. Disabil.Rehabil. 2004 Oct 7;26(19):1128-34.
- DeBolt LS, McCubbin JA. The effects of
home-based resistance exercise on balance, power, and mobility in adults with
multiple sclerosis. Arch.Phys.Med.Rehabil. 2004 Feb;85(2):290-7.
- White LJ, McCoy SC, Castellano V, Gutierrez G,
Stevens JE, Walter GA, Vandenborne K. Resistance training improves strength and
functional capacity in persons with multiple sclerosis. Mult.Scler. 2004
Dec;10(6):668-74.
- van der Kooi EL, Vogels OJ, van Asseldonk RJ,
Lindeman E, Hendriks JC, Wohlgemuth M, van der Maarel SM, Padberg GW. Strength
training and albuterol in facioscapulohumeral muscular dystrophy. Neurology
2004 Aug 24;63(4):702-8.
- Lindeman E, Spaans F, Reulen J, Leffers P,
Drukker J. Progressive resistance training in neuromuscular patients. Effects
on force and surface EMG. J.Electromyogr.Kinesiol. 1999 Dec;9(6):379-84.
- Tollback A, Eriksson S, Wredenberg A, Jenner G,
Vargas R, Borg K, Ansved T. Effects of high resistance training in patients
with myotonic dystrophy. Scand.J.Rehabil.Med. 1999 Mar;31(1):9-16.
- Hirsch MA, Toole T, Maitland CG, Rider RA. The
effects of balance training and high-intensity resistance training on persons
with idiopathic Parkinson's disease. Arch.Phys.Med.Rehabil. 2003
Aug;84(8):1109-17.
- Dibble LE, Hale T, Marcus RL, Gerber JP,
Lastayo PC. The safety and feasibility of high-force eccentric resistance
exercise in persons with Parkinson's disease. Arch.Phys.Med.Rehabil. 2006
Sep;87(9):1280-2.
- Hicks AL, Martin KA, Ditor DS, Latimer AE,
Craven C, Bugaresti J, McCartney N. Long-term exercise training in persons with
spinal cord injury: effects on strength, arm ergometry performance and
psychological well-being. Spinal Cord. 2003 Jan;41(1):34-43.
- Duran FS, Lugo L, Ramirez L, Eusse E. Effects
of an exercise program on the rehabilitation of patients with spinal cord
injury. Arch.Phys.Med.Rehabil. 2001 Oct;82(10):1349-54.
- Ouellette MM, LeBrasseur NK, Bean JF, Phillips
E, Stein J, Frontera WR, Fielding RA. High-intensity resistance training
improves muscle strength, self-reported function, and disability in long-term
stroke survivors. Stroke 2004 Jun;35(6):1404-9.
- Teixeira-Salmela LF, Olney SJ, Nadeau S,
Brouwer B. Muscle strengthening and physical conditioning to reduce impairment
and disability in chronic stroke survivors. Arch.Phys.Med.Rehabil. 1999
Oct;80(10):1211-8.
- Sharp SA, Brouwer BJ. Isokinetic strength
training of the hemiparetic knee: effects on function and spasticity.
Arch.Phys.Med.Rehabil. 1997 Nov;78(11):1231-6.
- Smith GV, Silver KH, Goldberg AP, Macko RF.
"Task-oriented" exercise improves hamstring strength and spastic reflexes in
chronic stroke patients. Stroke 1999 Oct;30(10):2112-8.
- Weiss A, Suzuki T, Bean J, Fielding RA. High
intensity strength training improves strength and functional performance after
stroke. Am.J.Phys.Med.Rehabil. 2000 Jul;79(4):369-76.
- Driver S, Rees K, O'connor J, Lox C. Aquatics,
health-promoting self-care behaviours and adults with brain injuries. Brain
Inj. 2006 Feb;20(2):133-41.
- Romberg A, Virtanen A, Ruutiainen J. Long-term
exercise improves functional impairment but not quality of life in multiple
sclerosis. J.Neurol. 2005 Jul;252(7):839-45.
- Tsimaras VK, Fotiadou EG. Effect of training on
the muscle strength and dynamic balance ability of adults with down syndrome.
J.Strength.Cond.Res. 2004 May;18(2):343-7.
- Podgorski CA, Kessler K, Cacia B, Peterson DR,
Henderson CM. Physical activity intervention for older adults with intellectual
disability: report on a pilot project. Ment.Retard. 2004 Aug;42(4):272-83.
- O'Connell DG, Barnhart R. Improvement in
wheelchair propulsion in pediatric wheelchair users through resistance
training: a pilot study. Arch.Phys.Med.Rehabil. 1995 Apr;76(4):368-72.
- Husted C, Pham L, Hekking A, Niederman R.
Improving quality of life for people with chronic conditions: the example of
t'ai chi and multiple sclerosis. Altern.Ther.Health Med. 1999
Sep;5(5):70-4.
- Schenkman M, Cutson TM, Kuchibhatla M, Chandler
J, Pieper CF, Ray L, Laub KC. Exercise to improve spinal flexibility and
function for people with Parkinson's disease: a randomized, controlled trial.
J.Am.Geriatr.Soc. 1998 Oct;46(10):1207-16.
- Jeong S, Kim MT. Effects of a theory-driven
music and movement program for stroke survivors in a community setting.
Appl.Nurs.Res. 2007 Aug;20(3):125-31.
- Chad KE, Bailey DA, McKay HA, Zello GA, Snyder
RE. The effect of a weight-bearing physical activity program on bone mineral
content and estimated volumetric density in children with spastic cerebral
palsy. J.Pediatr. 1999 Jul;135(1):115-7.
- Patikas D, Wolf SI, Mund K, Armbrust P,
Schuster W, Doderlein L. Effects of a postoperative strength-training program
on the walking ability of children with cerebral palsy: a randomized controlled
trial. Arch.Phys.Med.Rehabil. 2006 May;87(5):619-26.
- Romberg A, Virtanen A, Ruutiainen J, Aunola S,
Karppi SL, Vaara M, Surakka J, Pohjolainen T, Seppanen A. Effects of a 6-month
exercise program on patients with multiple sclerosis: a randomized study.
Neurology 2004 Dec 14;63(11):2034-8.
- van den BM, Dawes H, Wade DT, Newman M,
Burridge J, Izadi H, Sackley CM. Treadmill training for individuals with
multiple sclerosis: a pilot randomised trial. J.Neurol.Neurosurg.Psychiatry
2006 Apr;77(4):531-3.
- Newman MA, Dawes H, van den BM, Wade DT,
Burridge J, Izadi H. Can aerobic treadmill training reduce the effort of
walking and fatigue in people with multiple sclerosis: a pilot study.
Mult.Scler. 2007 Jan;13(1):113-9.
- Mount J, Dacko S. Effects of dorsiflexor
endurance exercises on foot drop secondary to multiple sclerosis: a pilot
study. NeuroRehabilitation. 2006;21(1):43-50.
- Cakit BD, Saracoglu M, Genc H, Erdem HR, Inan
L. The effects of incremental speed-dependent treadmill training on postural
instability and fear of falling in Parkinson's disease. Clin.Rehabil. 2007
Aug;21(8):698-705.
- Caglar AT, Gurses HN, Mutluay FK, Kiziltan G.
Effects of home exercises on motor performance in patients with Parkinson's
disease. Clin.Rehabil. 2005 Dec;19(8):870-7.
- Herman T, Giladi N, Gruendlinger L, Hausdorff
JM. Six weeks of intensive treadmill training improves gait and quality of life
in patients with Parkinson's disease: a pilot study. Arch.Phys.Med.Rehabil.
2007 Sep;88(9):1154-8.
- Ada L, Dean CM, Hall JM, Bampton J, Crompton S.
A treadmill and overground walking program improves walking in persons residing
in the community after stroke: a placebo-controlled, randomized trial.
Arch.Phys.Med.Rehabil. 2003 Oct;84(10):1486-91.
- Dean CM, Richards CL, Malouin F. Task-related
circuit training improves performance of locomotor tasks in chronic stroke: a
randomized, controlled pilot trial. Arch.Phys.Med.Rehabil. 2000
Apr;81(4):409-17.
- Duncan P, Richards L, Wallace D, Stoker-Yates
J, Pohl P, Luchies C, Ogle A, Studenski S. A randomized, controlled pilot study
of a home-based exercise program for individuals with mild and moderate stroke.
Stroke 1998 Oct;29(10):2055-60.
- Katz-Leurer M, Carmeli E, Shochina M. The
effect of early aerobic training on independence six months post stroke.
Clin.Rehabil. 2003 Nov;17(7):735-41.
- Studenski S, Duncan PW, Perera S, Reker D, Lai
SM, Richards L. Daily functioning and quality of life in a randomized
controlled trial of therapeutic exercise for subacute stroke survivors. Stroke
2005 Aug;36(8):1764-70.
- Eng JJ, Chu KS, Kim CM, Dawson AS, Carswell A,
Hepburn KE. A community-based group exercise program for persons with chronic
stroke. Med.Sci.Sports Exerc. 2003 Aug;35(8):1271-8.
- Leroux A. Exercise training to improve motor
performance in chronic stroke: effects of a community-based exercise program.
Int.J.Rehabil.Res. 2005 Mar;28(1):17-23.
- Rolland Y, Pillard F, Klapouszczak A, Reynish
E, Thomas D, Andrieu S, Riviere D, Vellas B. Exercise program for nursing home
residents with Alzheimer's disease: a 1-year randomized, controlled trial.
J.Am.Geriatr.Soc. 2007 Feb;55(2):158-65.
- Carmeli E, Barchad S, Masharawi Y, Coleman R.
Impact of a walking program in people with down syndrome. J.Strength.Cond.Res.
2004 Feb;18(1):180-4.
- Carmeli E, Kessel S, Coleman R, Ayalon M.
Effects of a treadmill walking program on muscle strength and balance in
elderly people with Down syndrome. J.Gerontol.A Biol.Sci.Med.Sci. 2002
Feb;57(2):M106-M110.
- Carmeli E, Merrick J, Berner YN. Effect of
training on health and functional status in older adults with intellectural
disability. Int.J.Ther.Rehabil. 2004;11(10):481-5.
- Bateman A, Culpan FJ, Pickering AD, Powell JH,
Scott OM, Greenwood RJ. The effect of aerobic training on rehabilitation
outcomes after recent severe brain injury: a randomized controlled evaluation.
Arch.Phys.Med.Rehabil. 2001 Feb;82(2):174-82.
- van den BM, Dawes H, Wade DT, Newman M,
Burridge J, Izadi H, Sackley CM. Treadmill training for individuals with
multiple sclerosis: a pilot randomised trial. J.Neurol.Neurosurg.Psychiatry
2006 Apr;77(4):531-3.
- Dibble LE, Hale TF, Marcus RL, Droge J, Gerber
JP, Lastayo PC. High-intensity resistance training amplifies muscle hypertrophy
and functional gains in persons with Parkinson's disease. Mov Disord. 2006
Sep;21(9):1444-52.
- Cott CA, Dawson P, Sidani S, Wells D. The
effects of a walking/talking program on communication, ambulation, and
functional status in residents with Alzheimer disease. Alzheimer
Dis.Assoc.Disord. 2002 Apr;16(2):81-7.
- Beebe LH, Tian L, Morris N, Goodwin A, Allen
SS, Kuldau J. Effects of exercise on mental and physical health parameters of
persons with schizophrenia. Issues Ment.Health Nurs. 2005
Jul;26(6):661-76.
- Oken BS, Kishiyama S, Zajdel D, Bourdette D,
Carlsen J, Haas M, Hugos C, Kraemer DF, Lawrence J, Mass M. Randomized
controlled trial of yoga and exercise in multiple sclerosis. Neurology 2004 Jun
8;62(11):2058-64.
- Wenneberg S, Gunnarsson LG, Ahlstrom G. Using
a novel exercise programme for patients with muscular dystrophy. Part II: a
quantitative study. Disabil.Rehabil. 2004 May 20;26(10):595-602.
- van der Kooi EL, Kalkman JS, Lindeman E,
Hendriks JC, van Engelen BG, Bleijenberg G, Padberg GW. Effects of training and
albuterol on pain and fatigue in facioscapulohumeral muscular dystrophy.
J.Neurol. 2007 Jul;254(7):931-40.
- Ashburn A, Fazakarley L, Ballinger C,
Pickering R, McLellan LD, Fitton C. A randomised controlled trial of a home
based exercise programme to reduce the risk of falling among people with
Parkinson's disease. J.Neurol.Neurosurg.Psychiatry 2007 Jul;78(7):678-84.
- Rodrigues de Paula F, Teixeira-Salmela LF,
Coelho de Morais Faria CD, Rocha de BP, Cardoso F. Impact of an exercise
program on physical, emotional, and social aspects of quality of life of
individuals with Parkinson's disease. Mov Disord. 2006 Aug;21(8):1073-7.
- Reuter I, Engelhardt M, Stecker K, Baas H.
Therapeutic value of exercise training in Parkinson's disease. Med.Sci.Sports
Exerc. 1999 Nov;31(11):1544-9.
- Ginis KAM, Latimer AE, McKechnie K, Ditor DS,
McCartney N, Hicks AL, Bugaresti J, Craven BC. Using exercise to enhance
subjective well-being among people with spinal cord injury: the mediating
influences of stress and pain. Rehabil.Psychol. 2003;48(3):157-64.
- Lai SM, Studenski S, Richards L, Perera S,
Reker D, Rigler S, Duncan PW. Therapeutic exercise and depressive symptoms
after stroke. J.Am.Geriatr.Soc. 2006 Feb;54(2):240-7.
- Teri L, Gibbons LE, McCurry SM, Logsdon RG,
Buchner DM, Barlow WE, Kukull WA, LaCroix AZ, McCormick W, Larson EB. Exercise
plus behavioral management in patients with Alzheimer disease: a randomized
controlled trial. JAMA 2003 Oct 15;290(15):2015-22.
- Heller T, Hsieh K, Rimmer JH. Attitudinal and
psychosocial outcomes of a fitness and health education program on adults with
down syndrome. Am.J.Ment.Retard. 2004 Mar;109(2):175-85.
- Skrinar GS, Huxley NA, Hutchinson DS,
Menninger E, Glew P. The role of a fitness intervention on people with serious
psychiatric disabilities. Psychiatr.Rehabil.J. 2005;29(2):122-7.
- Trivedi MH, Greer TL, Grannemann BD, Chambliss
HO, Jordan AN. Exercise as an augmentation strategy for treatment of major
depression. J.Psychiatr.Pract. 2006 Jul;12(4):205-13.
- Schmitz-Hubsch T, Pyfer D, Kielwein K, Fimmers
R, Klockgether T, Wullner U. Qigong exercise for the symptoms of Parkinson's
disease: a randomized, controlled pilot study. Mov Disord. 2006
Apr;21(4):543-8.
- Baatile J, Langbein WE, Weaver F, Maloney C,
Jost MB. Effect of exercise on perceived quality of life of individuals with
Parkinson's disease. J.Rehabil.Res.Dev. 2000 Sep;37(5):529-34.
- Lun V, Pullan N, Labelle N, Adams C,
Suchowersky O. Comparison of the effects of a self-supervised home exercise
program with a physiotherapist-supervised exercise program on the motor
symptoms of Parkinson's disease. Mov Disord. 2005 Aug;20(8):971-5.
- Viliani T, Pasquetti P, Magnolfi S, Lunardelli
ML, Giorgi C, Serra P, Taiti PG. Effects of physical training on
straightening-up processes in patients with Parkinson's disease.
Disabil.Rehabil. 1999 Feb;21(2):68-73.
- Pang MY, Harris JE, Eng JJ. A community-based
upper-extremity group exercise program improves motor function and performance
of functional activities in chronic stroke: a randomized controlled trial.
Arch.Phys.Med.Rehabil. 2006 Jan;87(1):1-9.
- Grigorenko A, Bjerkefors A, Rosdahl H,
Hultling C, Alm M, Thorstensson A. Sitting balance and effects of kayak
training in paraplegics. J.Rehabil.Med. 2004 May;36(3):110-6.
- Laufer Y, Dickstein R, Chefez Y, Marcovitz E.
The effect of treadmill training on the ambulation of stroke survivors in the
early stages of rehabilitation: a randomized study. J.Rehabil.Res.Dev. 2001
Jan;38(1):69-78.
- Surakka J, Romberg A, Ruutiainen J, Aunola S,
Virtanen A, Karppi SL, Maentaka K. Effects of aerobic and strength exercise on
motor fatigue in men and women with multiple sclerosis: a randomized controlled
trial. Clin.Rehabil. 2004 Nov;18(7):737-46.
- van den BM, Dawes H, Wade DT, Newman M,
Burridge J, Izadi H, Sackley CM. Treadmill training for individuals with
multiple sclerosis: a pilot randomised trial. J.Neurol.Neurosurg.Psychiatry
2006 Apr;77(4):531-3.
- Ball MP, Coons VB, Buchanan RW. A program for
treating olanzapine-related weight gain. Psychiatr.Serv. 2001
Jul;52(7):967-9.
- Nawoczenski DA, Ritter-Soronen JM, Wilson CM,
Howe BA, Ludewig PM. Clinical trial of exercise for shoulder pain in chronic
spinal injury. Phys.Ther. 2006 Dec;86(12):1604-18.
- Kilmer DD, Wright NC, Aitkens S. Impact of a
home-based activity and dietary intervention in people with slowly progressive
neuromuscular diseases. Arch.Phys.Med.Rehabil. 2005 Nov;86(11):2150-6.
- Bizzarini E, Saccavini M, Lipanje F, Magrin P,
Malisan C, Zampa A. Exercise prescription in subjects with spinal cord
injuries. Arch.Phys.Med.Rehabil. 2005 Jun;86(6):1170-5.
- Brown C, Goetz J, Van SA, Sullivan D, Hamera
E. A psychiatric rehabilitation approach to weight loss. Psychiatr.Rehabil.J.
2006;29(4):267-73.
- Vreeland B, Minsky S, Menza M, Rigassio RD,
Roemheld-Hamm B, Stern R. A program for managing weight gain associated with
atypical antipsychotics. Psychiatr.Serv. 2003 Aug;54(8):1155-7.
- McCurry SM, Gibbons LE, Logsdon RG, Vitiello
MV, Teri L. Nighttime insomnia treatment and education for Alzheimer's disease:
a randomized, controlled trial. J.Am.Geriatr.Soc. 2005 May;53(5):793-802.
- Babyak M, Blumenthal JA, Herman S, Khatri P,
Doraiswamy M, Moore K, Craighead WE, Baldewicz TT, Krishnan KR. Exercise
treatment for major depression: maintenance of therapeutic benefit at 10
months. Psychosom.Med. 2000 Sep;62(5):633-8.
- Dunn AL, Trivedi MH, Kampert JB, Clark CG,
Chambliss HO. Exercise treatment for depression: efficacy and dose response.
Am.J.Prev.Med. 2005 Jan;28(1):1-8.
- Duraiswamy G, Thirthalli J, Nagendra HR,
Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients
with schizophrenia--a randomized controlled trial. Acta Psychiatr.Scand. 2007
Sep;116(3):226-32.
- Janakiramaiah N, Gangadhar BN, Naga Venkatesha
Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant
efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: a randomized comparison
with electroconvulsive therapy (ECT) and imipramine. J.Affect.Disord. 2000
Jan;57(1-3):255-9.
- De Mello MT, Esteves AM, Tufik S. Comparison
between dopaminergic agents and physical exercise as treatment for periodic
limb movements in patients with spinal cord injury. Spinal Cord. 2004
Apr;42(4):218-21.
- McDevitt J, Wilbur J, Kogan J, Briller J. A
walking program for outpatients in psychiatric rehabilitation: pilot study.
Biol.Res.Nurs. 2005 Oct;7(2):87-97.
- Office for Human Research Protections (OHRP).
Guidance on Reviewing and Reporting Unanticipated Problems Involving Risks to
Subjects or Others and Adverse Events 2007 [cited 2008 Jan 31].
- Moore GE, Durstine JL, Marsh AP. Framework.
In: Durstine JL, Moore GE, editors. ACSM's Exercise Managment for Persons with
Chronic Diseases and Disabilities. Champaign, IL: Human Kinetics; 2002. p.
5-15.
- Lindeman E, Leffers P, Spaans F, Drukker J,
Reulen J, Kerckhoffs M, Koke A. Strength training in patients with myotonic
dystrophy and hereditary motor and sensory neuropathy: a randomized clinical
trial. Arch.Phys.Med.Rehabil. 1995 Jul;76(7):612-20.
- Dodd KJ, Taylor NF, Graham HK. Strength
training can have unexpected effects on the self-concept of children with
cerebral palsy. Pediatr.Phys.Ther. 2004;16(2):99-105.
- Ninot G, Bilard J, Delignieres D. Effects of
integrated or segregated sport participation on the physical self for
adolescents with intellectual disabilities. J.Intellect.Disabil.Res. 2005
Sep;49(Pt 9):682-9.
- United States.Public Health Service.Office of
the Surgeon General., National Center for Chronic Disease Prevention and Health
Promotion (, President's Council on Physical Fitness and Sports (. Physical
activity and health : a report of the Surgeon General. Atlanta, Ga.;
[Washington, D.C.]; Pittsburgh, PA: U.S. Dept. of Health and Human Services,
Centers for Disease Control and Prevention, National Center for Chronic Disease
Prevention and Health Promotion ; President's Council on Physical Fitness and
Sports ; For sale by the Supt. of Docs.; 1996.
- World Health Organization. International
classification of functioning, disability and health : ICF. Geneva: World
Health Organization; 2001.
- Exercise during pregnancy and the
postnatal period. ACOG Technical Bulletin - 1985. Washington,D.C.: American
College of Obstetricians and Gynecologists; 1985.
- American College of Obstetricians and
Gynecologists. Women and Exercise. Washington, D.C.: American College of
Obstetricians and Gynecologists; 1994.
- ACOG Committee opinion. Number 267,
January 2002: exercise during pregnancy and the postpartum period.
Obstet.Gynecol. 2002 Jan;99(1):171-3.
- Pivarnik J. Physical activity during pregnancy
and the postpartum period. In: Institute of Medicine, editor. Adequacy of
Evidence for Physical Activity Guidelines Development: Workshop Summary.
Washington, DC: National Academies Press; 2006. p. 102-5.
- Hegaard HK, Pedersen BK, Nielsen BB, Damm P.
Leisure time physical activity during pregnancy and impact on gestational
diabetes mellitus, pre-eclampsia, preterm delivery and birth weight: a review.
Acta Obstet.Gynecol.Scand. 2007;86(11):1290-6.
- Morris SN, Johnson NR. Exercise during
pregnancy: a critical appraisal of the literature. J.Reprod.Med. 2005
Mar;50(3):181-8.
- Leet T, Flick L. Effect of exercise on
birthweight. Clin.Obstet.Gynecol. 2003 Jun;46(2):423-31.
- Evenson KR, Siega-Riz AM, Savitz DA, Leiferman
JA, Thorp JM, Jr. Vigorous leisure activity and pregnancy outcome. Epidemiology
2002 Nov;13(6):653-9.
- Duncombe D, Skouteris H, Wertheim EH, Kelly L,
Fraser V, Paxton SJ. Vigorous exercise and birth outcomes in a sample of
recreational exercisers: a prospective study across pregnancy.
Aust.N.Z.J.Obstet.Gynaecol. 2006 Aug;46(4):288-92.
- Impact of physical activity during
pregnancy and postpartum on chronic disease risk. Med.Sci.Sports Exerc. 2006
May;38(5):989-1006.
- Marcoux S, Brisson J, Fabia J. The effect of
leisure time physical activity on the risk of pre-eclampsia and gestational
hypertension. J.Epidemiol.Community Health 1989 Jun;43(2):147-52.
- Sorensen TK, Williams MA, Lee IM, Dashow EE,
Thompson ML, Luthy DA. Recreational physical activity during pregnancy and risk
of preeclampsia. Hypertension 2003 Jun;41(6):1273-80.
- Saftlas AF, Logsden-Sackett N, Wang W, Woolson
R, Bracken MB. Work, leisure-time physical activity, and risk of preeclampsia
and gestational hypertension. Am.J.Epidemiol. 2004 Oct 15;160(8):758-65.
- Meher S, Duley L. Exercise or other physical
activity for preventing pre-eclampsia and its complications.
Cochrane.Database.Syst.Rev. 2006;(2):CD005942.
- Ceysens G, Rouiller D, Boulvain M. Exercise
for diabetic pregnant women. Cochrane.Database.Syst.Rev. 2006;3:CD004225.
- Dempsey JC, Butler CL, Williams MA. No need
for a pregnant pause: physical activity may reduce the occurrence of
gestational diabetes mellitus and preeclampsia. Exerc.Sport Sci.Rev. 2005
Jul;33(3):141-9.
- Zhang C, Solomon CG, Manson JE, Hu FB. A
prospective study of pregravid physical activity and sedentary behaviors in
relation to the risk for gestational diabetes mellitus. Arch.Intern.Med. 2006
Mar 13;166(5):543-8.
- Kramer MS, McDonald SW. Aerobic exercise for
women during pregnancy. Cochrane.Database.Syst.Rev. 2006;3:CD000180.
- Poudevigne MS, O'Connor PJ. A review of
physical activity patterns in pregnant women and their relationship to
psychological health. Sports Med. 2006;36(1):19-38.
- Hegaard HK, Hedegaard M, Damm P, Ottesen B,
Petersson K, Henriksen TB. Leisure time physical activity is associated with a
reduced risk of preterm delivery. Am.J.Obstet.Gynecol. 2008
Feb;198(2):180-5.
- Daley AJ, Macarthur C, Winter H. The role of
exercise in treating postpartum depression: a review of the literature.
J.Midwifery Womens Health 2007 Jan;52(1):56-62.
- Larson-Meyer DE. Effect of postpartum exercise
on mothers and their offspring: a review of the literature. Obes.Res. 2002
Aug;10(8):841-53.
- Amorim AR, Linne YM, Lourenco PM. Diet or
exercise, or both, for weight reduction in women after childbirth.
Cochrane.Database.Syst.Rev. 2007;(3):CD005627.
- Rooney BL, Schauberger CW, Mathiason MA.
Impact of perinatal weight change on long-term obesity and obesity-related
illnesses. Obstet.Gynecol. 2005 Dec;106(6):1349-56.
- McCrory MA. Aerobic exercise during lactation:
safe, healthful, and compatible. J.Hum.Lact. 2000 May;16(2):95-8.
- Banks-Wallace J, Conn V. Interventions to
promote physical activity among African American women. Public Health Nurs.
2002 Sep;19(5):321-35.
- Eyler AE, Wilcox S, Matson-Koffman D, Evenson
KR, Sanderson B, Thompson J, Wilbur J, Rohm-Young D. Correlates of physical
activity among women from diverse racial/ethnic groups. J.Womens Health
Gend.Based.Med. 2002 Apr;11(3):239-53.
- Kumanyika S. The minority factor in the
obesity epidemic. Ethn.Dis. 2002;12(3):316-9.
- Yancey AK, Kumanyika SK, Ponce NA, McCarthy
WJ, Fielding JE, Leslie JP, Akbar J. Population-based interventions engaging
communities of color in healthy eating and active living: a review 152.
Prev.Chronic.Dis. 2004 Jan;1(1):A09.
- Yancey AK, Wold CM, McCarthy WJ, Weber MD, Lee
B, Simon PA, Fielding JE. Physical inactivity and overweight among Los Angeles
County adults 153. Am.J.Prev.Med. 2004 Aug;27(2):146-52.
- Gibson CA, Kirk EP, LeCheminant JD, Bailey BW,
Jr., Huang G, Donnelly JE. Reporting quality of randomized trials in the diet
and exercise literature for weight loss 46. BMC.Med.Res.Methodol. 2005 Feb
23;5(1):9.
- Kumanyika SK. Minisymposium on obesity:
overview and some strategic considerations 75. Annu.Rev.Public Health
2001;22:293-308.
- Backman DR, Carman JS, Aldan SG. Fruits and
vegetables and physical activity at the worksite: business leaders and working
women speak out on access and environment. Sacramento, CA: California
Department of Health Services; 2004.
- Day K. Active living and social justice:
planning for physical activity in low-income, black, and latino communities.
J.Am.Plan.Assoc. 2006;71(1):88-99.
- Gordon-Larsen P, Nelson MC, Page P, Popkin BM.
Inequality in the built environment underlies key health disparities in
physical activity and obesity. Pediatrics 2006 Feb;117(2):417-24.
- Powell LM, Slater S, Chaloupka FJ, Harper D.
Availability of physical activity-related facilities and neighborhood
demographic and socioeconomic characteristics: a national study. Am.J.Public
Health 2006 Sep;96(9):1676-80.
- Yancey AK, Ory MG, Davis SM. Dissemination of
physical activity promotion interventions in underserved populations.
Am.J.Prev.Med. 2006 Oct;31(4 Suppl):S82-S91.
- Marshall SJ, Jones DA, Ainsworth BE, Reis JP,
Levy SS, Macera CA. Race/ethnicity, social class, and leisure-time physical
inactivity. Med.Sci.Sports Exerc. 2007 Jan;39(1):44-51.
- Kalter-Leibovici O, Atamna A, Lubin F, Alpert
G, Keren MG, Murad H, Chetrit A, Goffer D, Eilat-Adar S, Goldbourt U. Obesity
among Arabs and Jews in Israel: a population-based study. Isr.Med.Assoc.J. 2007
Jul;9(7):525-30.
- Matthews CE, Chen KY, Freedson PS, Buchowski
MS, Beech BM, Pate RR, Troiano RP. Amount of time spent in sedentary behaviors
in the United States, 2003-2004. Am.J.Epidemiol. 2008 Apr 1;167(7):875-81.
- Troiano RP, Berrigan D, Dodd KW, Masse LC,
Tilert T, McDowell M. Physical activity in the United States measured by
accelerometer. Med.Sci.Sports Exerc. 2008 Jan;40(1):181-8.
- Adams PF, Schoenborn CA. Health behaviors of
adults: United States, 2002-04. Vital Health Stat.10 2006 Sep;(230):1-140.
- Ogden CL, Carroll MD, Curtin LR, McDowell MA,
Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States,
1999-2004 96. JAMA 2006 Apr 5;295(13):1549-55.
- Wang Y, Beydoun MA. The obesity epidemic in
the United States--gender, age, socioeconomic, racial/ethnic, and geographic
characteristics: a systematic review and meta-regression analysis.
Epidemiol.Rev. 2007;29:6-28.
- Yancey A, Bastani R, Glenn B. Racial/ethnic
disparities in health status. In: Andersen R, Rice TH, Kominski GF, editors.
Changing the U.S. health care system: key issues in health services, policy and
management. 3rd ed. Jossey-Bass; 2007.
- He XZ, Baker DW. Differences in leisure-time,
household, and work-related physical activity by race, ethnicity, and
education. J.Gen.Intern.Med. 2005 Mar;20(3):259-66.
- Sternfeld B, Cauley J, Harlow S, Liu G, Lee M.
Assessment of physical activity with a single global question in a large,
multiethnic sample of midlife women 125. Am.J.Epidemiol. 2000 Oct
1;152(7):678-87.
- Gregg EW, Gerzoff RB, Caspersen CJ, Williamson
DF, Narayan KM. Relationship of walking to mortality among US adults with
diabetes 22. Arch.Intern.Med. 2003 Jun 23;163(12):1440-7.
- Ostbye T, Taylor DH, Jung SH. A longitudinal
study of the effects of tobacco smoking and other modifiable risk factors on
ill health in middle-aged and old Americans: results from the Health and
Retirement Study and Asset and Health Dynamics among the Oldest Old survey 55.
Prev.Med. 2002 Mar;34(3):334-45.
- Richardson CR, Kriska AM, Lantz PM, Hayward
RA. Physical activity and mortality across cardiovascular disease risk groups
56. Med.Sci.Sports Exerc. 2004 Nov;36(11):1923-9.
- Manini TM, Everhart JE, Patel KV, Schoeller
DA, Colbert LH, Visser M, Tylavsky F, Bauer DC, Goodpaster BH, Harris TB. Daily
activity energy expenditure and mortality among older adults 49. JAMA 2006 Jul
12;296(2):171-9.
- Crespo CJ, Palmieri MR, Perdomo RP, Mcgee DL,
Smit E, Sempos CT, Lee IM, Sorlie PD. The relationship of physical activity and
body weight with all-cause mortality: results from the Puerto Rico Heart Health
Program 12. Ann.Epidemiol. 2002 Nov;12(8):543-52.
- Hakim AA, Petrovitch H, Burchfiel CM, Ross GW,
Rodriguez BL, White LR, Yano K, Curb JD, Abbott RD. Effects of walking on
mortality among nonsmoking retired men 24. N.Engl.J.Med. 1998 Jan
8;338(2):94-9.
- Fujita K, Takahashi H, Miura C, Ohkubo T, Sato
Y, Ugajin T, Kurashima K, Tsubono Y, Tsuji I, Fukao A, et al. Walking and
mortality in Japan: the Miyagi Cohort Study 20. J.Epidemiol. 2004 Feb;14 Suppl
1:S26-S32.
- Lam TH, Ho SY, Hedley AJ, Mak KH, Leung GM.
Leisure time physical activity and mortality in Hong Kong: case-control study
of all adult deaths in 1998 40. Ann.Epidemiol. 2004 Jul;14(6):391-8.
- Lan TY, Chang HY, Tai TY. Relationship between
components of leisure physical activity and mortality in Taiwanese older adults
41. Prev.Med. 2006 Jul;43(1):36-41.
- Matthews CE, Jurj AL, Shu XO, Li HL, Yang G,
Li Q, Gao YT, Zheng W. Influence of exercise, walking, cycling, and overall
nonexercise physical activity on mortality in Chinese women 50. Am.J.Epidemiol.
2007 Jun 15;165(12):1343-50.
- Schooling CM, Lam TH, Li ZB, Ho SY, Chan WM,
Ho KS, Tham MK, Cowling BJ, Leung GM. Obesity, physical activity, and mortality
in a prospective chinese elderly cohort
64. Arch.Intern.Med. 2006 Jul
24;166(14):1498-504.
- Manson JE, Greenland P, LaCroix AZ, Stefanick
ML, Mouton CP, Oberman A, Perri MG, Sheps DS, Pettinger MB, Siscovick DS.
Walking compared with vigorous exercise for the prevention of cardiovascular
events in women 184. N.Engl.J.Med. 2002 Sep 5;347(10):716-25.
- Folsom AR, Arnett DK, Hutchinson RG, Liao F,
Clegg LX, Cooper LS. Physical activity and incidence of coronary heart disease
in middle-aged women and men 162. Med.Sci.Sports Exerc. 1997
Jul;29(7):901-9.
- Noda H, Iso H, Toyoshima H, Date C, Yamamoto
A, Kikuchi S, Koizumi A, Kondo T, Watanabe Y, Wada Y, et al. Walking and sports
participation and mortality from coronary heart disease and stroke 188.
J.Am.Coll.Cardiol. 2005 Nov 1;46(9):1761-7.
- Skinner JS, Jaskolski A, Jaskolska A, Krasnoff
J, Gagnon J, Leon AS, Rao DC, Wilmore JH, Bouchard C. Age, sex, race, initial
fitness, and response to training: the HERITAGE Family Study. J.Appl.Physiol
2001 May;90(5):1770-6.
- McTiernan A, Kooperberg C, White E, Wilcox S,
Coates R, ms-Campbell LL, Woods N, Ockene J. Recreational physical activity and
the risk of breast cancer in postmenopausal women: the Women's Health
Initiative Cohort Study 19. JAMA 2003 Sep 10;290(10):1331-6.
- Bernstein L, Patel AV, Ursin G,
Sullivan-Halley J, Press MF, Deapen D, Berlin JA, Daling JR, McDonald JA,
Norman SA, et al. Lifetime recreational exercise activity and breast cancer
risk among black women and white women 65. J.Natl.Cancer Inst. 2005 Nov
16;97(22):1671-9.
- Slattery ML, Edwards S, Murtaugh MA, Sweeney
C, Herrick J, Byers T, Giuliano AR, Baumgartner KB. Physical activity and
breast cancer risk among women in the southwestern United States 66.
Ann.Epidemiol. 2007 May;17(5):342-53.
- Adams-Campbell LL, Rosenberg L, Rao RS, Palmer
JR. Strenuous physical activity and breast cancer risk in African-American
women 41. J.Natl.Med.Assoc. 2001 Jul;93(7-8):267-75.
- Gilliland FD, Li YF, Baumgartner K, Crumley D,
Samet JM. Physical activity and breast cancer risk in hispanic and non-hispanic
white women 44. Am.J.Epidemiol. 2001 Sep 1;154(5):442-50.
- Yang D, Bernstein L, Wu AH. Physical activity
and breast cancer risk among Asian-American women in Los Angeles: a
case-control study 51. Cancer 2003 May 15;97(10):2565-75.
- Barcenas CH, Wilkinson AV, Strom SS, Cao Y,
Saunders KC, Mahabir S, Hernandez-Valero MA, Forman MR, Spitz MR, Bondy ML.
Birthplace, years of residence in the United States, and obesity among
Mexican-American adults 8. Obesity.(Silver.Spring) 2007 Apr;15(4):1043-52.
- Ghosh A, Das Chaudhuri AB. Explaining body
composition by some covariate factors among the elderly Bengalee Hindu women of
Calcutta, India 45. J.Nutr.Health Aging 2005 Nov;9(6):403-6.
- Slattery ML, Sweeney C, Edwards S, Herrick J,
Murtaugh M, Baumgartner K, Guiliano A, Byers T. Physical activity patterns and
obesity in Hispanic and non-Hispanic white women 121. Med.Sci.Sports Exerc.
2006 Jan;38(1):33-41.
- Hornbuckle LM, Bassett DR, Jr., Thompson DL.
Pedometer-determined walking and body composition variables in African-American
women 54. Med.Sci.Sports Exerc. 2005 Jun;37(6):1069-74.
- Mack KA, Anderson L, Galuska D, Zablotsky D,
Holtzman D, Ahluwalia I. Health and sociodemographic factors associated with
body weight and weight objectives for women: 2000 behavioral risk factor
surveillance system 86. J.Womens Health (Larchmt.) 2004 Nov;13(9):1019-32.
- Kruger HS, Venter CS, Vorster HH, Margetts BM.
Physical inactivity is the major determinant of obesity in black women in the
North West Province, South Africa: the THUSA study. Transition and Health
During Urbanisation of South Africa 72. Nutrition 2002 May;18(5):422-7.
- Hui SSC, Thomas N, Tomlinson B. Relationship
between physical activity, fitness and CHD risk factors in middle-age Chinese
161. J.Phys.Act.Health 2005;2(3):307-23.
- Sternfeld B, Wang H, Quesenberry CP, Jr.,
Abrams B, Everson-Rose SA, Greendale GA, Matthews KA, Torrens JI, Sowers M.
Physical activity and changes in weight and waist circumference in midlife
women: findings from the Study of Women's Health Across the Nation 126.
Am.J.Epidemiol. 2004 Nov 1;160(9):912-22.
- Fitzgerald SJ, Kriska AM, Pereira MA, De
Court. Associations among physical activity, television watching, and obesity
in adult Pima Indians 38. Med.Sci.Sports Exerc. 1997 Jul;29(7):910-5.
- Forrest KY, Bunker CH, Kriska AM, Ukoli FA,
Huston SL, Markovic N. Physical activity and cardiovascular risk factors in a
developing population 43. Med.Sci.Sports Exerc. 2001 Sep;33(9):1598-604.
- Yu TY, Pei YC, Lau YC, Chen CK, Hsu HC, Wong
AM. Comparison of the effects of swimming and Tai Chi Chuan on body fat
composition in elderly people 157. Chang Gung.Med.J. 2007
Mar;30(2):128-34.
- Crane PB, Wallace DC. Cardiovascular risks and
physical activity in middle-aged and elderly African American women 18.
J.Cardiovasc.Nurs. 2007 Jul;22(4):297-303.
- Lee KJ, Inoue M, Otani T, Iwasaki M, Sasazuki
S, Tsugane S. Physical activity and risk of colorectal cancer in Japanese men
and women: the Japan Public Health Center-based prospective study 82. Cancer
Causes Control 2007 Mar;18(2):199-209.
- Iwane M, Arita M, Tomimoto S, Satani O,
Matsumoto M, Miyashita K, Nishio I. Walking 10,000 steps/day or more reduces
blood pressure and sympathetic nerve activity in mild essential hypertension
59. Hypertens.Res. 2000 Nov;23(6):573-80.
- Witmer JM, Hensel MR, Holck PS, Ammerman AS,
Will JC. Heart disease prevention for Alaska Native women: a review of pilot
study findings 151. J.Womens Health (Larchmt.) 2004 Jun;13(5):569-78.
- Wilmore JH, Despres JP, Stanforth PR, Mandel
S, Rice T, Gagnon J, Leon AS, Rao D, Skinner JS, Bouchard C. Alterations in
body weight and composition consequent to 20 wk of endurance training: the
HERITAGE Family Study 149. Am.J.Clin.Nutr. 1999 Sep;70(3):346-52.
- Ishikawa K, Ohta T, Zhang J, Hashimoto S,
Tanaka H. Influence of age and gender on exercise training-induced blood
pressure reduction in systemic hypertension 58. Am.J.Cardiol. 1999 Jul
15;84(2):192-6.
- Lara A, Yancey AK, Tapia-Conye R, Flores Y,
Kuri-Morales P, Mistry R, Subirats E, McCarthy WJ. Pausa para tu Salud:
reduction of weight and waistlines by integrating exercise breaks into
workplace organizational routine 80. Prev.Chronic.Dis. 2008 Jan;5(1):A12.
- Tsuzuku S, Kajioka T, Endo H, Abbott RD, Curb
JD, Yano K. Favorable effects of non-instrumental resistance training on fat
distribution and metabolic profiles in healthy elderly people 135.
Eur.J.Appl.Physiol 2007 Mar;99(5):549-55.
- Byrne NM, Weinsier RL, Hunter GR, Desmond R,
Patterson MA, Darnell BE, Zuckerman PA. Influence of distribution of lean body
mass on resting metabolic rate after weight loss and weight regain: comparison
of responses in white and black women 12. Am.J.Clin.Nutr. 2003
Jun;77(6):1368-73.
- Irwin ML, Ainsworth BE, Mayer-Davis EJ, Addy
CL, Pate RR, Durstine JL. Physical activity and the metabolic syndrome in a
tri-ethnic sample of women 7. Obes.Res. 2002 Oct;10(10):1030-7.
- Ford ES, Kohl HW, III, Mokdad AH, Ajani UA.
Sedentary behavior, physical activity, and the metabolic syndrome among U.S.
adults 22. Obes.Res. 2005 Mar;13(3):608-14.
- Carnethon MR, Gidding SS, Nehgme R, Sidney S,
Jacobs DR, Jr., Liu K. Cardiorespiratory fitness in young adulthood and the
development of cardiovascular disease risk factors 41. JAMA 2003 Dec
17;290(23):3092-100.
- Weinstein AR, Sesso HD, Lee IM, Cook NR,
Manson JE, Buring JE, Gaziano JM. Relationship of physical activity vs body
mass index with type 2 diabetes in women 186. JAMA 2004 Sep
8;292(10):1188-94.
- Hu FB, Stampfer MJ, Solomon C, Liu S, Colditz
GA, Speizer FE, Willett WC, Manson JE. Physical activity and risk for
cardiovascular events in diabetic women 150. Ann.Intern.Med. 2001 Jan
16;134(2):96-105.
- Hu FB, Li TY, Colditz GA, Willett WC, Manson
JE. Television watching and other sedentary behaviors in relation to risk of
obesity and type 2 diabetes mellitus in women 151. JAMA 2003 Apr
9;289(14):1785-91.
- Hsia J, Wu L, Allen C, Oberman A, Lawson WE,
Torrens J, Safford M, Limacher MC, Howard BV. Physical activity and diabetes
risk in postmenopausal women 148. Am.J.Prev.Med. 2005 Jan;28(1):19-25.
- Knowler WC, Barrett-Connor E, Fowler SE,
Hamman RF, Lachin JM, Walker EA, Nathan DM. Reduction in the incidence of type
2 diabetes with lifestyle intervention or metformin 154. N.Engl.J.Med. 2002 Feb
7;346(6):393-403.
- Orchard TJ, Temprosa M, Goldberg R, Haffner S,
Ratner R, Marcovina S, Fowler S. The effect of metformin and intensive
lifestyle intervention on the metabolic syndrome: the Diabetes Prevention
Program randomized trial 164. Ann.Intern.Med. 2005 Apr 19;142(8):611-9.
- Britton A, McKee M, Black N, McPherson K,
Sanderson C, Bain C. Threats to applicability of randomised trials: exclusions
and selective participation. J.Health Serv.Res.Policy 1999
Apr;4(2):112-21.
top of page
Note: Documents in PDF format require the
Adobe Acrobat Reader®.
If you experience problems with PDF documents, please
download the latest version of the Reader®.
Continue to H. Research Recommendations
Back to G10. Adverse Events
Back to Physical Activity Guidelines Advisory
Committee Report
|
|