 |

In addition to watching a loved one undergo difficult treatments, families of children with cancer must deal with disruption of normal life, travel to treatment centers, arranging childcare, finances, and other challenges. The cumulative effects can have serious consequences for quality of life during treatment and after it ends.
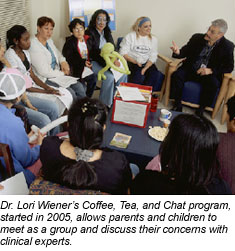
"We realize now that in order to provide our pediatric patients with the services that they need, we have to see these children in the context of their families and their communities, and integrate each of these dimensions so they can return home with the support, tools, and coping strategies to survive cancer," explains Dr. Lori Wiener, head of the Psychosocial Section and coordinator of the Psychosocial Support and Research Program in NCI's Pediatric Oncology Branch.
She hopes that some of the research under way through her program, which has developed resources and practice models for treatment centers and families, can help people who are looking for ways to handle these challenges. Psychosocial support within the pediatric oncology program begins with social workers who contact patients as soon as they are recommended for a clinical trial at NIH, and who maintain contact with these families one-on-one throughout the course of their treatment.
 Many of these families stay at the Children's Inn at NIH, where support programs compliment services at the Clinical Center, including play, art, and music therapy; support groups and workshops; psychiatric consultation; counseling; camp programs; school programs and vocational testing; pain and palliative care services; spiritual ministry; and bereavement programs, among others.
Many of these families stay at the Children's Inn at NIH, where support programs compliment services at the Clinical Center, including play, art, and music therapy; support groups and workshops; psychiatric consultation; counseling; camp programs; school programs and vocational testing; pain and palliative care services; spiritual ministry; and bereavement programs, among others.
Psychotherapy for children in clinical trials also addresses fear and anxiety due to being far from home, new treatments, and invasive procedures. "It's horrifying to see a panic-stricken child trying to deal with an impending bone marrow transplant, or any kind of needle stick," says Dr. Jimmie Holland, a psychiatrist and Wayne Chapman Chair in Psychiatric Oncology at Memorial Sloan-Kettering Cancer Center, which has the country's largest training program in this field. "The experience upsets anyone who comes near it. But if you can help these children and their family members prepare for the rigors of treatment, using behavioral techniques that are proven, you can give patients and their families a sense of control and diminish panic in these situations."
Drs. Holland and Wiener have worked together on resources that outline psychosocial issues and solutions that are so critical to successful cancer care, some of which are based on a report commissioned by the Institute of Medicine, Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs, as well as a reference book that will soon be available from the American Psychosocial Oncology Society, Quick Reference for Pediatric Oncology Clinicians: The Psychiatric and Psychological Dimensions of Pediatric Cancer Symptom Management, for which Dr. Wiener is lead editor.
Dr. Wiener's program has also developed tools, including several for the siblings of cancer patients: a workbook titled This is MY World, another titled Brothers and Sisters - We're in This Together, and a customizable board game available later this year.
After children complete their cancer treatment and leave the Clinical Center, they are connected with the support network in their local communities. But their relationship with staff at NIH can last a lifetime. Even when a child dies, their family members are considered cancer survivors, Dr. Wiener explains, and she is in touch with them each year on the anniversary of their loss. "There's a sense that we've lived through this life-altering experience together," Dr. Wiener says, "and a special connection often arises between families and the health care providers who traveled that journey with them."
|