Introduction
Moles
Dysplastic Nevi
Melanoma
Prevention of Melanoma
Early Detection of Melanoma
Other Booklets
Pictures of Ordinary Moles and Dysplastic Nevi
Pictures of Melanoma
National Cancer Institute Information Resources
Introduction
The National Cancer Institute (NCI) has written this booklet (NIH Publication No. 99-3133) to help you
learn more about common moles* and unusual
ones called dysplastic nevi
or atypical moles. This booklet shows what moles look like and explains how
they may be related to melanoma, a
type of skin cancer. It describes the
signs of melanoma and explains how you can check your skin for moles that might
be cancerous. It also explains why and how you can protect your skin. Other
NCI booklets about skin cancer and cancer prevention are listed in the
"Other Booklets" section.
Cancer research has led to real progress against cancer -- better survival and
an improved quality of life. Through research, our knowledge about moles and
cancers of the skin keeps increasing. We are finding new ways to prevent,
detect, and treat cancer. The
Cancer Information Service and the other
sources of NCI information listed under
"National Cancer Institute Information Resources"
can provide the latest, most accurate information about moles, dysplastic nevi,
and cancer. Publications mentioned in this booklet and others are available
from the Cancer Information Service at 1-800-4-CANCER. Many NCI publications
are also available on the Internet at the Web sites listed in the
"National Cancer Institute Information Resources"
section at the end of this booklet.
*Words that may be new to readers are printed in italics.
Definitions of these and other terms related to moles and melanoma are listed in
the Dictionary. For some words, a
"sounds-like" spelling is also given.
 Back to Top Back to Top
Moles
Moles are growths on the skin. Doctors call moles nevi (one mole is a
nevus). These growths occur when cells
in the skin, called melanocytes,
grow in a cluster with tissue surrounding them. Moles are usually pink, tan,
brown, or flesh-colored. Melanocytes are also spread evenly throughout the
skin and produce the pigment that
gives skin its natural color. When skin is exposed to the sun, melanocytes
produce more pigment, causing the skin to tan, or darken.
Moles are very common. Most people have between 10 and 40 moles. A person
may develop new moles from time to time, usually until about age 40. Moles can
be flat or raised. They are usually round or oval and no larger than a pencil
eraser. Many moles begin as a small, flat spot and slowly become larger in
diameter and raised. Over many years, they may flatten again, become
flesh-colored, and go away.
 Back to Top Back to Top
Dysplastic Nevi
About one out of every ten people has at least one unusual (or atypical)
mole that looks different from an ordinary mole. The medical term for these
unusual moles is dysplastic nevi. The
"Pictures of Ordinary Moles and Dysplastic Nevi"
section shows the differences between ordinary moles and dysplastic nevi.
Doctors believe that dysplastic nevi are more likely than ordinary moles to
develop into a type of skin cancer called melanoma. Because of this, moles
should be checked regularly by a doctor or nurse specialist, especially if they
look unusual; grow larger; or change in color, outline, or in any other way.
 Back to Top Back to Top
Melanoma
Melanoma is a type of skin cancer -- one of the most serious types because
advanced melanomas have the ability to spread to other parts of the body.
(Melanoma can also develop in the eye, called intraocular melanoma, or rarely
in other parts of the body where pigment cells are found. The
CIS can provide
information about the diagnosis and treatment of intraocular melanoma.)
Melanoma begins when melanocytes (pigment cells) gradually become more abnormal
and divide without control or order. These cells can invade and destroy the
normal cells around them. The abnormal cells form a growth of
malignant tissue (a cancerous
tumor) on the surface of the skin.
Melanoma can begin either in an existing mole or as a new growth on the skin.
The "Pictures of Melanoma" section shows
examples of melanoma. A doctor or nurse specialist can tell whether an
abnormal-looking mole should be closely watched or should be removed and
checked for melanoma cells. The purpose of routine skin exams is to identify
and follow abnormal moles.
The removal of the entire mole or a sample of tissue for examination under a
microscope is called a biopsy. If
possible, it is best to remove moles by an
excisional biopsy, rather
than a shave biopsy.
If the biopsy results in a diagnosis of melanoma, the patient and the doctor
should work together to make treatment decisions. In many cases, melanoma can
be cured by minimal surgery if the tumor is discovered when it is thin (before
it has grown downward from the skin surface) and before the cancer cells have
begun to spread to other places in the body. However, if melanoma is not found
early, the cancer cells can spread through the bloodstream and
lymphatic system to form
tumors in other parts of the body. Melanoma is much harder to control when it
has spread. The spread of cancer is called
metastasis.
Doctors and scientists believe that it is possible to prevent many melanomas
and to detect most others early, when the disease is more likely to be cured
with minimal surgery. In the past several decades, an increasing percentage of
melanomas have been diagnosed at very early stages, when they are quite thin
and unlikely to have spread. Learning about prevention and early detection,
while important for everyone, is especially important for people who have an
increased risk for melanoma. People who are at an increased risk include those
who have dysplastic nevi or a very large number of ordinary moles.
Risk Factors for Melanoma
Family history of melanoma Dysplastic nevi History of melanoma Weakened immune system Many ordinary moles (more than 50) Ultraviolet (UV) radiation Severe, blistering sunburns Freckles Fair skin
|
The National Cancer Institute booklet
What You Need To Know About™ Melanoma
has more information about
risk factors for this disease.
It is important to remember that not everyone who has dysplastic nevi or
other risk factors for melanoma gets the disease. In fact, most do not. Also,
about half the people who develop melanoma do not have dysplastic nevi, and
they may not have any other known risk factor for the disease. At this time,
no one can explain why one person gets melanoma while another does not.
Research has shown that sun exposure, especially excessive exposure that leads
to bad, blistering sunburns, is an important and avoidable risk factor.
Scientists are continuing their studies of risk factors for melanoma.
 Back to Top Back to Top
Prevention of Melanoma
The number of people in the world who develop melanoma is increasing each
year. In the United States, the number has more than doubled in the past 20
years. Experts believe that much of the worldwide increase in melanoma is
related to an increase in the amount of time people spend in the sun.
Ultraviolet (UV) radiation
from the sun and from sunlamps and tanning booths damages the skin and can lead
to melanoma and other types of skin cancer. (Two types of ultraviolet
radiation -- UVA and UVB -- are explained in the
"Dictionary" section.) Everyone, especially
those who have dysplastic nevi or other risk factors, should try to reduce the
risk of developing melanoma by protecting the skin from UV radiation. The
intensity of UV radiation from the sun is greatest in the summer, particularly
during midday hours. A simple rule is to avoid the sun or protect your skin
whenever your shadow is shorter than you are.
People who work or play in the sun should wear protective clothing, such as
a hat and long sleeves. Also, lotion, cream, or gel that contains
sunscreen can help protect the skin.
Many doctors believe sunscreens may help prevent melanoma, especially those that
reflect, absorb, and/or scatter both types of ultraviolet radiation. Sunscreens
are rated in strength according to a
sun protection factor
(SPF). The higher the SPF, the more
sunburn protection is provided. Sunscreens with an SPF value of 2 to 11
provide minimal protection against sunburns. Sunscreens with an SPF of 12 to
29 provide moderate protection. Those with an SPF of 30 or higher provide high
protection against sunburn. Sunglasses that have UV-absorbing lenses should
also be worn. The label should specify that the lenses block at least 99
percent of UVA and UVB radiation.
 Back to Top Back to Top
Early Detection of Melanoma
Because melanoma usually begins on the surface of the skin, it often can be
detected at an early stage with a total skin examination by a trained health
care worker. Checking the skin regularly for any signs of the disease
increases the chance of finding melanoma early. A monthly skin self-exam is
very important for people who have any of the known risk factors, but doing
skin self-exams routinely is a good idea for everyone.
Here is how to do a skin self-exam:
After a bath or shower, stand in front of a full-length mirror in a well-lighted room. Use a hand-held mirror to look at hard-to-see areas. Begin with the face and scalp and work downward, checking the head, neck, shoulders, back, chest, and so on. Be sure to check the front, back, and sides of the arms and legs. Also, check the groin, the palms, the fingernails, the soles of the feet, the toenails, and the area between the toes. Be sure to check the hard-to-see areas of the body, such as the scalp and neck. A friend or relative may be able to help inspect these areas. Use a comb or a blow dryer to help move hair so you can see the scalp and neck better. Be aware of where your moles are and how they look. By checking your skin regularly, you will become familiar with what your moles look like. Look for any signs of change, particularly a new black mole or a change in outline, shape, size, color (especially a new black area), or feel of an existing mole. Also, note any new, unusual, or "ugly-looking" moles. If your doctor has taken photos of your skin, compare these pictures with the way your skin looks on self-examination. Check moles carefully during times of hormone changes, such as adolescence, pregnancy, and menopause. As hormone levels change, moles may change. It may be helpful to record the dates of your skin exams and to write notes about the way your skin looks. If you find anything unusual, see your doctor right away. Remember, the earlier a melanoma is found, the better the chance for a cure.
In addition to doing routine skin self-exams, people should have their skin
checked regularly by a doctor or nurse specialist. A doctor can do a skin exam
during visits for regular checkups. People who think they have dysplastic nevi
should point them out to the doctor. It is also important to tell the doctor
about any new, changing, or "ugly-looking" moles.
Sometimes it is necessary to see a specialist. A
dermatologist (skin doctor) is
likely to have the most training in diseases of the skin. Some plastic
surgeons, general surgeons,
oncologists, internists, and
family doctors also have a special interest and training in moles and melanoma.
Melanoma may run in families, and members of these families are at high risk
for the disease. In some of these families, certain members also have a large
number (usually over 100) of
dysplastic nevi.
These people have an especially high risk of developing melanoma. When two or
more family members develop melanoma, it is important for all of the patients'
close relatives (parents, brothers, sisters, and children above the age of 10)
to see a doctor and be examined carefully for dysplastic nevi or any signs of
melanoma. The doctor can then decide how often each person needs to be seen.
(Doctors may recommend that these family members have checkups every 6 months.)
Anyone who has a large number of dysplastic nevi also should be examined regularly.
A doctor may want to watch a slightly abnormal mole closely to see whether it
changes over time. Pictures taken at one visit may be compared with the
appearance of the mole at the next visit. Sometimes a doctor decides that a
mole should be removed so that the tissue can be examined under a microscope.
The removal of a mole, called a biopsy, is usually done in the doctor's office
using a local anesthetic. It
generally takes only a few minutes. The patient may require stitches, and a
small scar will remain after healing. A
pathologist examines the tissue
under a microscope to see whether the melanocytes are normal, dysplastic, or
cancerous.
Because most moles, including most dysplastic nevi, do not develop into
melanoma, removing all of them is not necessary. A doctor can recommend when
and when not to remove moles. Usually, only moles that look like melanoma,
those that change, or those that are both new and look abnormal need to be
removed.
 Back to Top Back to Top
Other Booklets
The National Cancer Institute booklets listed below and others are available from the Cancer Information Service by calling 1-800-4-CANCER.
 Back to Top Back to Top
Pictures of Ordinary Moles and Dysplastic Nevi
|
|
Ordinary Moles
|
Dysplastic Nevi
|
|
Color
|
Evenly tan or brown; all typical moles on one person tend to look similar.
|
Mixture of tan, brown, and red/pink. A person's moles often look quite different from
one another.
|
|
|
|

|
|
Shape
|
Round or oval, with a distinct edge that separates the mole from the rest of the skin.
|
Have irregular, sometimes notched edges. May fade into the skin around it. The flat portion
of the mole may be level with the skin.
|
|
|
|

|
|
Surface
|
Begin as flat, smooth spots on skin (1a); may become raised (1b) and form a smooth
bump (1c).
|
May have a smooth, slightly scaly, or rough, irregular, "pebbly" appearance.
|
|
|
|

|
|
Size
|
Usually less than 5 millimeters (about 1/4 inch) across (size of a pencil eraser).
|
Often larger than 5 millimeters (about 1/4 inch) across and sometimes larger
than 10 millimeters (about 1/2 inch).
|
|
|

|

|
|
Number
|
Between 10 and 40 typical moles may be present on an adult's body.
|
May be present in large numbers (more than 100 on the same person). However, some
people have only a few dysplastic nevi.
|
|
|
|

|
|
Location
|
Usually found above the waist on sun-exposed surfaces of the body. Scalp, breasts,
and buttocks rarely have normal moles.
|
May occur anywhere on the body but most frequently on the back and areas exposed to
the sun. May also appear below the waist and on the scalp, breasts, and buttocks.
|
|
|

|
|
 Back to Top Back to Top
Pictures of Melanoma
|
Large size
|
Most melanomas are at least 5 millimeters
(about 1/4 inch) across when they are found; many
are much larger. An unusually large mole may be melanoma.
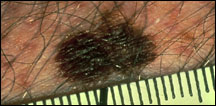
|
|
Many colors
|
A mixture of tan, brown, white, pink, red, gray, blue, and especially
black in a mole suggests melanoma.

|
|
Irregular border
|
If a mole has an edge that is irregular or notched, it may be melanoma.

|
|
Abnormal surface
|
If a mole is scaly, flaky, oozing, or bleeding, has an open sore that does not heal, or has a
hard lump in it, it may be melanoma.

|
|
Unusual sensation
|
If a mole itches or is painful or tender, melanoma may be present.

|
|
Abnormal skin around mole
|
If color from the mole spreads into the skin around it or if this skin becomes red or loses
its color (becomes white or gray), melanoma may be present.

|
 Back to Top Back to Top
National Cancer Institute Information Resources
You may want more information for yourself, your family, and your doctor. The following National Cancer Institute (NCI) services are available to help you.
Cancer Information Service (CIS)
Provides accurate, up-to-date information on cancer to patients and their families, health professionals, and the general public. Information specialists translate the latest scientific information into understandable language and respond in English, Spanish, or on TTY equipment.
Toll-free: 1-800-4-CANCER (1-800-422-6237)
TTY (for deaf and hard of hearing callers): 1-800-332-8615
http://www.cancer.gov
NCI's Web site contains comprehensive information about cancer causes and prevention, screening and diagnosis, treatment and survivorship; clinical trials; statistics; funding, training, and employment opportunities; and the Institute and its programs.
See the complete index of What You Need To Know About™ Cancer publications.
 Back to Top Back to Top
|
