|
Childhood Cancer Survivors Research
The Childhood Cancer Survivor Study (CCSS) is an NCI-funded research project that includes a cohort of more than 20,000 people who were diagnosed with cancer as children between 1970 and 1986, and who survived at least 5 years. Because of the study design and the large number of people enrolled, CCSS has allowed researchers to discern long-term disease- and treatment-related outcomes with unprecedented clarity.
"As more children become survivors and live for decades, we have more opportunities to learn about the long-term effects of cancer and its treatments," says Dr. Barry Anderson, senior investigator in NCI's Cancer Therapy Evaluation Program and scientific liaison to the study.
CCSS operates through a network of 26 pediatric oncology research centers and has enrolled survivors with a spectrum of cancer diagnoses and treatments, characterizing their specific treatment parameters and updating this information with self-reports, tissue specimens, and follow-up questionnaires every 2 years that detail their health and psychosocial status. More than 4,000 siblings are also included as controls.
"The data we gather is a scientific resource, not only for members of CCSS, but for any investigator in the research community," says Dr. Les Robison, chair of the Department of Epidemiology and Cancer Control at St. Jude Children's Research Hospital in Memphis. More than 60 studies have been published to date, including many that were used to develop the current long-term follow-up guidelines from the Children's Oncology Group.
Clinical researchers are often faced with designing treatments that balance cure rates and side effects, both immediate and long term. Another challenge is to develop effective interventions for survivors after treatment, such as teaching preventive behaviors or recommending heightened screening. The research published by CCSS helps physicians to sort through these issues and to guide evidence-based practice.
For example, a major CCSS study on chronic illness appeared in the October 12 New England Journal of Medicine, showing that childhood cancer survivors are eight times more likely to develop a severe or life-threatening chronic health condition. "The impact of some of these health problems can be reduced with periodic survivor-focused follow-up," said Dr. Kevin Oeffinger, lead author of the study and a researcher at Memorial Sloan-Kettering Cancer Center in New York City.
Plans are under way to recruit another 14,500 cancer survivors to CCSS, particularly from among minority populations. These people, who were diagnosed between 1987 and 1999, will reveal the long-term effects of cancer therapies including agents like ifosfamide, dose-intensive treatment regimens, and the reduction in radiotherapy for Hodgkin disease and childhood acute lymphoblastic leukemia.
 Promoting Health and Well-Being after Cancer
Promoting Health and Well-Being after Cancer
Many cancer survivors attempt to make lifestyle changes such as exercising, quitting smoking, and improving their diet to provide a better quality of life after treatment, as well as reduce the likelihood of future illness. However, reviews of the existing literature and data collected from the National Health Interview Survey show that these kinds of changes are difficult to initiate and to maintain in the long run.
"Despite evidence of potential benefits, lifestyle changes are difficult for everybody, not just cancer survivors," said Dr. Linda Nebeling, chief of the Health Promotion Research Branch in DCCPS. "You may have an episode in your life such as a cancer diagnosis that makes it very personal, but you still have to work through the processes to help overcome triggers that make you more likely to fall into old habits."
Colleen Doyle, lead author of the ACS guidelines, Nutrition and Physical Activity During and After Cancer Treatment: An American Cancer Society Guide for Informed Choices, sees a reworking of our environment as a necessary adjunct to education in this area. "As with the general population, education and increased awareness will only go so far in promoting healthier living - even among people who may be highly motivated to make changes - because our environments are huge barriers to all of us living well. The long-term solution is going to have to include changing environments and social norms, as we've seen with tobacco control." ACS recently addressed some of these issues in a Recommendation for Community Action that focused on promoting healthy changes in schools, worksites, and communities, published within their 2006 Prevention Guidelines.
NCI is currently funding extensive research into the mechanics of what exercise, diet, and the combination of the two can do to help the body physiologically, explained Dr. Nebeling. "Are there ways to combine diet and exercise to improve the resistance of your body to developing a recurrence?"
One example of this is the Transdisciplinary Research on Energetics and Cancer (TREC) initiative, launched in 2005. TREC research centers are studying how the combined effects of obesity, poor diet, and lack of physical activity increase cancer risk. "A lot of the biological work is very relevant to cancer survivors," said Dr. Ann McTiernan, a TREC researcher from Fred Hutchinson Cancer Research Center in Seattle. "Evidence is increasing that keeping weight in normal ranges and increasing physical activity are associated with improved survival and reduced recurrence in patients with several types of cancer including breast, colon, and prostate."
In addition to the large-scale projects, she explained, TREC investigators also are beginning several survivor-specific research studies, such as looking at yoga as a method to improve weight control and quality of life in breast cancer survivors, and ways to increase exercise in children who are cancer survivors and their families.
Cancer Affects Daily Life and Well-Being
Most cancer survivors look forward to resuming normal life after treatment, but burgeoning evidence suggests that for many the experience doesn't end with their last oncology visit. Survivors often deal with psychosocial issues that affect their school and work performance, finances, sexual health, and self-identity. The range and severity of these issues can vary based on the type of cancer a person has, their disease management, their age when illness occurs, and their personal characteristics.
Many times cancer survivors suffer emotional fallout from their disease. Dr. Gary Deimling, a researcher at Case Western Reserve University in Cleveland, notes that nearly half of all long-term survivors continue to have worries about recurrence or new cancers, or that symptoms they experience may be cancer related. There is also some concern that these worries are relatively strong predictors of depression.
Despite these obstacles, a positive attitude and self-identification can help survivors cope with the after-effects of cancer. Dr. Deimling notes that an individual's self-identification as a cancer survivor is associated with that person's level of optimism and self-esteem, and could promote better mental health outcomes.
Cancer survivors sometimes experience problems with sexual health, including a loss of desire for sex, impaired fertility, erectile dysfunction in men, and painful sexual intercourse in women. According to an article published in Hematology last year by Dr. Leslie Schover of the University of Texas M.D. Anderson Cancer Center, cancer treatment can "damage reproductive health in ways that are profound and often permanent. [But] interventions that prevent or reverse these problems will greatly improve the quality of life of our patients."
Dr. Schover recently listed a number of evidence-based interventions to address some of these effects - including cryopreservation of sperm, eggs, and embryos, as well as conservative surgical and hormone treatments - as a participating author of the American Society of Clinical Oncology's fertility preservation guidelines, which were published June 20 in the Journal of Clinical Oncology.
Often, cancer survivors face increased costs for medical care and personal expenses after cancer, such as those associated with transportation to and from treatment or lost days of work. Furthermore, dietary needs and lingering side effects such as fatigue, neuropathy, or cognitive changes may affect their performance at work or school.
"Work is particularly important for many cancer survivors because it provides income, health insurance, purpose in life, and even social relationships," said Dr. Carolyn Messner of CancerCare, a nonprofit organization that helps cancer survivors by providing free counseling, telephone and online support groups, education programs, and financial assistance.
"Returning to work represents a return to the routine that survivors were used to before they had cancer. Work reminds them that they can get back to normal activities." Also, Dr. Messner adds, survivors should pace themselves when returning to work and may require a workplace accommodation to manage long-term effects of cancer.
"The important message here is that cancer is often a life-altering and potentially traumatic event," explains Dr. Julia Rowland, director of NCI's OCS, "but we can make recovery easier by educating survivors on what to expect, giving them ways to manage stress, teaching them effective behavioral and coping skills, and directing them to resources that can help them not merely survive, but hopefully thrive after treatment."
Caregivers of Cancer Patients Are Also Survivors
There is mounting research cataloging the impact that caring for loved ones with cancer - by parents, spouses, siblings, even close friends - can have. It might come as no surprise, for example, that parents of children who have undergone cancer treatment can show psychological problems similar to those seen in people who have survived natural disasters or war. Moreover, studies have revealed that such posttraumatic stress symptoms can be, and often are, worse than those seen in the child, and that they can last for months and even years after treatment is over.
Although it's a relatively new area, explained OCS Director Dr. Julia Rowland, research on cancer caregivers has matured to the point where it is now testing interventions to help individuals, and often families, deal with the physical, psychological, and financial effects of providing care.
The studies are attempting to "test interventions that promote communication between survivors and their caregivers, and enable caregivers to feel competent in or informed about the care that they deliver," Dr. Rowland said. "Others are attempting to enhance caregivers' coping skills and attention to personal health and well-being."
At The Children's Hospital of Philadelphia, for instance, Dr. Anne Kazak, who directs its Center for Pediatric Traumatic Stress, is testing a family-based program to help both children and parents better handle the psychological trauma that cancer can inflict on families.
 "The program model integrates cognitive behavior therapy and family therapy," Dr. Kazak explained. "It asks family members, within the context of a group of families, to discuss their beliefs about what's happened to them, and then uses behavioral approaches to help them cope better and feel better."
"The program model integrates cognitive behavior therapy and family therapy," Dr. Kazak explained. "It asks family members, within the context of a group of families, to discuss their beliefs about what's happened to them, and then uses behavioral approaches to help them cope better and feel better."
Among Dr. Laurel Northouse's caregiver-related projects at the University of Michigan in Ann Arbor is a similar family-based intervention for survivors and caregivers that strictly involves single-family encounters. The program has been used successfully to help women with recurrent breast cancer and their caregivers cope with emotional challenges, and Dr. Northouse and her colleagues just completed a study using it to help men who have been treated for prostate cancer and their spouses.
Among Survivors, Cancer Sometimes Returns
With recent advances in the treatment and early detection of cancer, there is a growing need to monitor the risk of developing new malignancies among long-term survivors of cancer.
"We know that the burden of second cancers is not borne equally among cancer survivors," says Dr. Joseph F. Fraumeni, Jr., director of NCI's Division of Cancer Epidemiology and Genetics (DCEG). "But there are patterns of incidence that make it possible to tailor prevention strategies, including long-term surveillance for early diagnosis and treatment of subsequent tumors."
Among research elucidating these patterns of new malignancies is that of Drs. Lois Travis and Mitchell Gail of DCEG, who developed a model for estimating a woman's risk of developing breast cancer after treatment with large-field chest radiotherapy for Hodgkin lymphoma, showing that cumulative risk increases with age at end of follow-up, time since diagnosis, and radiation dose.
Similarly, women who are treated for breast cancer with higher dose chemotherapy have been shown to be at increased risk for developing leukemia, and comprehensive postmastectomy radiotherapy has been linked to excess lung cancers, according to research by the NCI-funded National Surgical Adjuvant Breast and Bowel Project. Researchers are now focusing on ways to identify which patients are most likely to benefit from chemotherapy or radiation, to avoid exposing women unnecessarily to these risks.
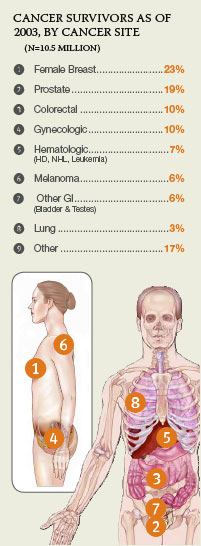
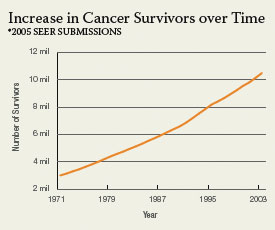
 While certain therapies, environmental exposures, and genetics can predispose people to developing cancer again, it's important to note that many second or multiple cancers in the adult survivor population are simply due to aging, says Dr. Julia Rowland, director of NCI's OCS. The most recent data from the Surveillance, Epidemiology, and End Results (SEER) program (2003) indicate that 16 percent of new diagnoses were among people who had already been treated for cancer, underscoring the importance of long-term surveillance and follow-up care among cancer survivors.
While certain therapies, environmental exposures, and genetics can predispose people to developing cancer again, it's important to note that many second or multiple cancers in the adult survivor population are simply due to aging, says Dr. Julia Rowland, director of NCI's OCS. The most recent data from the Surveillance, Epidemiology, and End Results (SEER) program (2003) indicate that 16 percent of new diagnoses were among people who had already been treated for cancer, underscoring the importance of long-term surveillance and follow-up care among cancer survivors.
A monograph on the risks of second cancers - reporting on those that have arisen among U.S. cancer survivors from 1973 to 2000 - will soon be available as an NIH publication and on the SEER Web site. More than 50 adult and 18 childhood tumors, including new data on some uncommon sites and individual histologic types, are included with comparison between SEER data and other studies, and discussion of potential risk factors and mechanisms.
|