Released: September 2007
Investigation of cases of HIV infection in healthcare personnel without identified risk factors is coordinated by the Centers for Disease Control and Prevention (CDC) and state health department staff. These investigations have been conducted since early in the AIDS epidemic, but it was not until 1991 that a standardized investigation protocol was developed and implemented by CDC. Since then, healthcare personnel with HIV/AIDS who are reported without any known risk for HIV infection are to be investigated by state and local health departments using this protocol. In addition, CDC has requested that health departments also investigate other reports (e.g., from physicians or from published sources of information) of healthcare personnel who may have occupationally acquired HIV infection even if they did not meet the criteria of the AIDS surveillance case definition and the state does not have formal requirements for HIV infection reporting.
Because of the voluntary nature of the reporting system, there may be some underreporting of cases. Documented cases of occupationally acquired HIV/AIDS are those in which HIV seroconversion is temporally related to an exposure to an HIV-positive source and in which the exposed worker has no nonoccupational risk factors for acquisition of HIV. Possible cases of occupationally acquired HIV/AIDS are those in which a worker is found to be HIV positive, has no nonoccupational risk factors for HIV/AIDS, and has opportunities for occupational exposure to blood, body fluids, or HIV-positive laboratory material. Although seroconversion after exposure was not documented for these personnel, occupational acquisition of their infection might have been possible.
Of those healthcare personnel for whom case investigations were completed from 1981-2006, 57 had documented seroconversion to HIV following occupational exposures (see table for occupations). The routes of exposure resulting in infection were: 48 percutaneous (puncture/cut injury); five, mucocutaneous (mucous membrane and/or skin); two, both percutaneous and mucocutaneous; and two were of unknown route. Forty-nine healthcare personnel were exposed to HIV-infected blood; three to concentrated virus in a laboratory; one to visibly bloody fluid; and four to an unspecified fluid. In addition, 140 possible cases of HIV infection or AIDS have occurred among healthcare personnel.
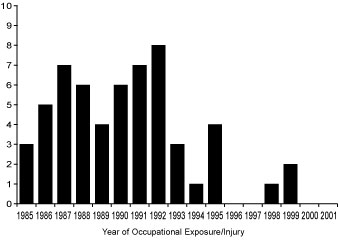
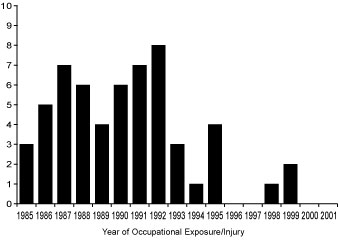
The most recent possible new case of occupationally acquired HIV/AIDS was reported to CDC in 2000; no new documented cases have been reported since that time, although several cases are in various stages of investigation. As yet, none can be classified as documented cases. The figure shows the number of exposures/injuries leading to documented transmission by year, from 1984-1999. There are usually delays between the exposure and the reporting of the case to CDC. The number of possible cases may decrease if individuals are reclassified when a nonoccupational risk is identified or may increase if new cases are reported.
More than 90% of healthcare personnel infected with HIV have nonoccupational risk factors for acquiring their infection.
Suspected cases of occupationally acquired HIV/AIDS may be reported to the
Division of Healthcare Quality Promotion at 800-893-0485.
| Healthcare Personnel with Documented and Possible Occupationally Acquired AIDS/HIV Infection, by Occupation, 1981-2006 |
| Occupation |
Documented |
Possible |
| Nurse |
24 |
35 |
| Laboratory worker, clinical |
16 |
17 |
| Physician, nonsurgical |
6 |
12 |
| Laboratory technician, nonclinical |
3 |
- |
| Housekeeper/maintenance worker |
2 |
13 |
| Technician, surgical |
2 |
2 |
| Embalmer/morgue technician |
1 |
2 |
| Health aide/attendant |
1 |
15 |
| Respiratory therapist |
1 |
2 |
| Technician, dialysis |
1 |
3 |
| Dental worker, including dentist |
- |
6 |
| Emergency medical technician/paramedic |
- |
12 |
| Physician, surgical |
- |
6 |
| Other technician/therapist |
- |
9 |
| Other healthcare occupation |
- |
6 |
| Total |
57 |
140 |
|
This graph is from the article by Do AN et al. Occupationally acquired HIV infection: national case surveillance data during 20 years of the HIV epidemic in the U.S. Infect Control Hosp Epidemiol 2003;24:86-96.