Zanzibar: Beyond Malaria Control
Malaria has declined to low levels in Zanzibar, and careful planning is now underway to prevent it from taking hold again. Indeed, Zanzibar is entering uncharted waters. PMI looks forward to learning valuable lessons from this next phase of malaria control and how it may be applicable in other settings where malaria transmission has been reduced.
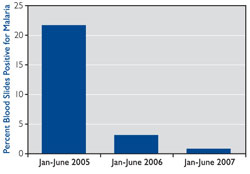
| Percentage of Blood Slides Positive for Malaria in Children Under Age 2, Zanzibar, 2005-2007 |
|
 |
|
| After long-lasting insecticide-treated bed nets (LLINs) were distributed in early 2006 and insecticide was sprayed on the inside of houses during 2006 – 2007, data gathered from health facility laboratory registers and pediatric wards showed a 95 percent reduction in malaria infections throughout Zanzibar for children under 2 years of age. A separate community survey in May 2007 found no malaria cases among pregnant and recently pregnant Zanzibari women. | |
With an integrated package of malaria interventions supported by multiple partners over the past five years, and with support from PMI during the past two years, Zanzibar – an archipelago that forms part of the United Republic of Tanzania – has made dramatic strides in controlling malaria. In fact, compared with five years ago, malaria is now rare.
However, this success is fragile due to several factors. On the Tanzania mainland, just 20 miles away from Zanzibar, the prevalence of malaria infection in residents remains high and travel between the two is very common. The species of mosquito that can transmit malaria still exists in Zanzibar, so ongoing vigilance is critical. To achieve the World Health Organization’s criteria for pre-elimination status (less than 1 case of confirmed malaria among 1,000 persons with fever), Zanzibar needs to reduce malaria transmission even further.
What Zanzibar does in the coming years will be the true measure of its success with malaria control. The strategies to maintain this success will also provide useful information for other countries as they reduce malaria transmission.
The Next Step: Detecting Malaria Epidemics
 |
||
| Staff from the Zanzibar Malaria Control Program (standing) and a clinical officer from a peripheral health facility discuss implementation of an early epidemic detection system. Source: Abdul-wahiyd Al-mafazy | ||
Zanzibar is now finalizing plans for a system to detect, confirm, respond to, and contain a malaria epidemic at the first sign of increased transmission.
An epidemic is easily defined: the unusual occurrence of infection or disease above what is normally expected. But this definition becomes more challenging to operationalize when the number of people with a particular disease has declined rapidly in a short period of time, as is true in Zanzibar.
In late November 2007, Zanzibar’s Malaria Control Program (ZMCP) and colleagues from PMI, Research Triangle International, the Mennonite Economic Development Associates, and Selcom Wireless (through a novel public-private partnership) drafted a preliminary plan for a malaria early detection system. After subsequent planning meetings with key stakeholders in Zanzibar, ZMCP implemented the system in 10 health facilities in April – May 2008. Eventually, all health facilities in Zanzibar will be expected to report to the system upon confirmation of malaria in a patient.
 |
|
| Source: Bob Wirtz, CDC | |
Zanzibar’s Plan for a Malaria Early Detection System: A Summary
Detection: Initially, 10 peripheral health facilities in Unguja and Pemba (the largest islands in Zanzibar) are participating in the system. The ability to diagnose malaria has been strengthened at these facilities, primarily via use of malaria rapid diagnostic tests. Using recent data from each facility, epidemic thresholds will be set for helping each health facility recognize when it has surpassed the threshold point.
Reporting: Using a cell phone, each health facility reports data on a weekly basis via a customized text messaging menu developed by Selcom Wireless, in collaboration with ZMCP. The malaria data are transmitted to a server, where they are processed and presented in two formats. First, a summary of each week’s surveillance data (for Unguja and Pemba separately) is sent via a single text message to the ZMCP program manager, district medical officers (DMOs), and other Ministry of Health authorities. Second, for easy viewing of malaria trends over time, the server automatically generates graphical images viewable on a secure Web site. Both ZMCP and district surveillance officers (DSOs) have access to the Web site. To facilitate reporting of consistent, accurate, and timely data, the sentinel health facilities are reporting only three indicators: total number of outpatient visits, number of laboratory-confirmed malaria cases, and number of persons tested for malaria that week.Confirmation: If increased numbers of laboratory-confirmed malaria cases are reported, representatives from the district health management team and ZMCP will visit the health facility within 24 hours after notification to rule out false alarms. An increase could be due to many factors, including human error. The representatives will obtain name, age, village, recent travel history, symptoms, and treatment for each case-patient and review laboratory records to help rule out technician errors as the “cause” of the epidemic. Households of the reported malaria case-patients will be visited within 24 hours, and each member of the household will be screened for malaria using rapid diagnostic tests, as will all residents of a sample of nearby homes. Data will be reviewed within three to four days after initiating the confirmation process. The DMO and ZMCP will issue a joint statement regarding their findings and their plan for containing the epidemic, if one is confirmed.
Response: A key step will be to rapidly make the community and health care system aware of a confirmed increase in malaria transmission. The DSO will notify all health facilities in the affected district and instruct them to heighten their index of suspicion for malaria. ZMCP will alert the DMOs in all surrounding districts to do the same. The main intervention will be provision of artemisinin-based combination therapy (ACT) to persons with fever (independent of malaria diagnosis) detected through house-to-house active case detection in communities where data indicate the epidemic is occurring. This strategy, known as mass fever treatment, aims to get treatment to probable malaria cases as quickly as possible to alleviate illness, avert death, and help contain the epidemic.
Integrated vector control must also be part of the initial response. A combination of indoor residual spraying (IRS) in the affected area and increased emphasis on use of insecticide-treated bed nets (ITNs) will be used. In Zanzibar, since ownership of ITNs is already high for the overall population (>60 percent), a rapid awareness campaign to reinforce nightly use of nets may serve as a very fast and effective epidemic control strategy.
 |
|
| Source: Bob Wirtz, CDC | |
Control: After the epidemic is suppressed, longer-term control methods will be implemented. Activities may include distribution of LLINs to increase overall population coverage, focal IRS of the affected communities, and assurances that ACTs are well stocked at all health facilities. Community campaigns to encourage residents to seek medical attention for fever episodes, especially if they have recently traveled to the Tanzania mainland, will also be an important strategy.
The Future
In Zanzibar, PMI is committed to strengthening local-, district-, and national-level capacities for the early detection and response to malaria epidemics. All three levels must be involved, know their roles in advance, and respond to possible epidemics using a pre-planned strategy. There is little doubt that such a system will eventually be called upon on Unguja or Pemba in the future.
Submitted by Peter McElroy, CDC-Tanzania and PMI Resident Technical Advisor